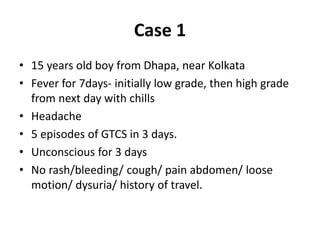
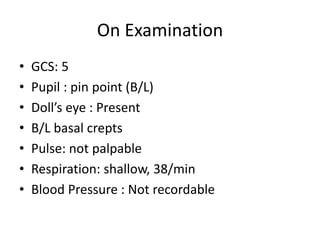
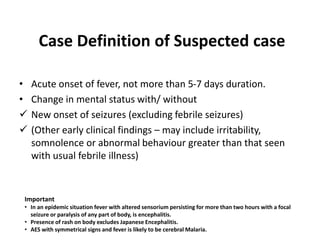
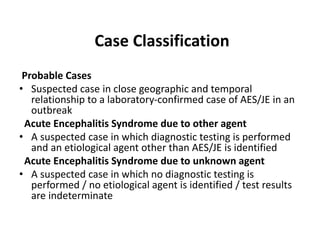
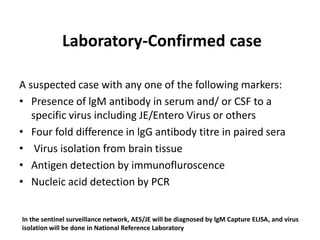
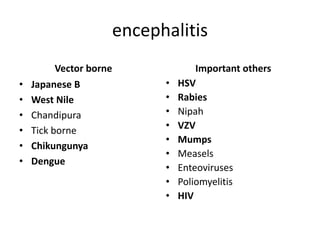
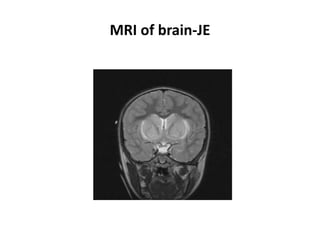
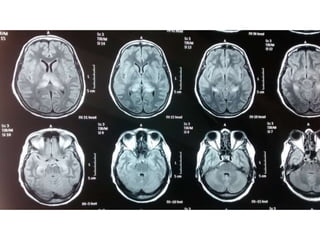
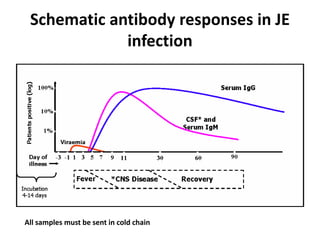
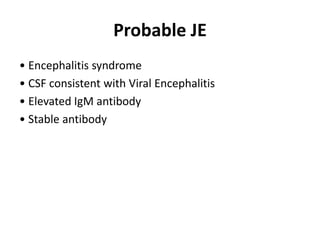
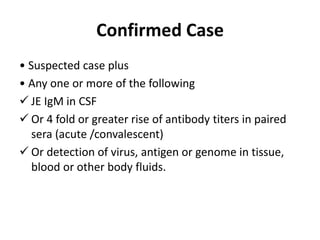
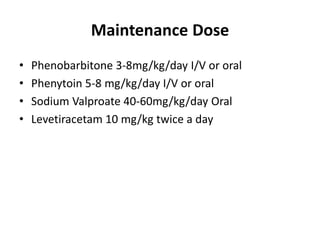
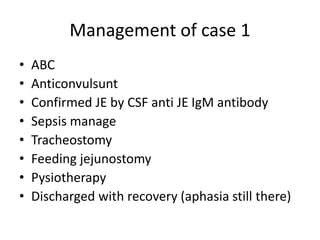
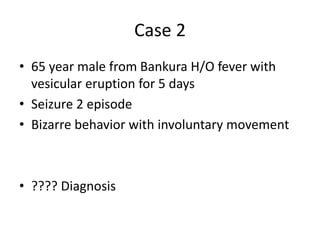
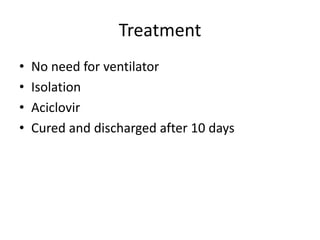
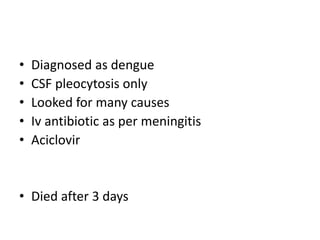
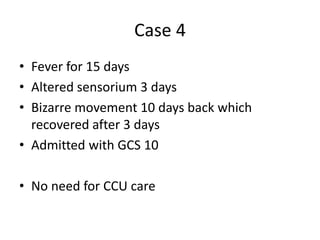
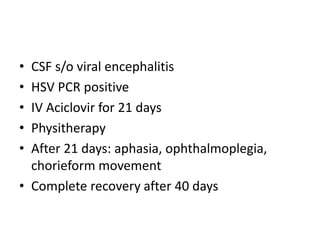
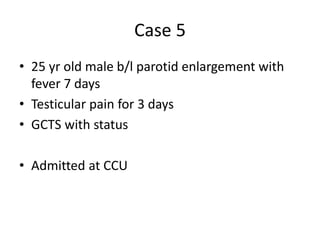
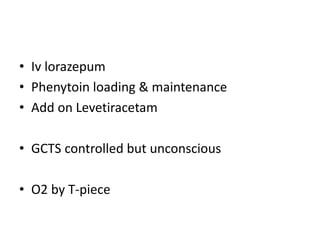
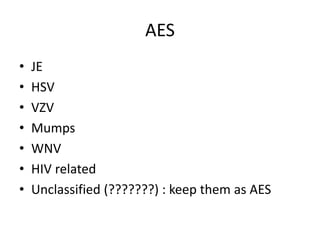
This document discusses several cases of acute encephalitis syndrome (AES) along with background information on AES etiologies and Japanese encephalitis (JE) epidemiology. Case 1 involves a 15-year-old boy with JE diagnosed by CSF IgM antibody testing who required ventilatory support and developed aphasia. Case 2 is a 65-year-old man with varicella zoster virus encephalitis diagnosed based on clinical presentation. Case 3 is a fatal case of dengue encephalitis diagnosed based on CSF findings and clinical course. Case 4 involved HSV encephalitis confirmed by PCR testing who recovered with acyclovir treatment. Case 5 involved mumps meningoencephalitis presenting with par