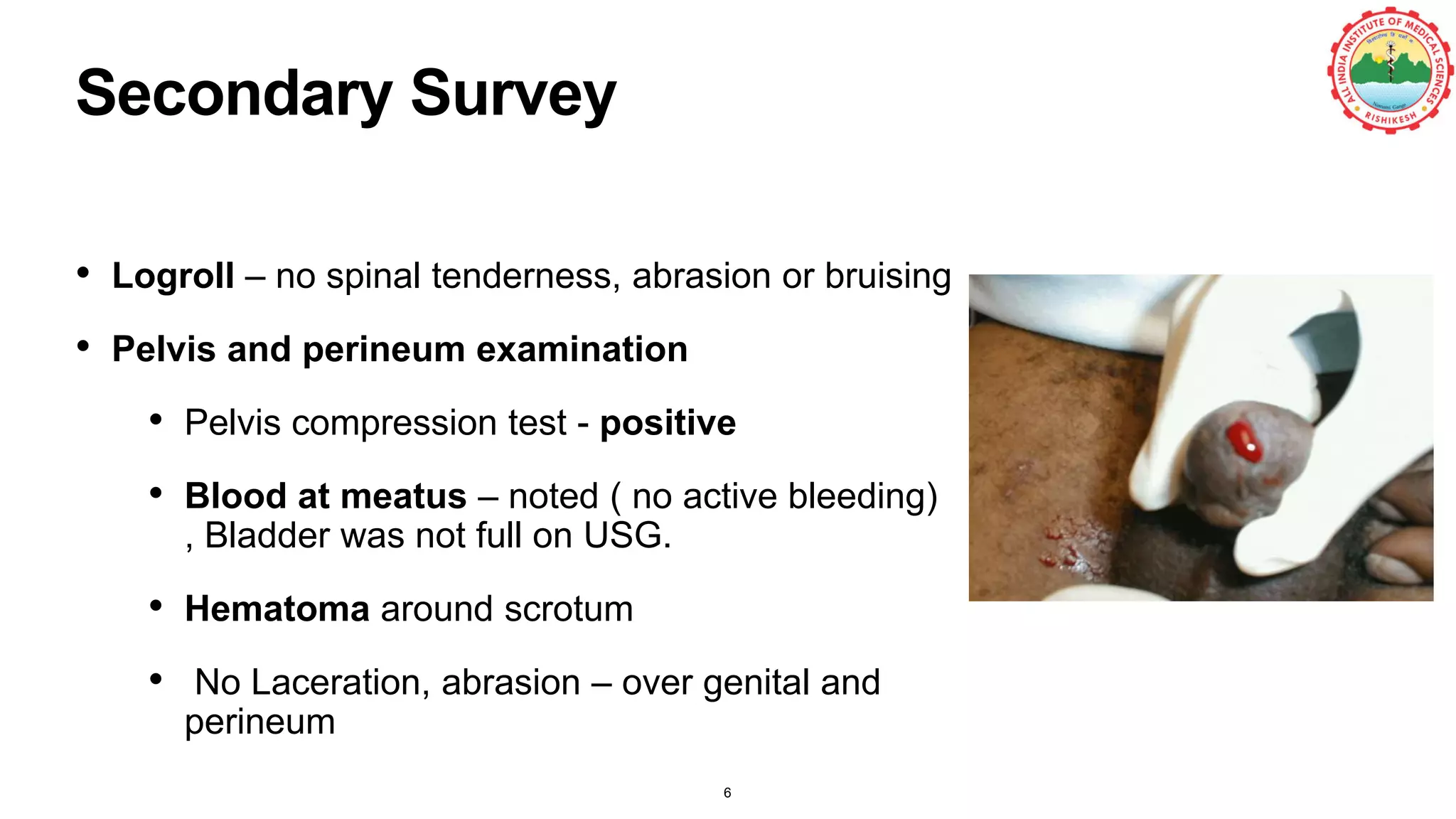
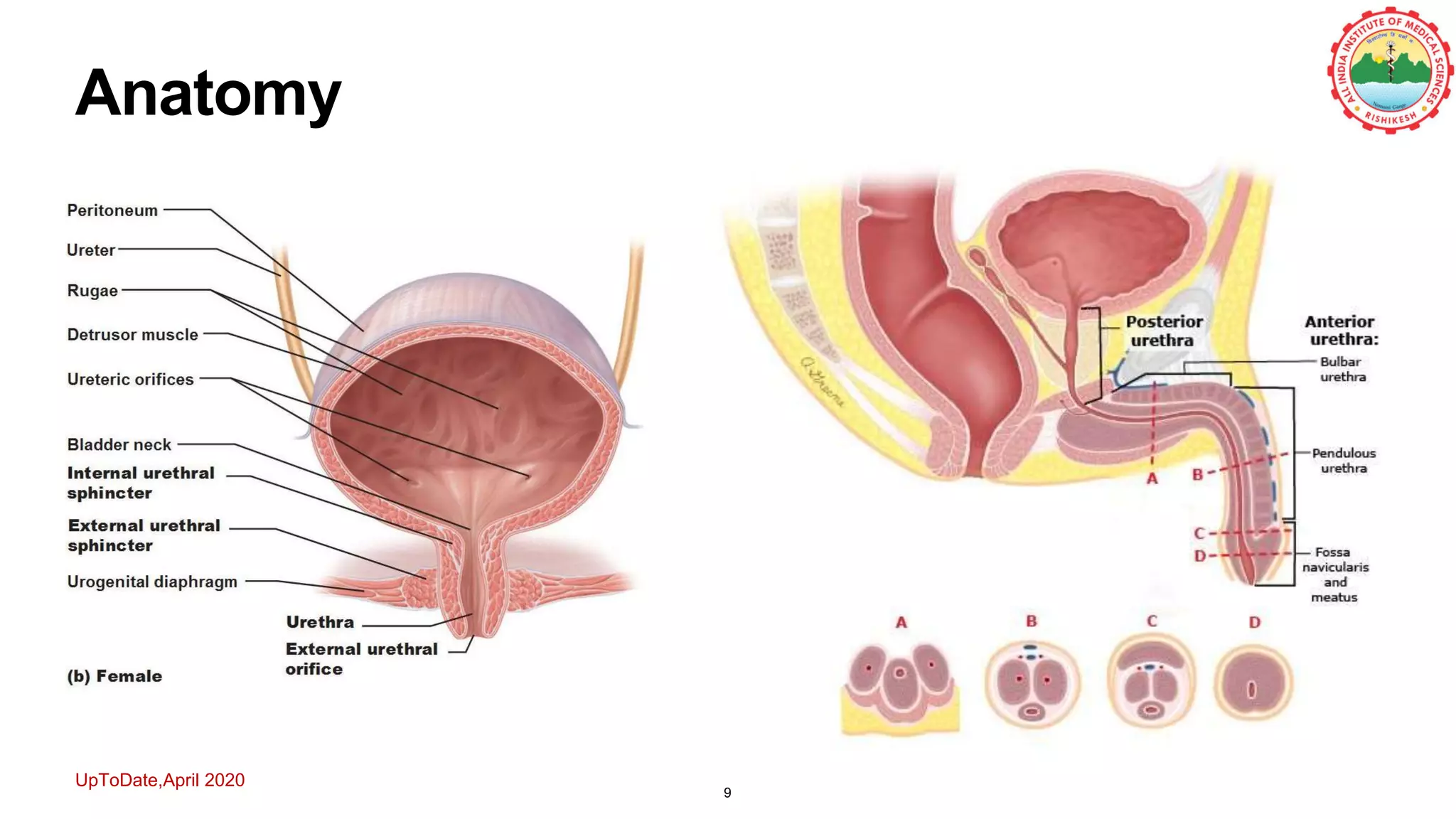
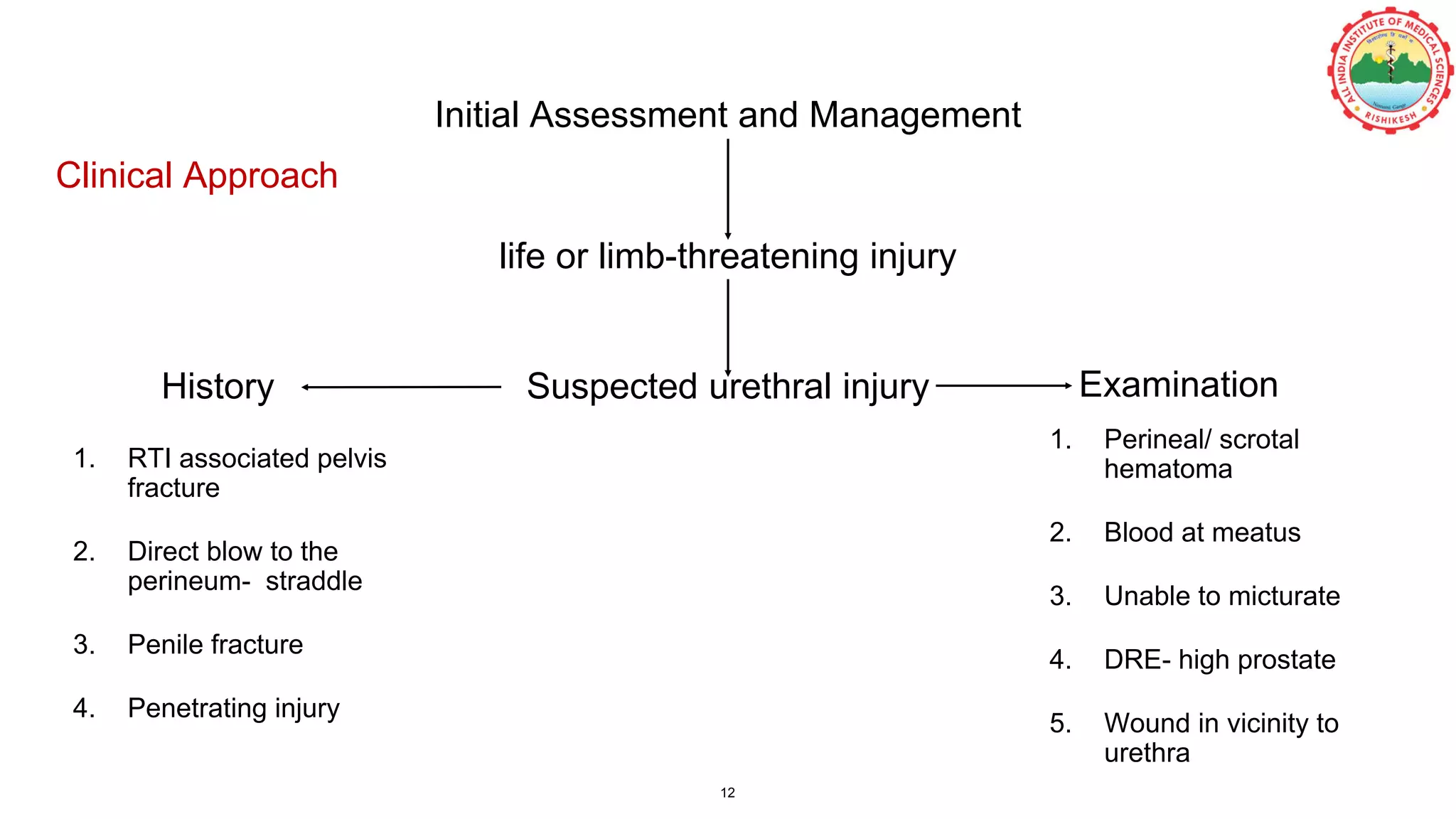
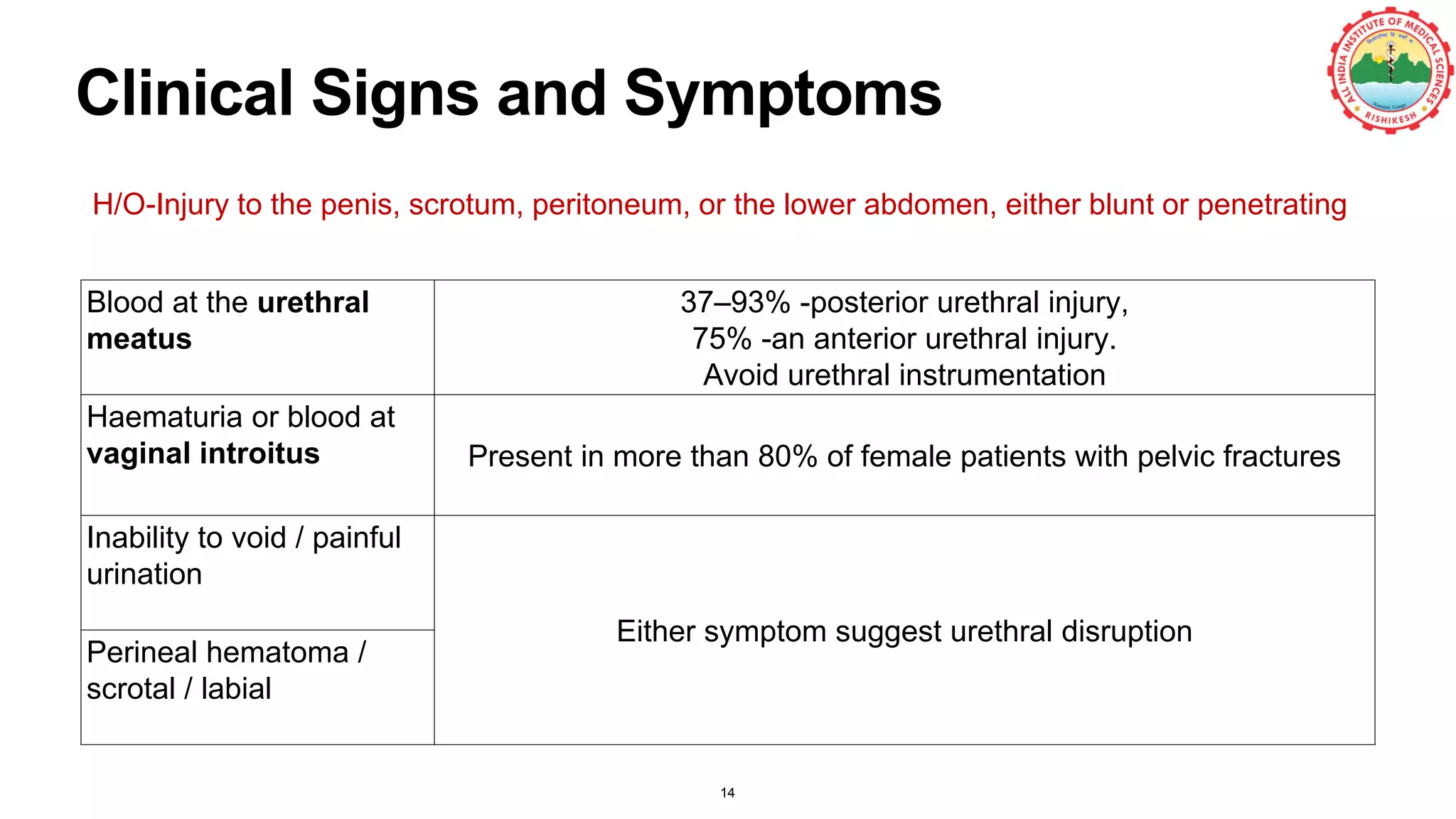
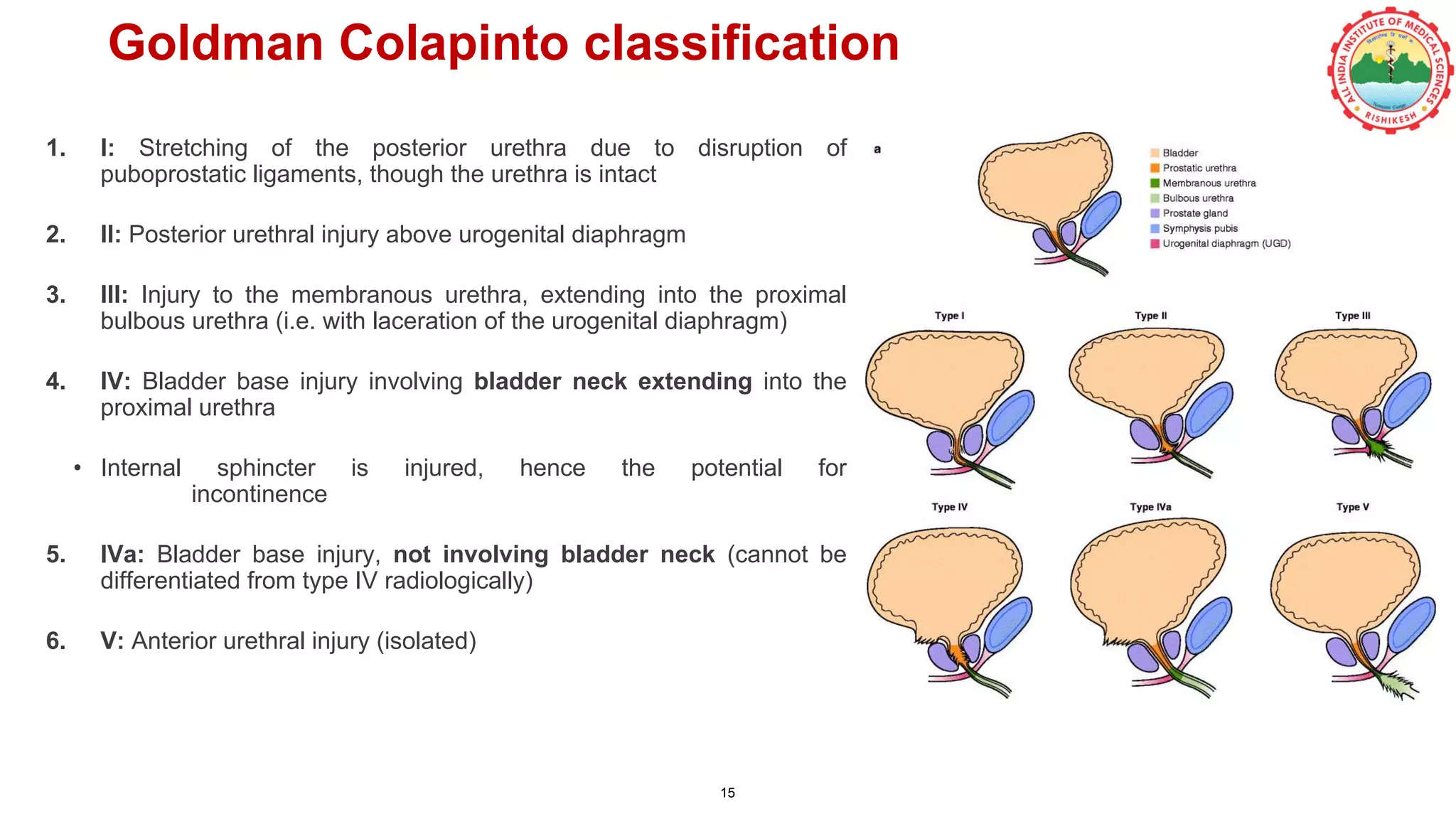
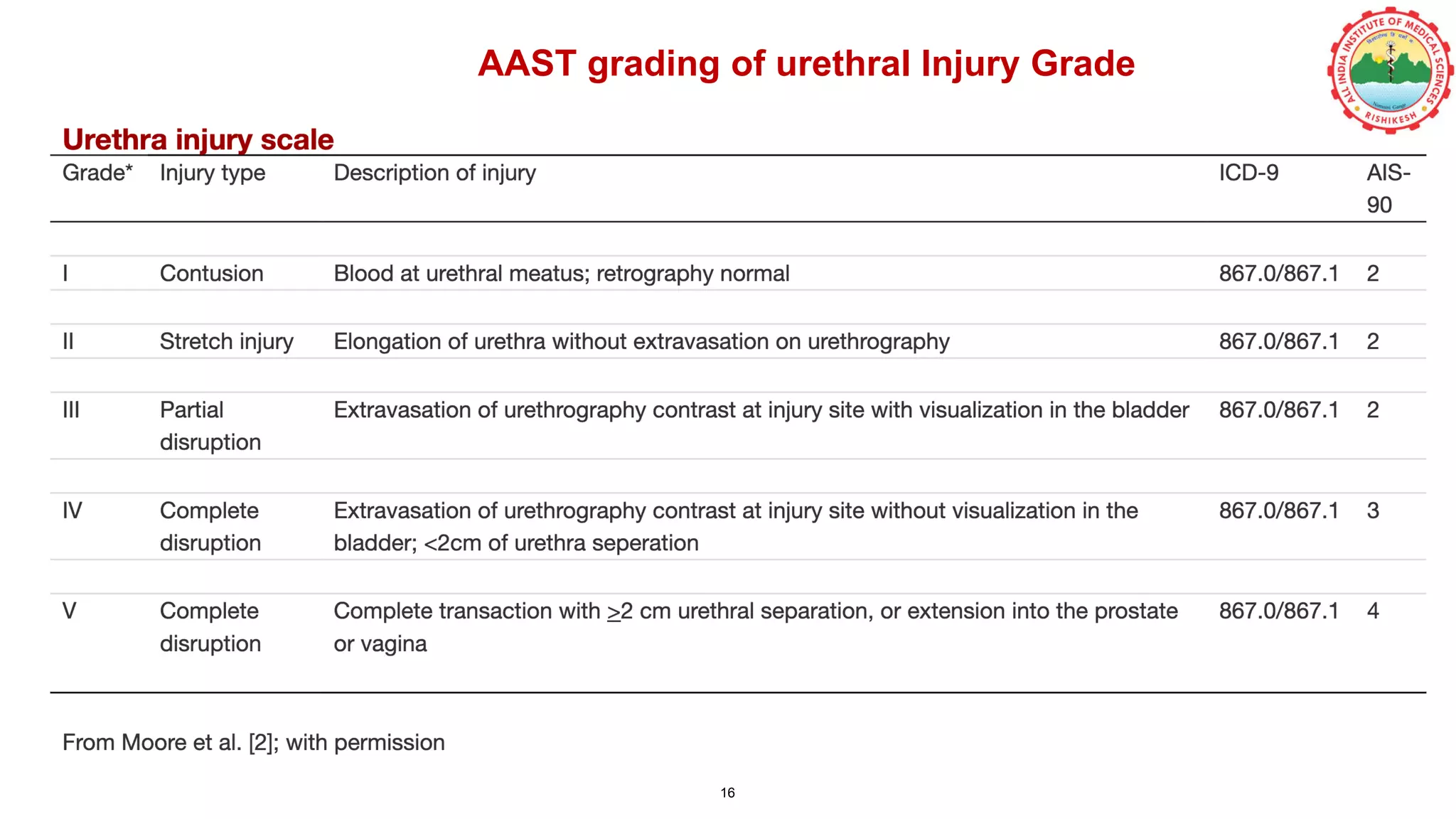
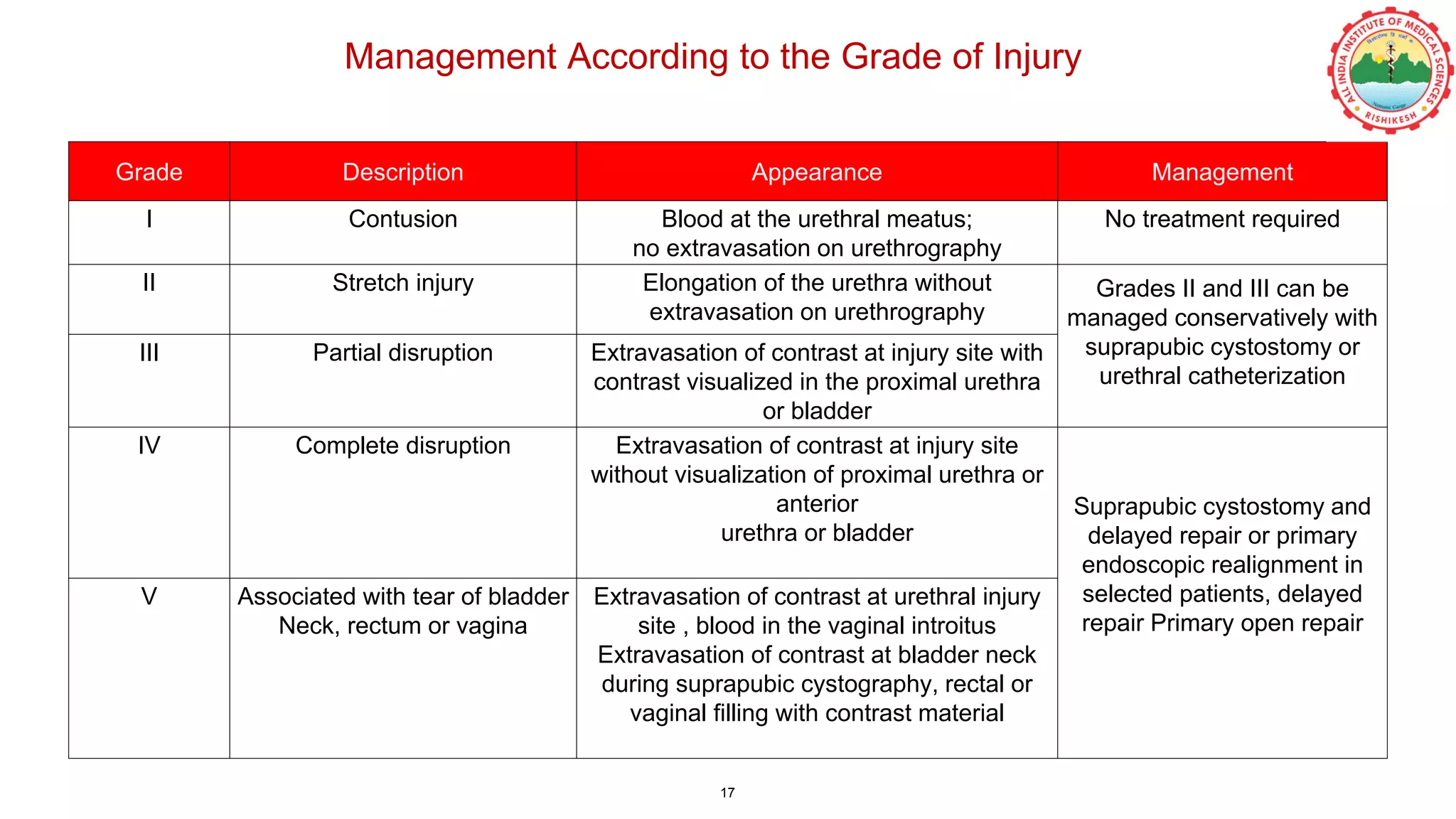
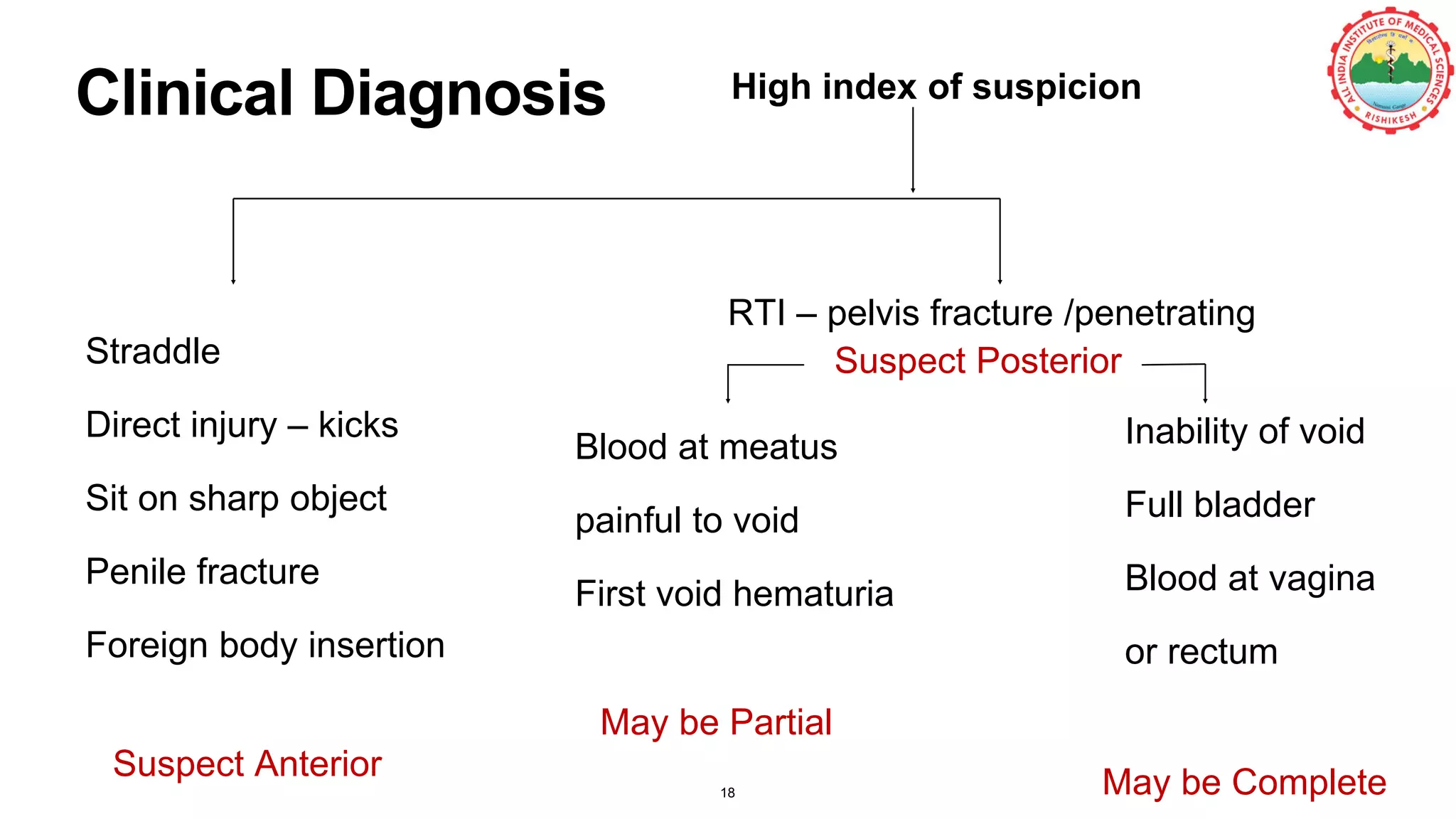
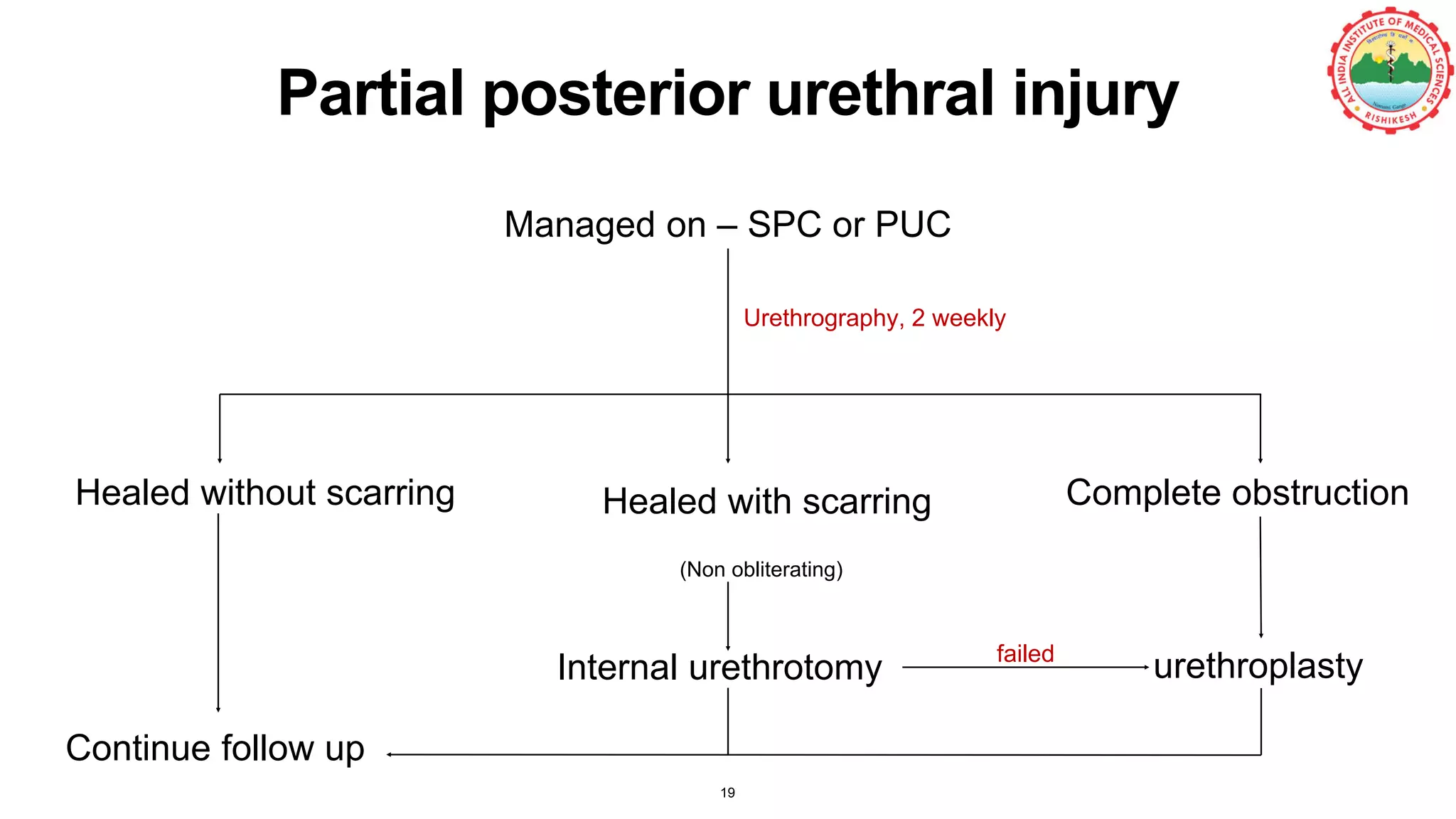
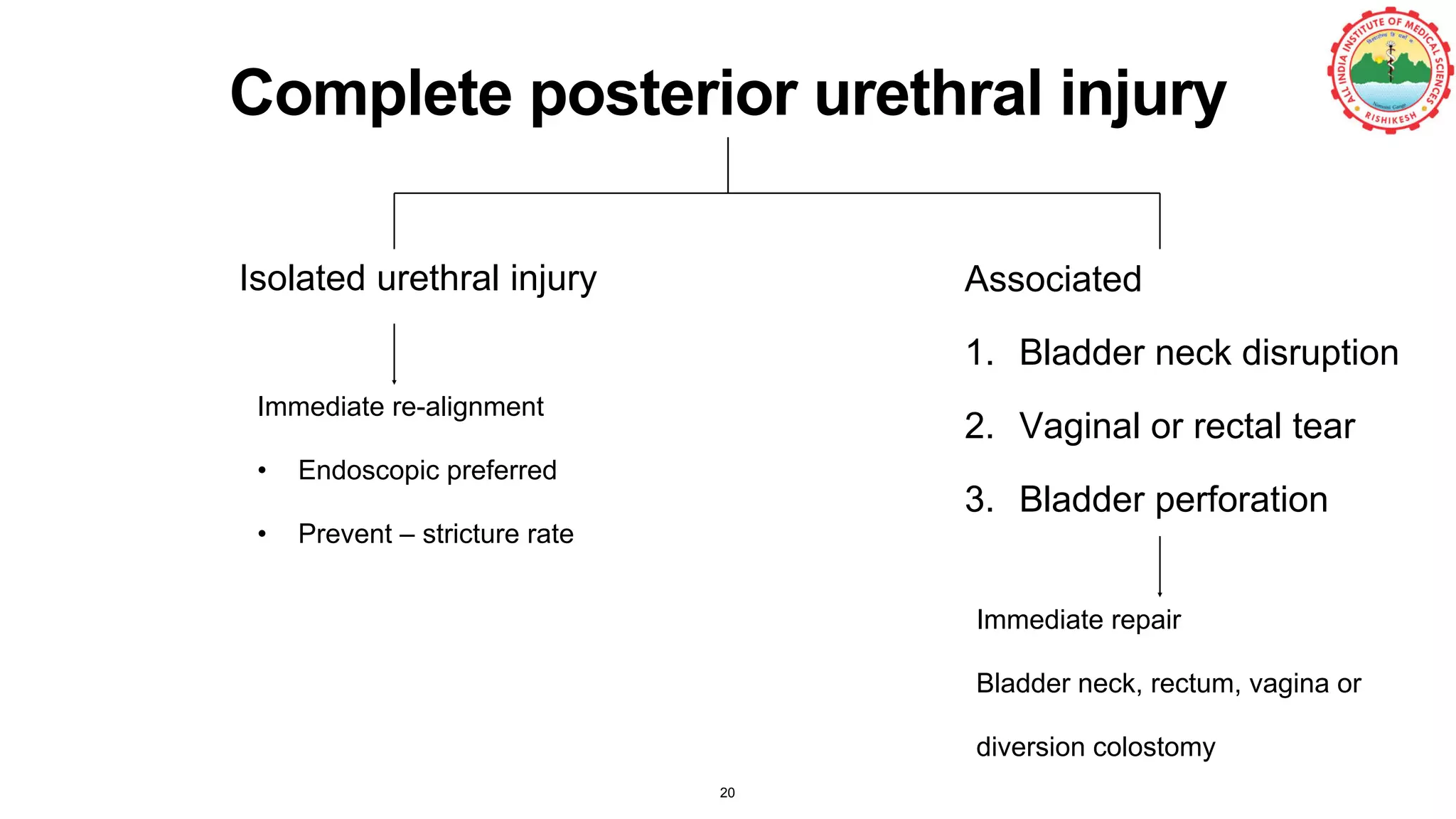
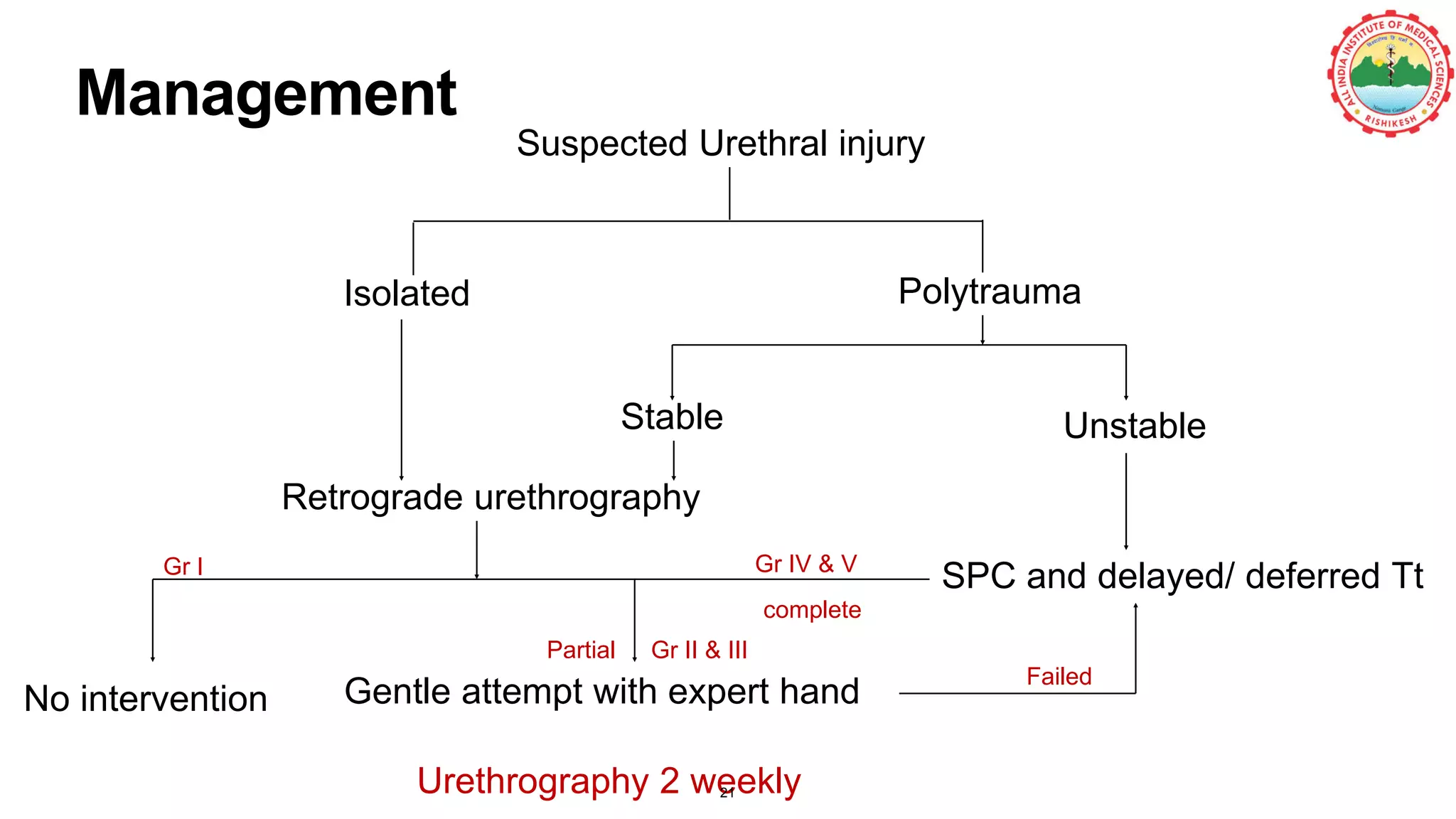
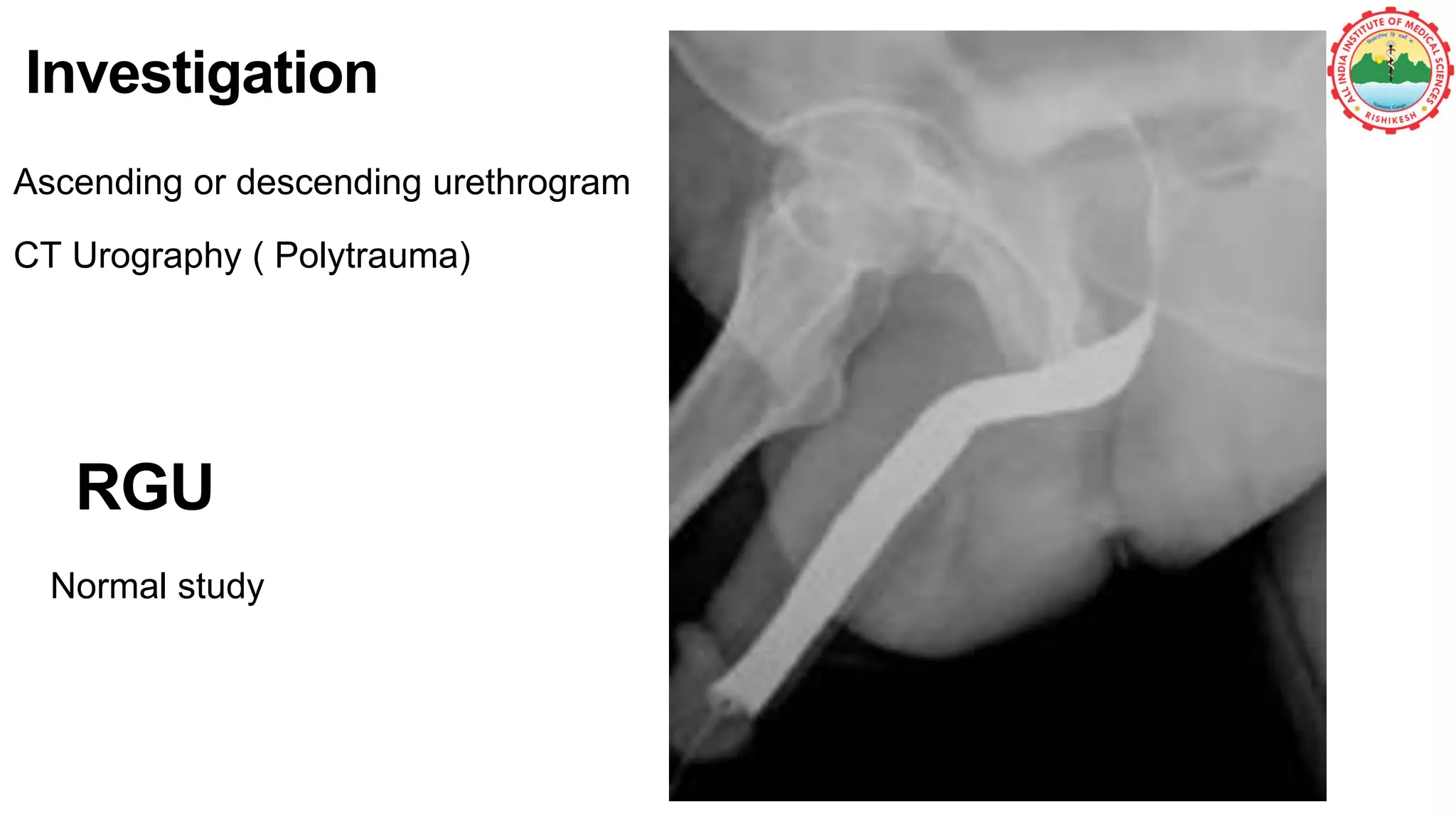
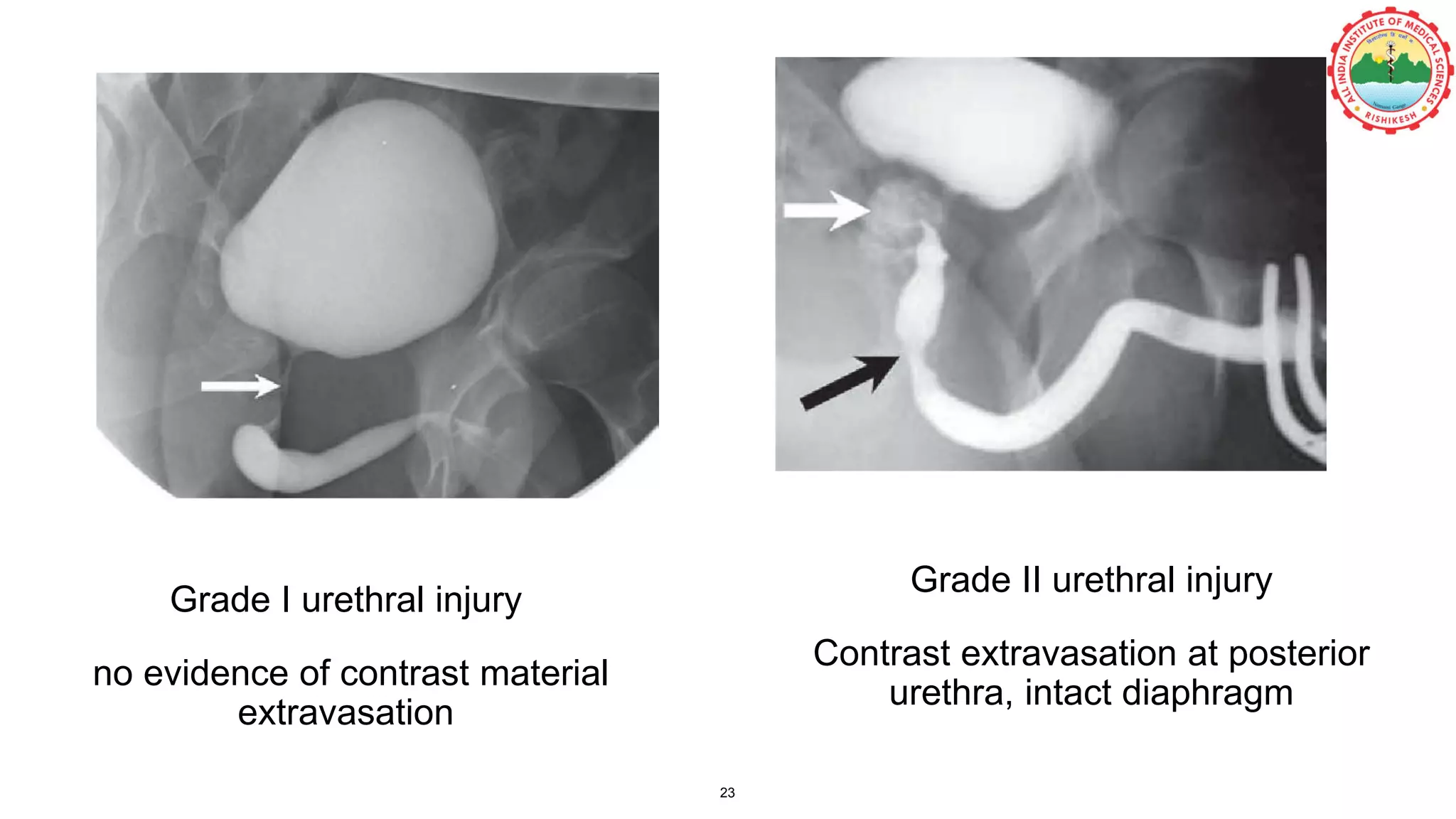
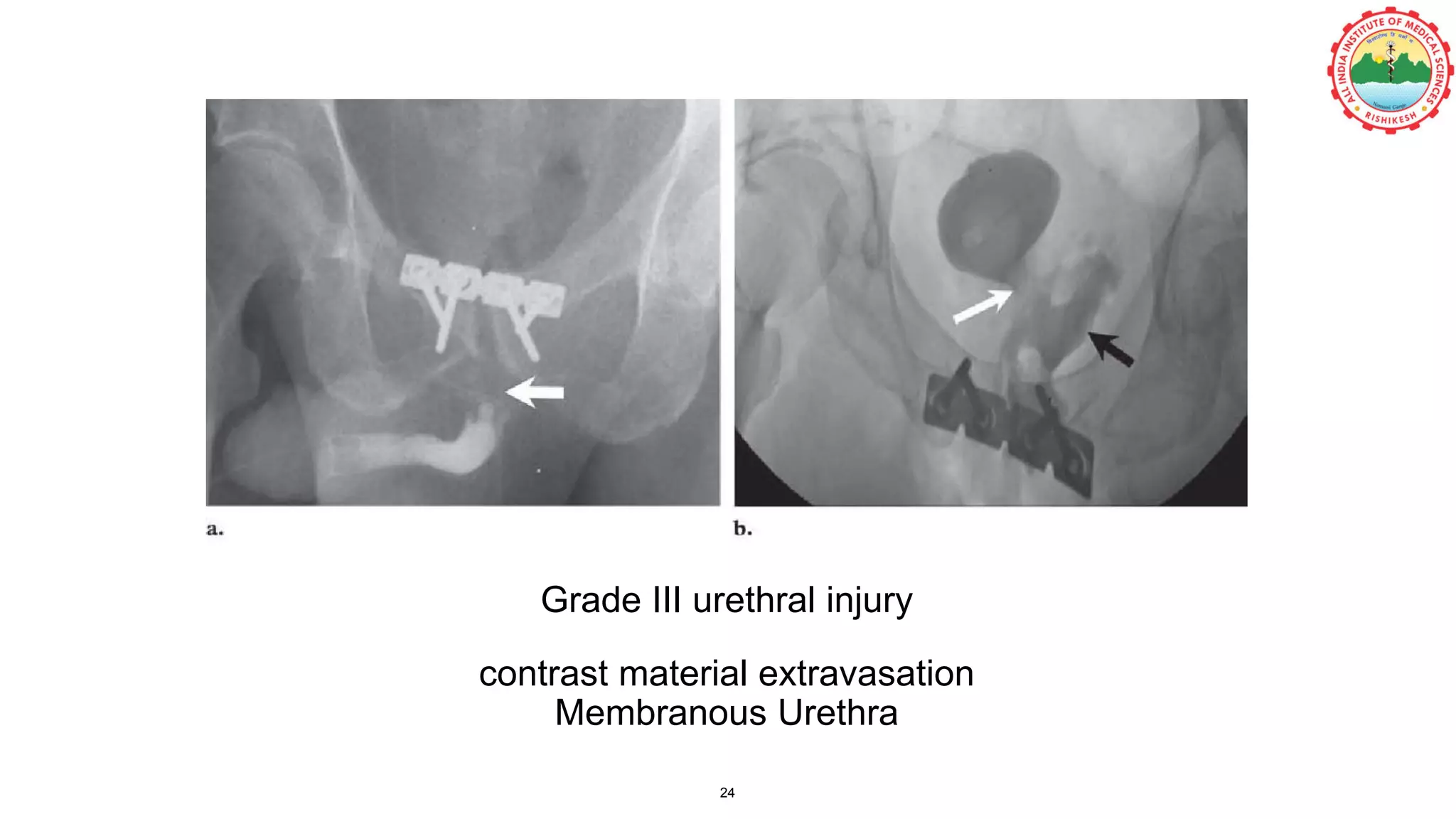
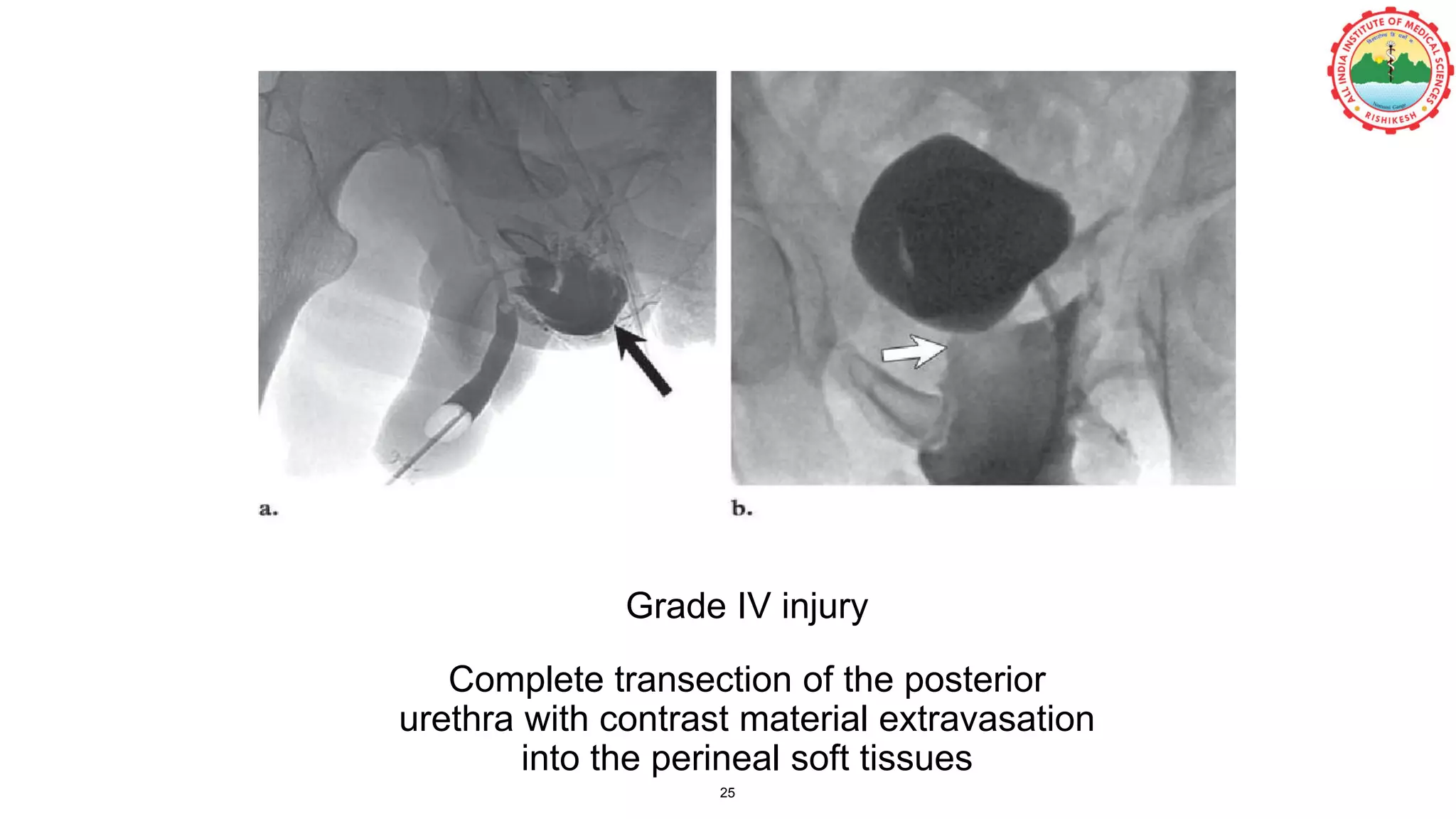
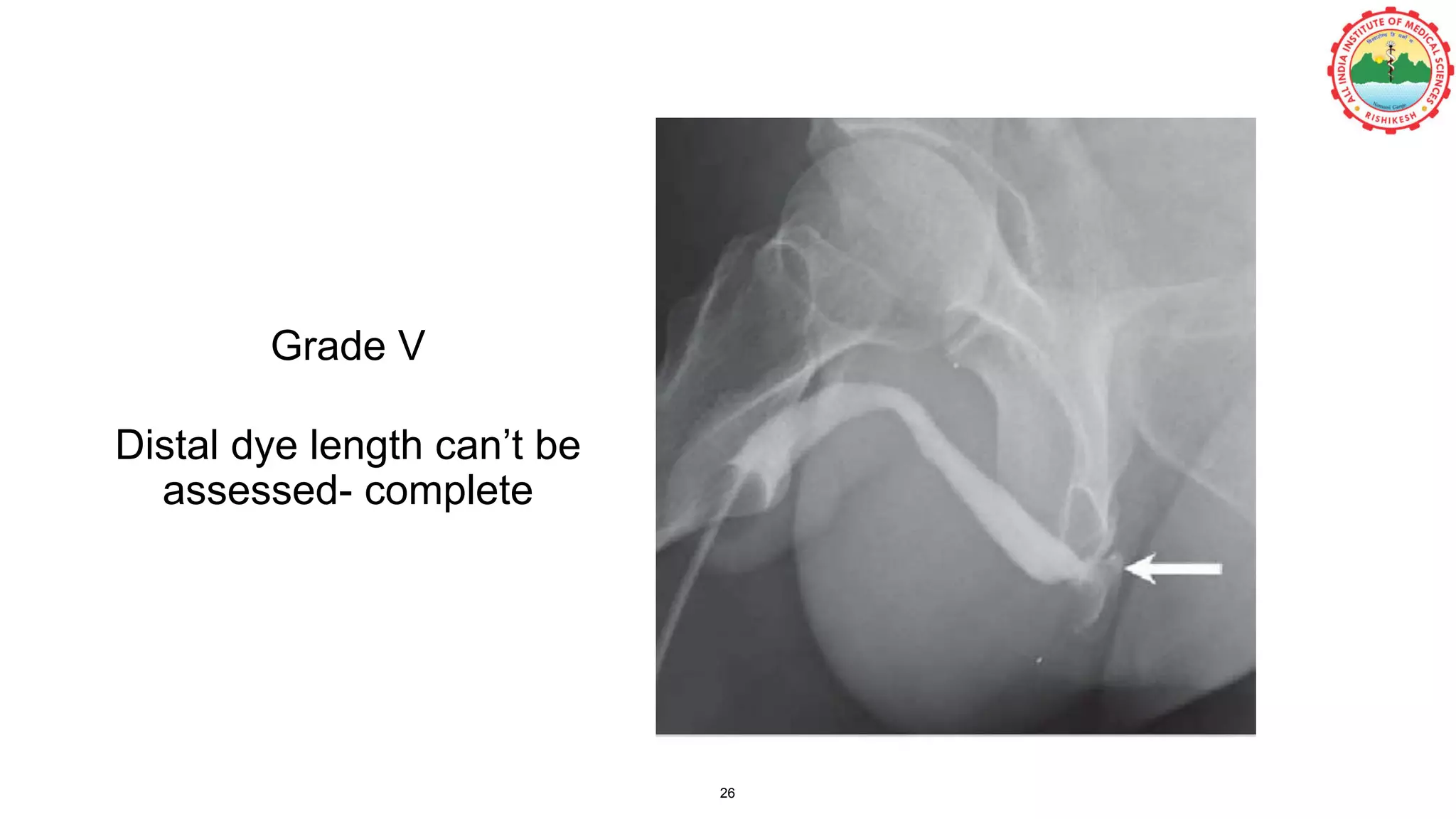
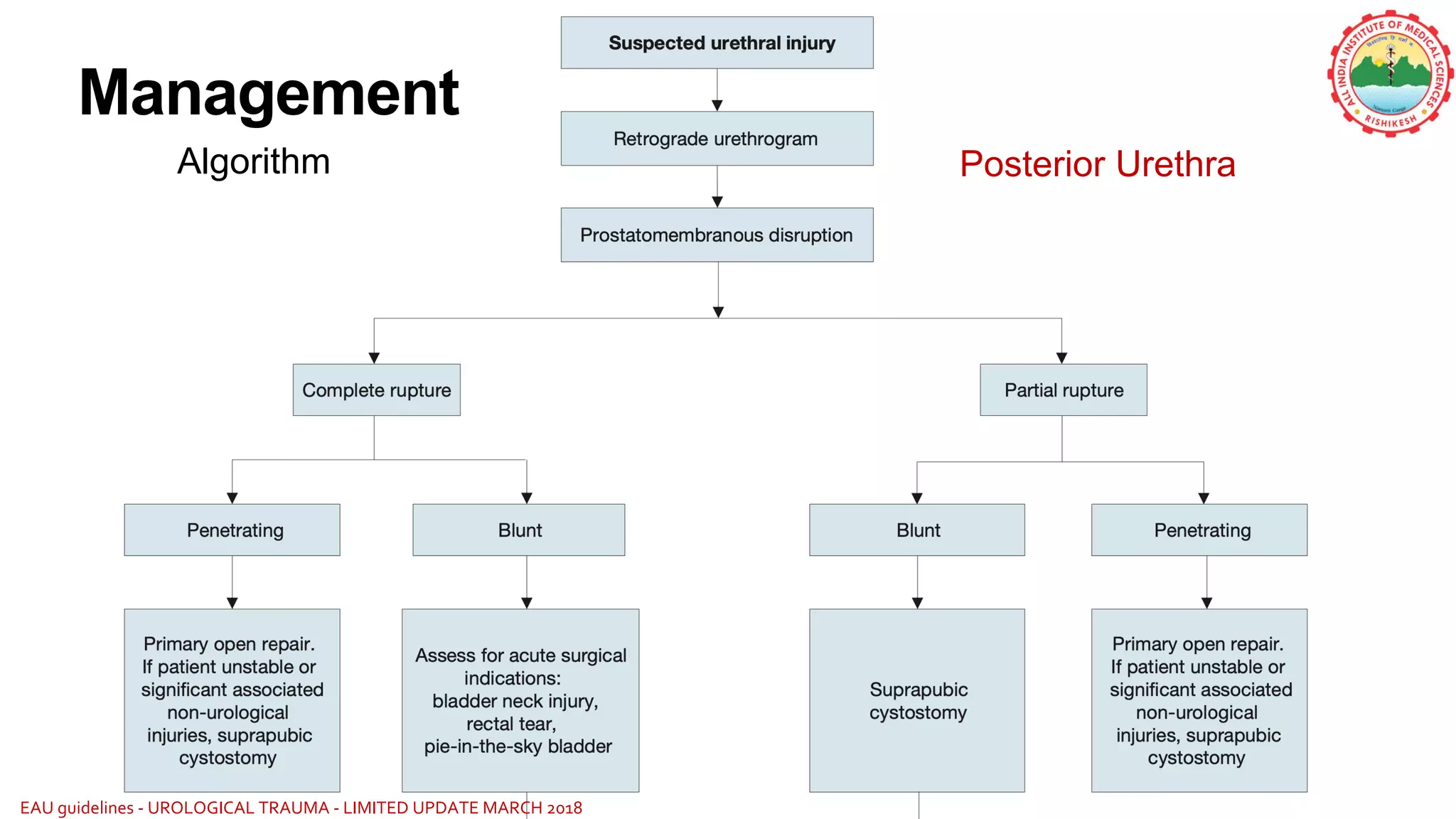
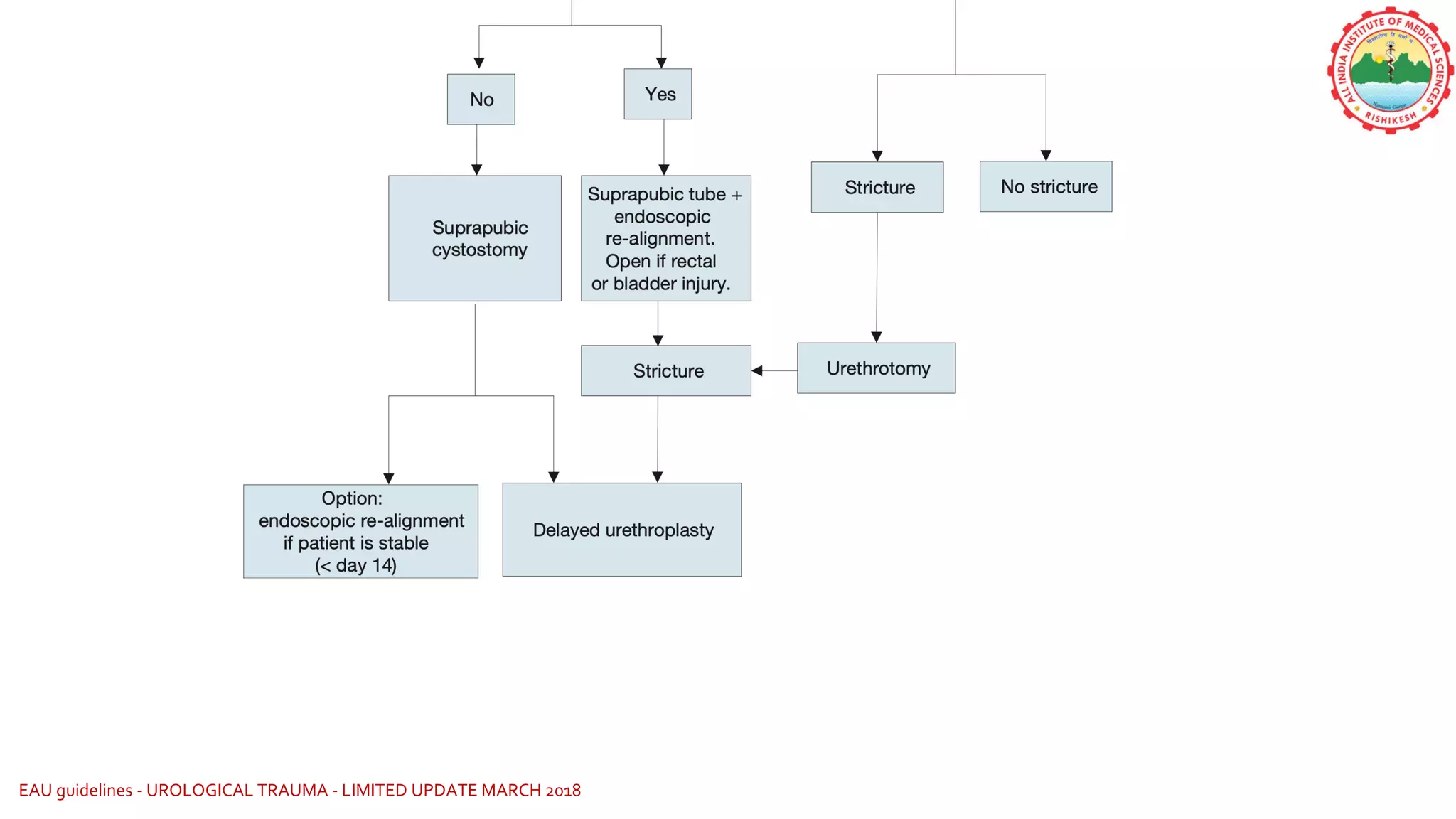
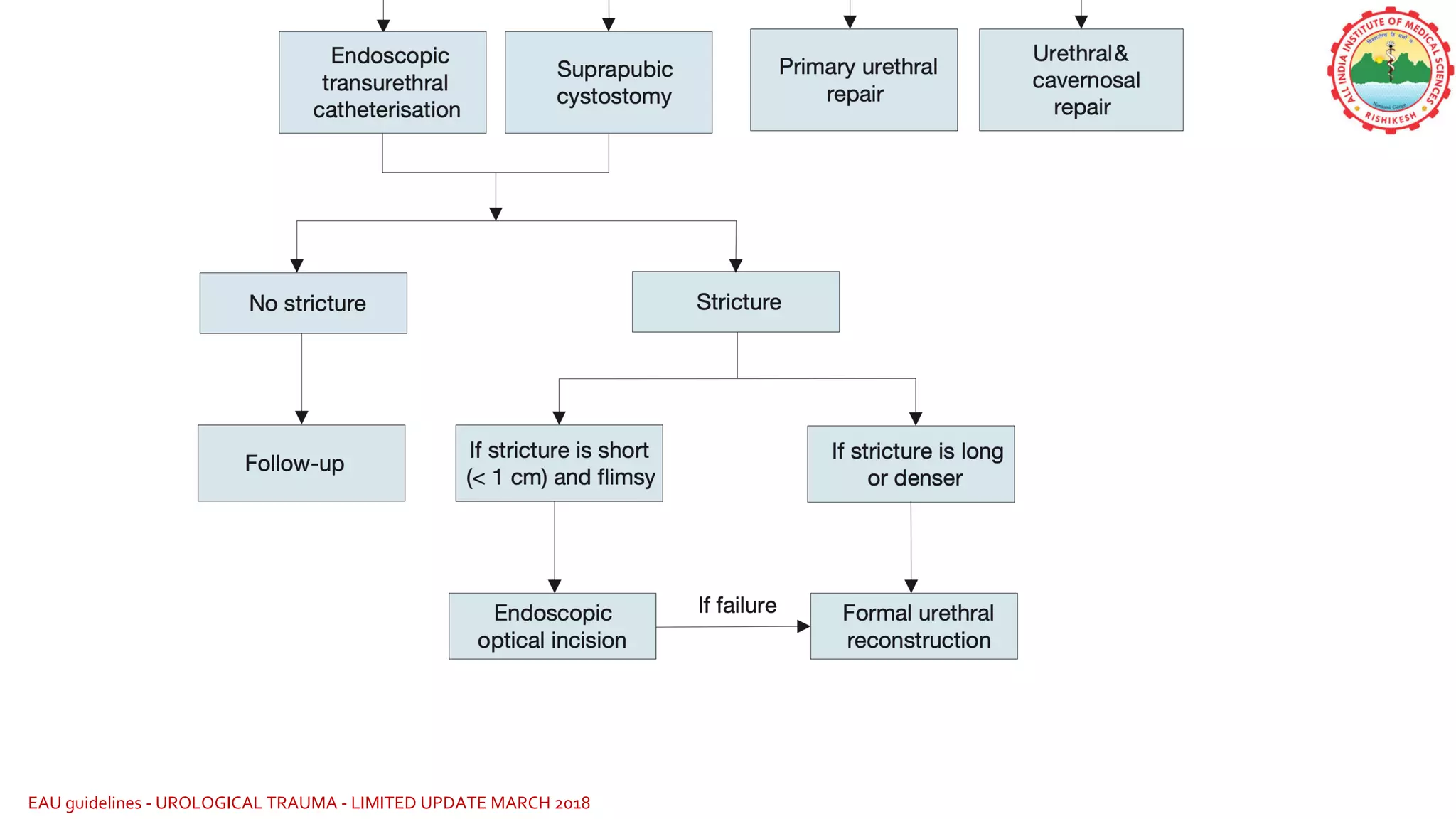
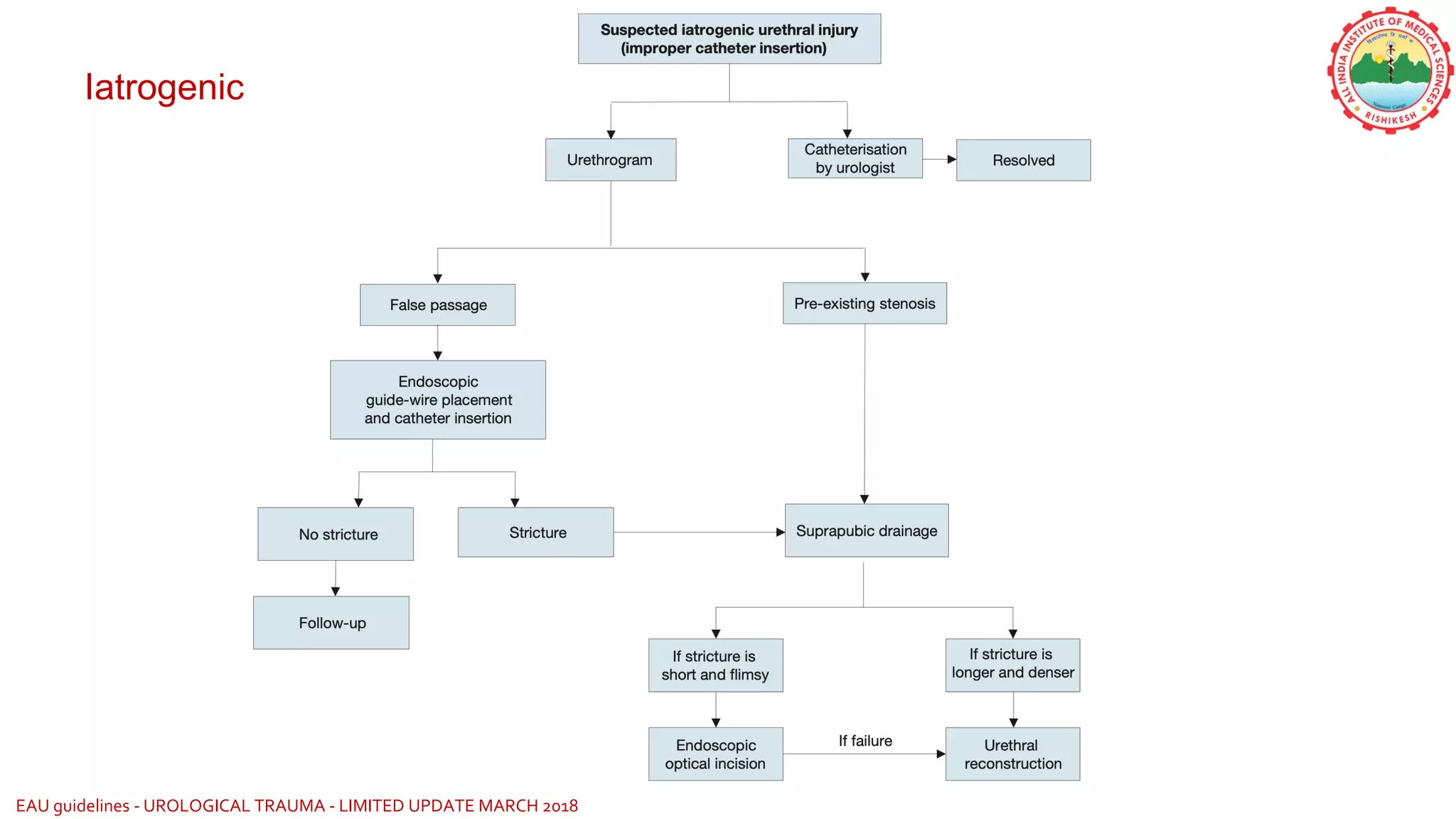
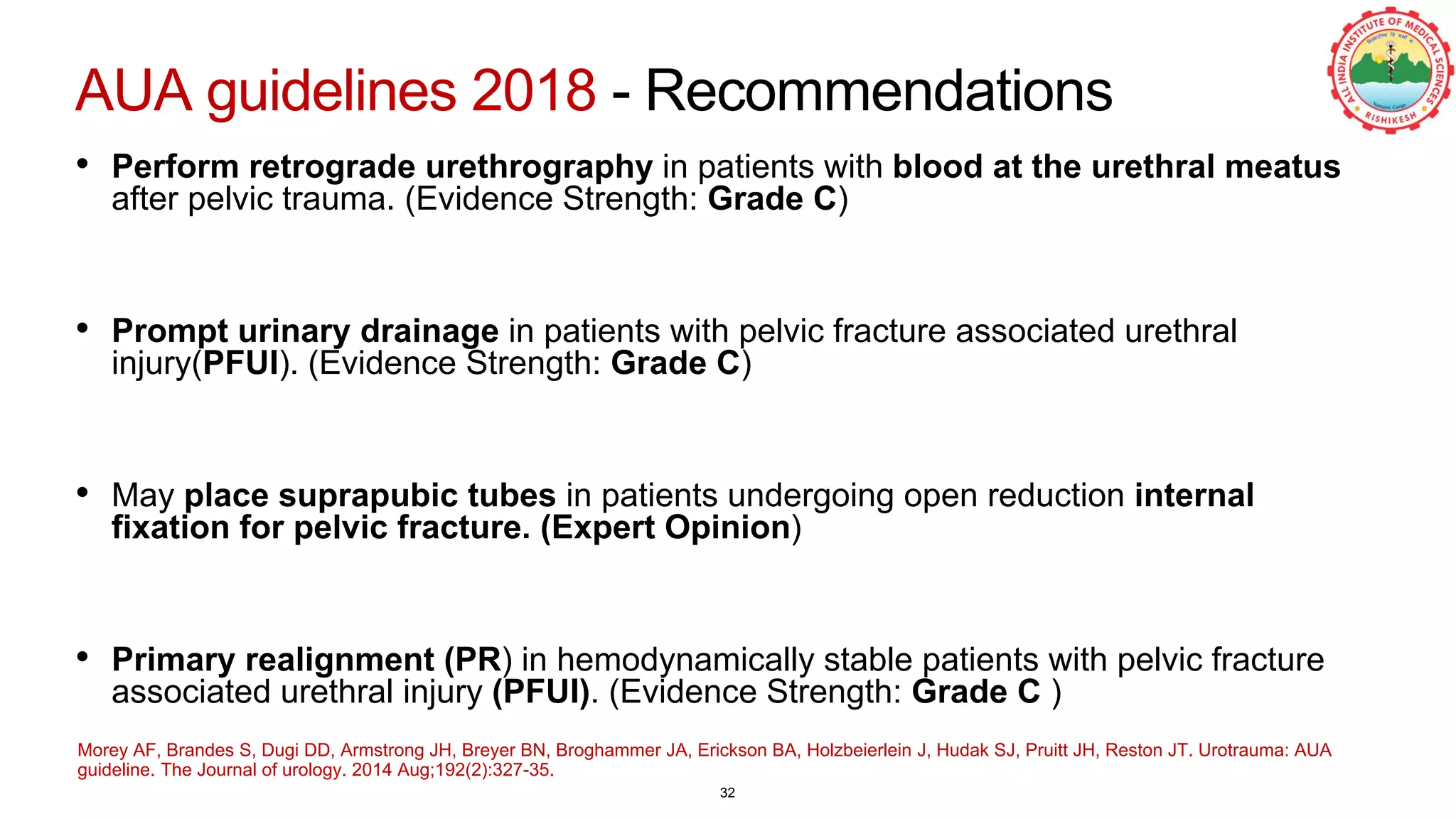
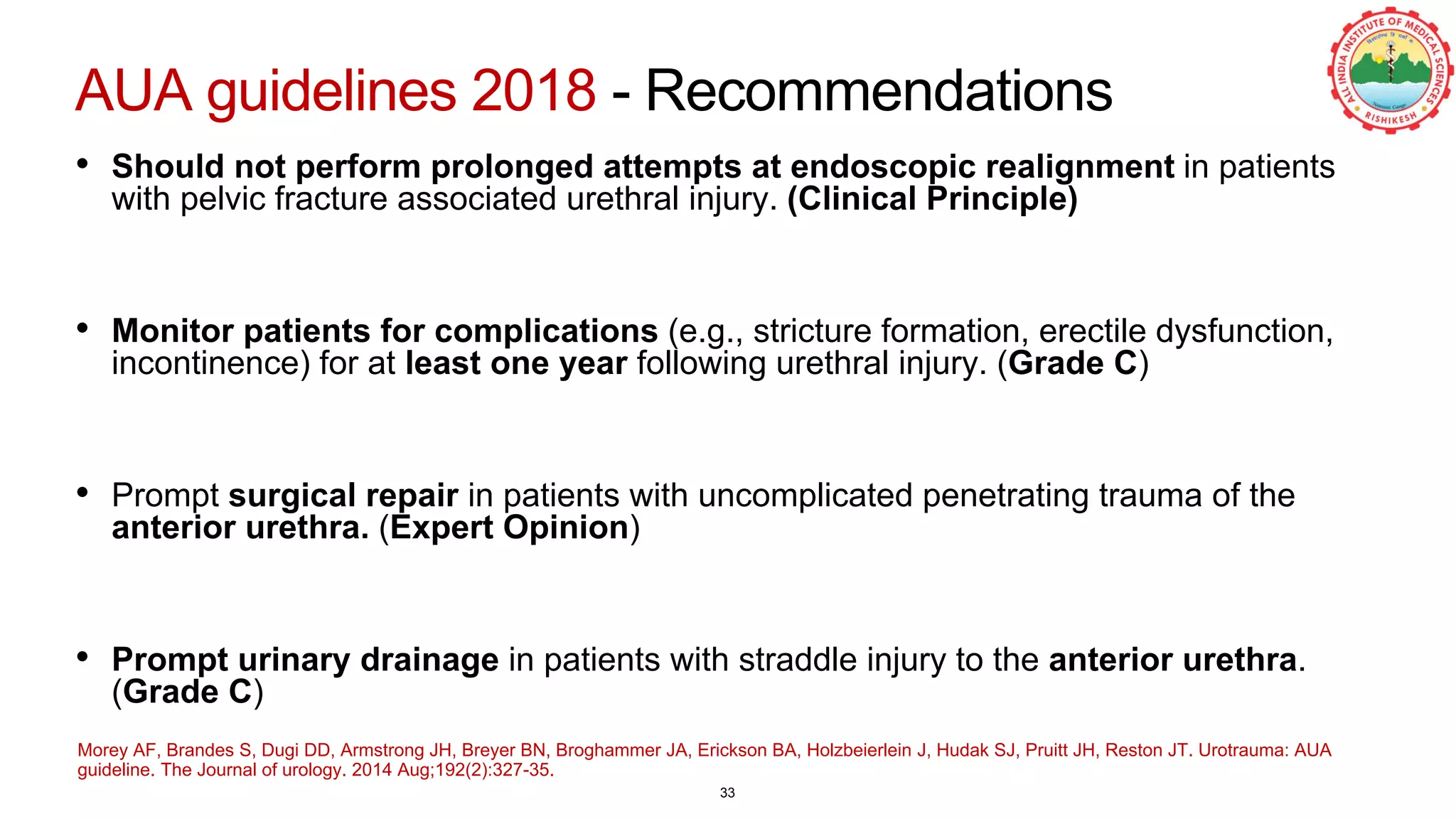
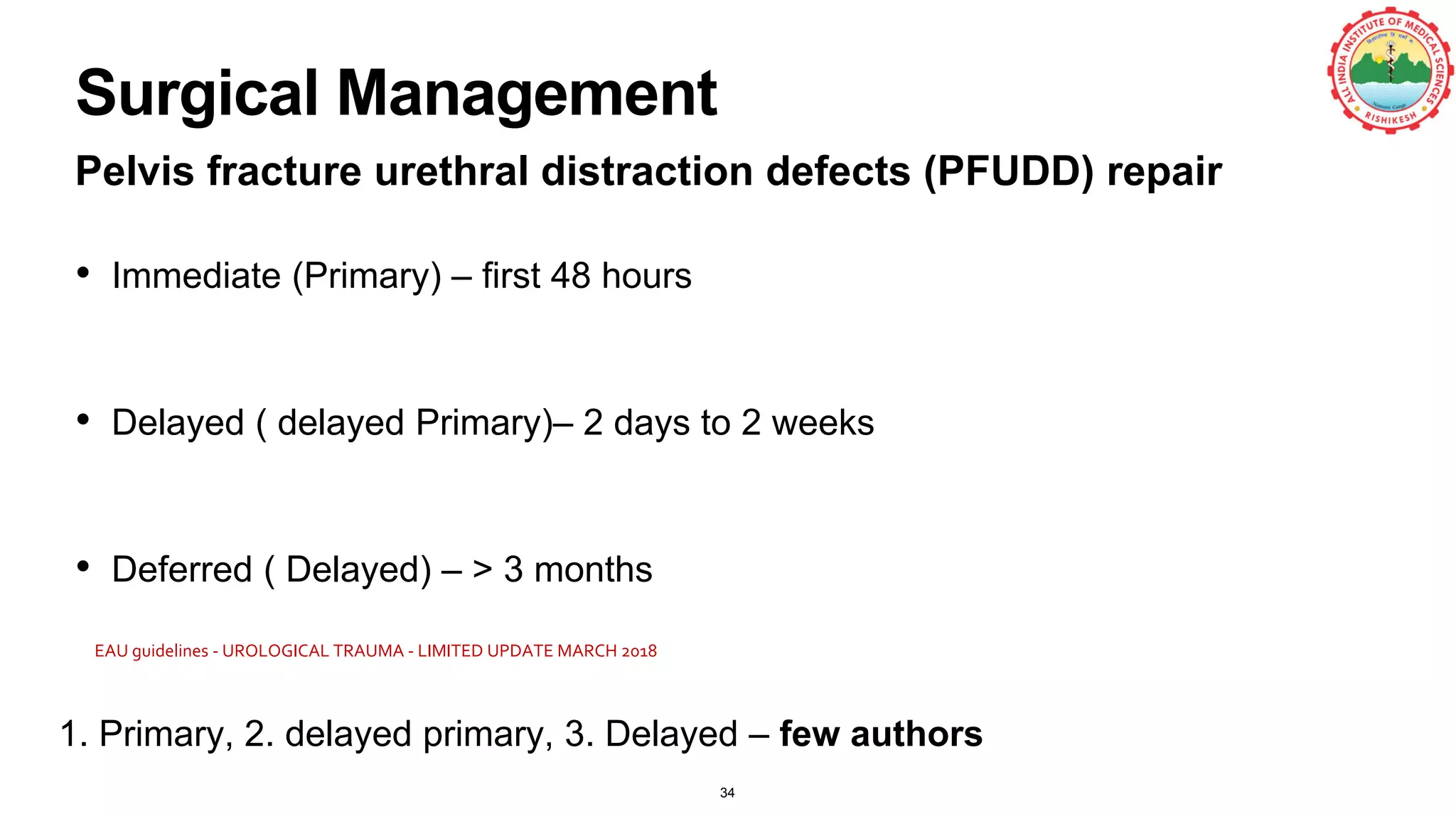
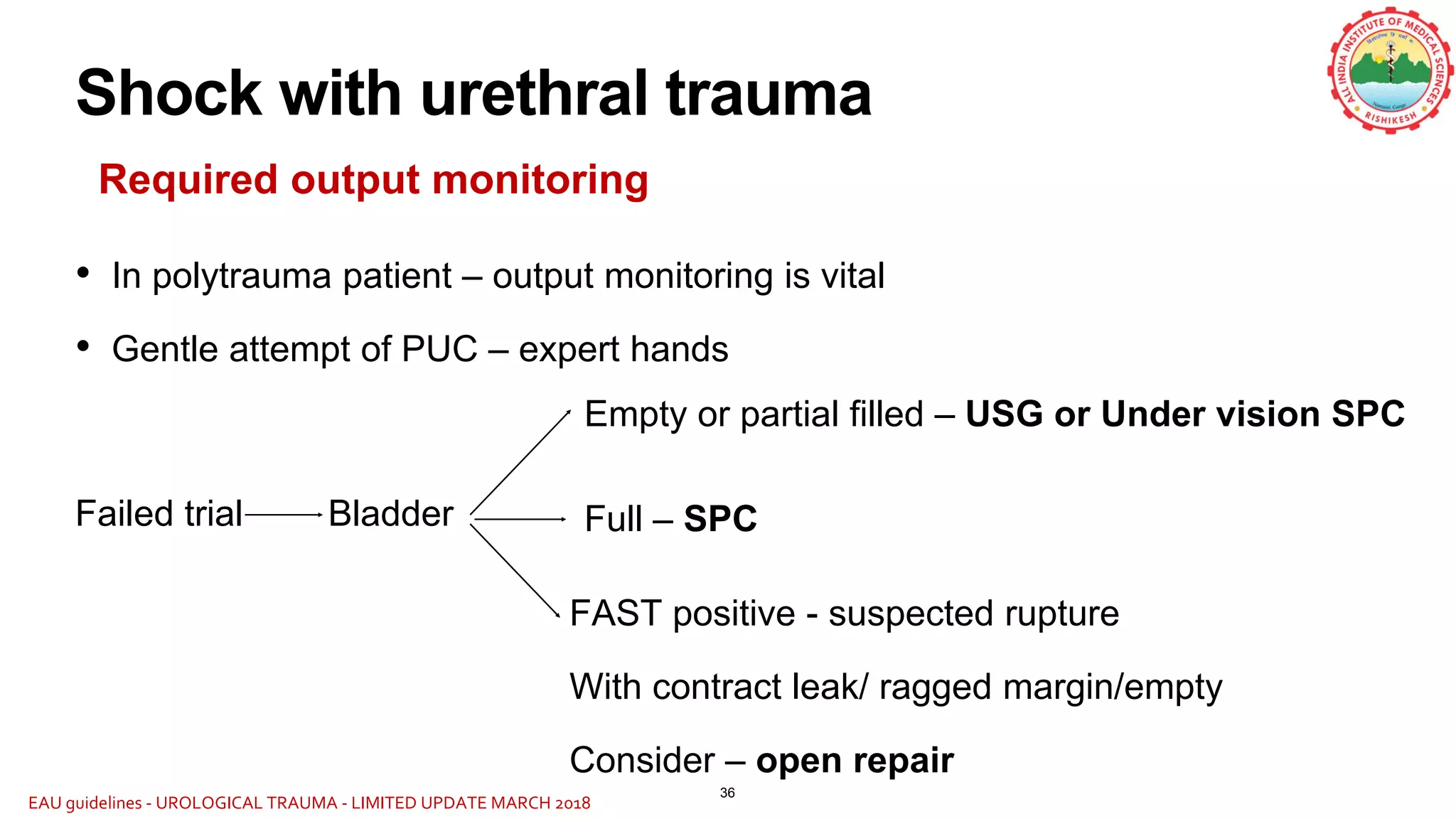
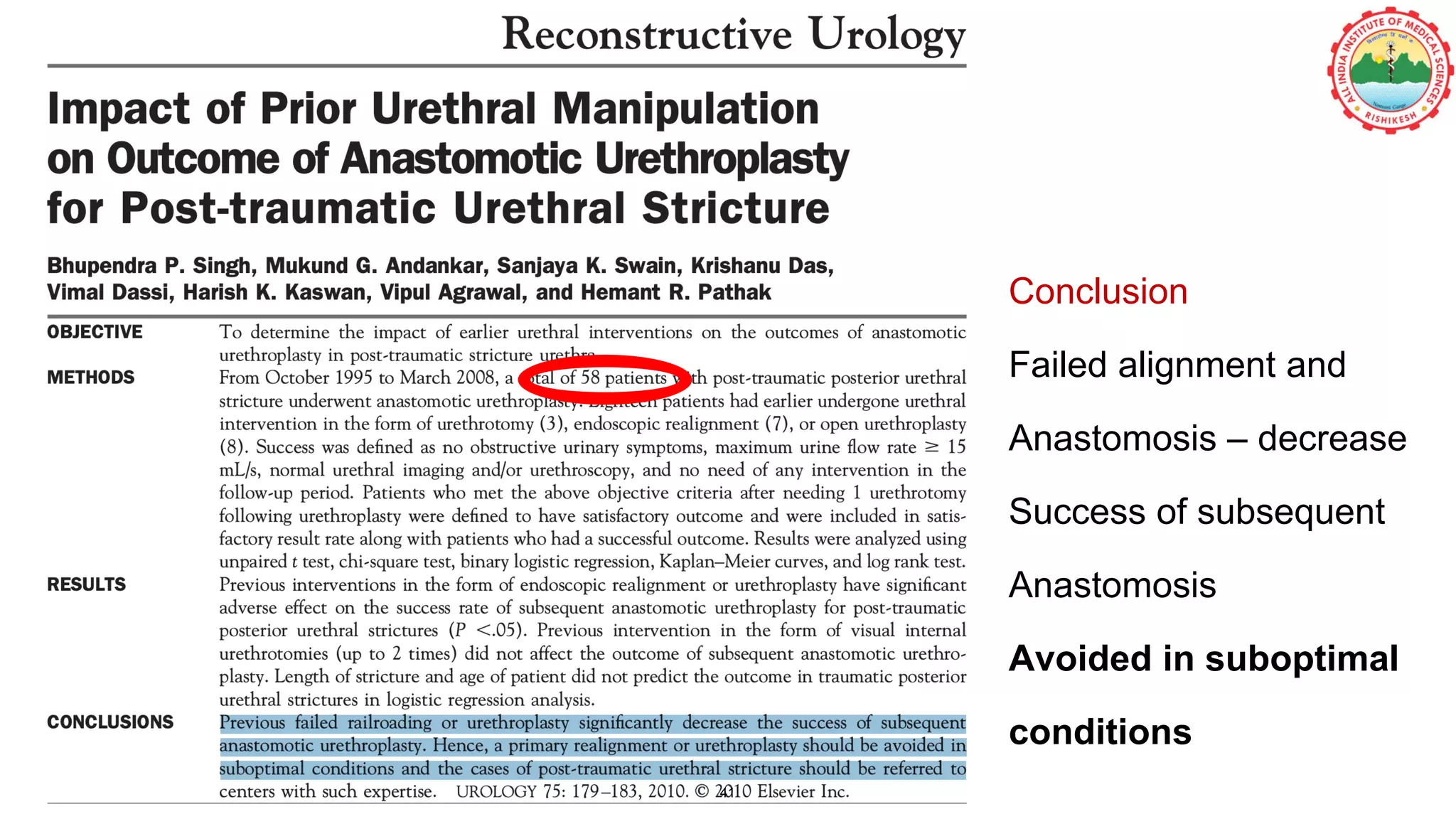
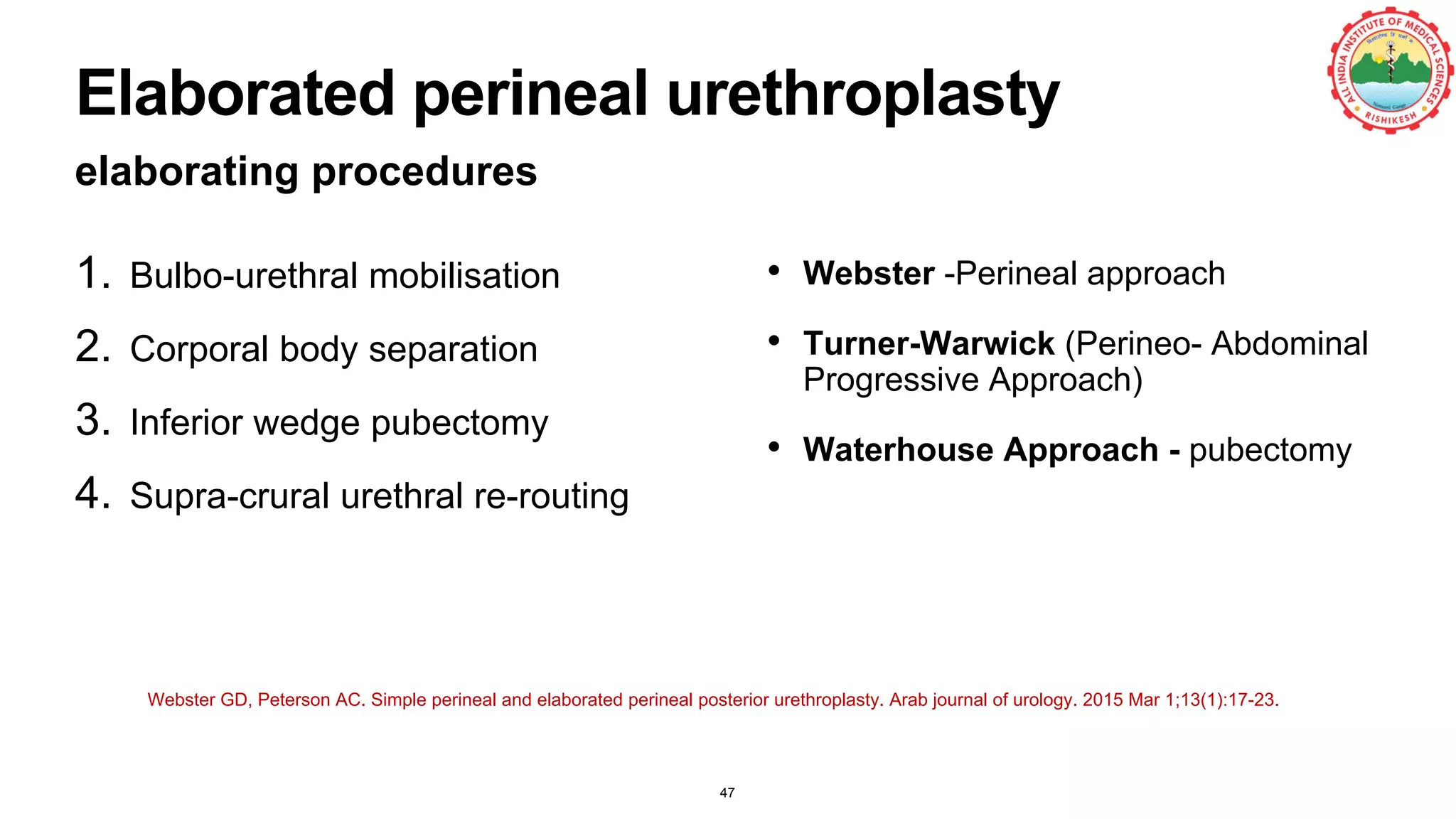
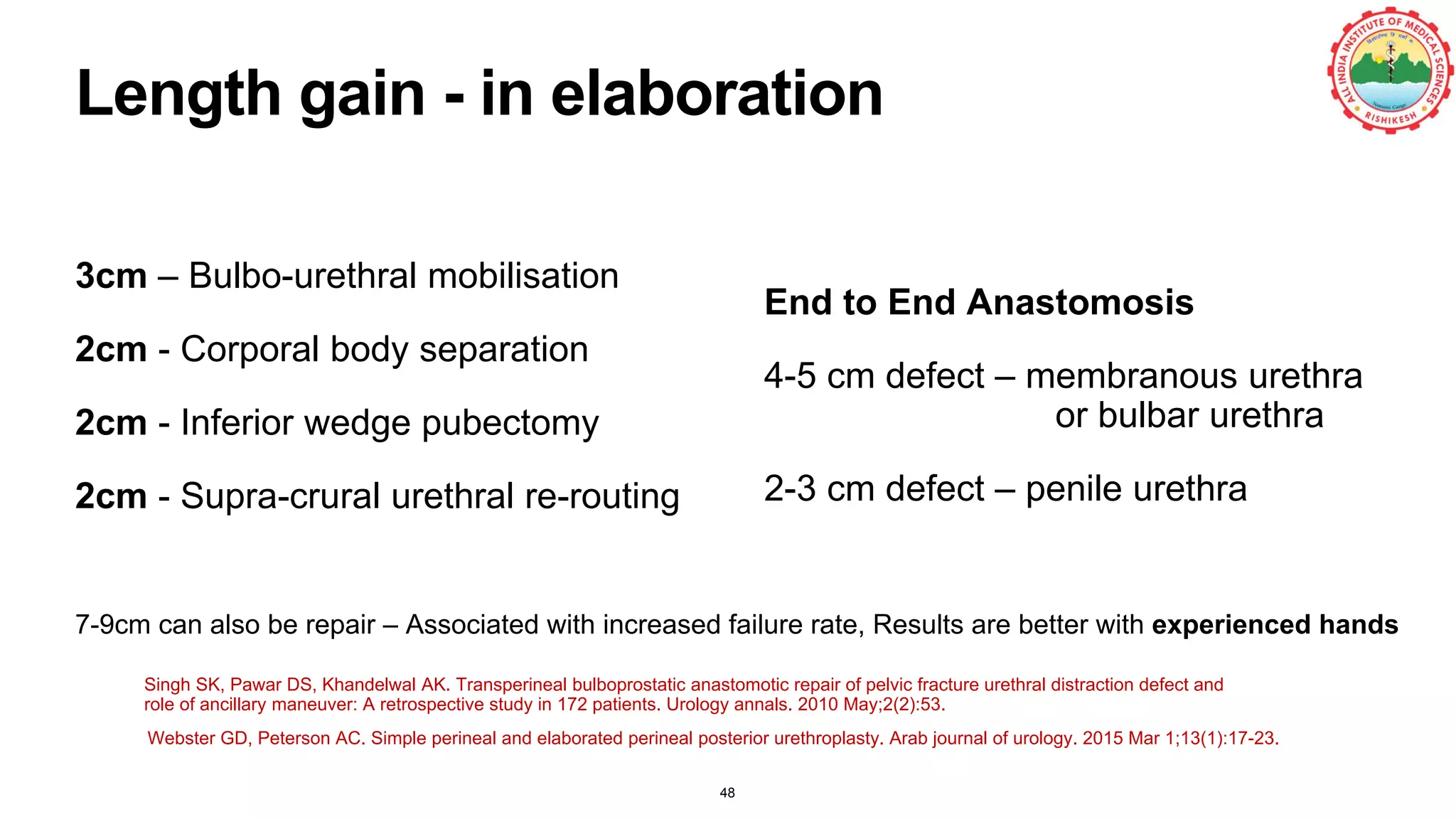
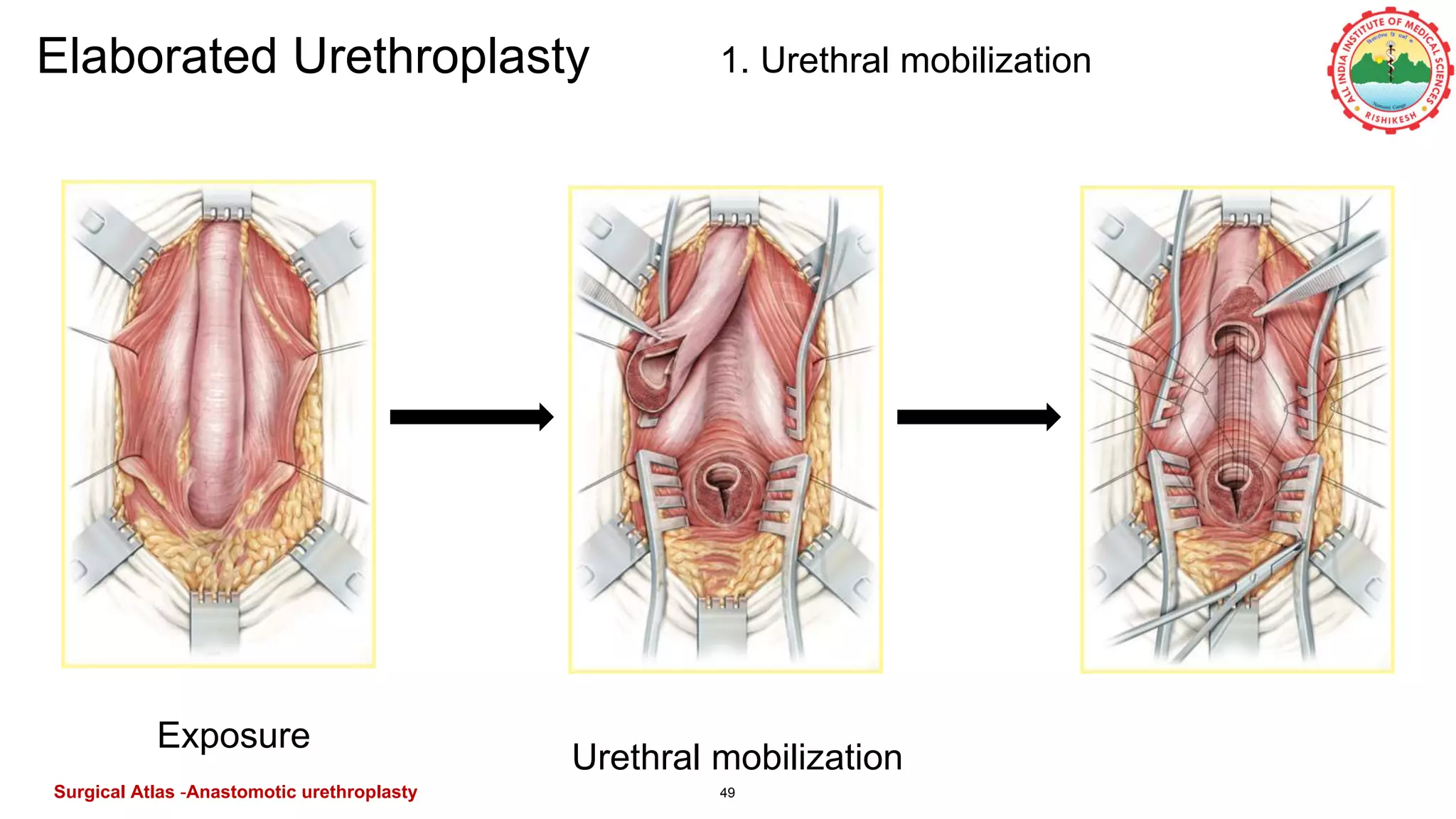
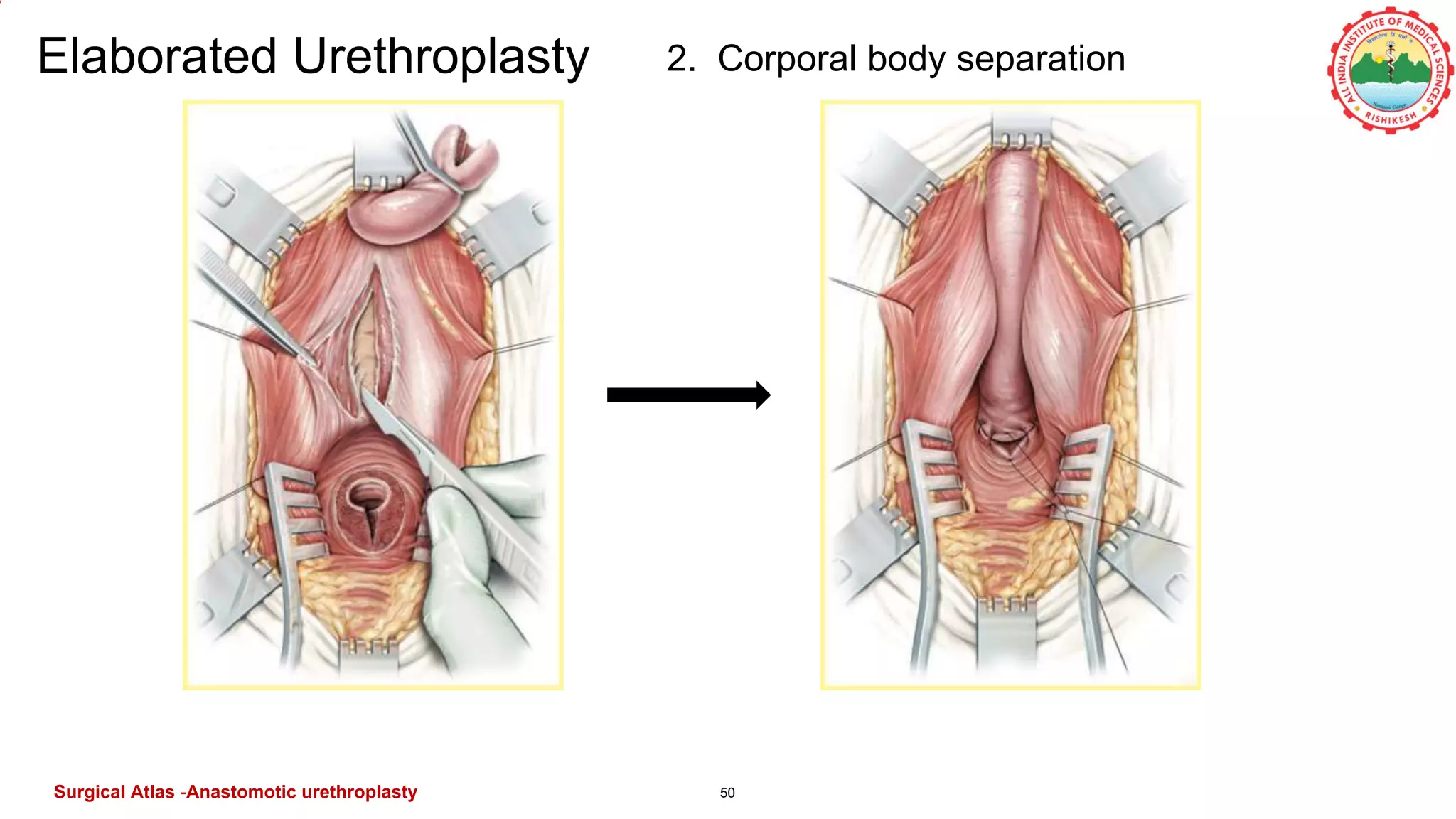
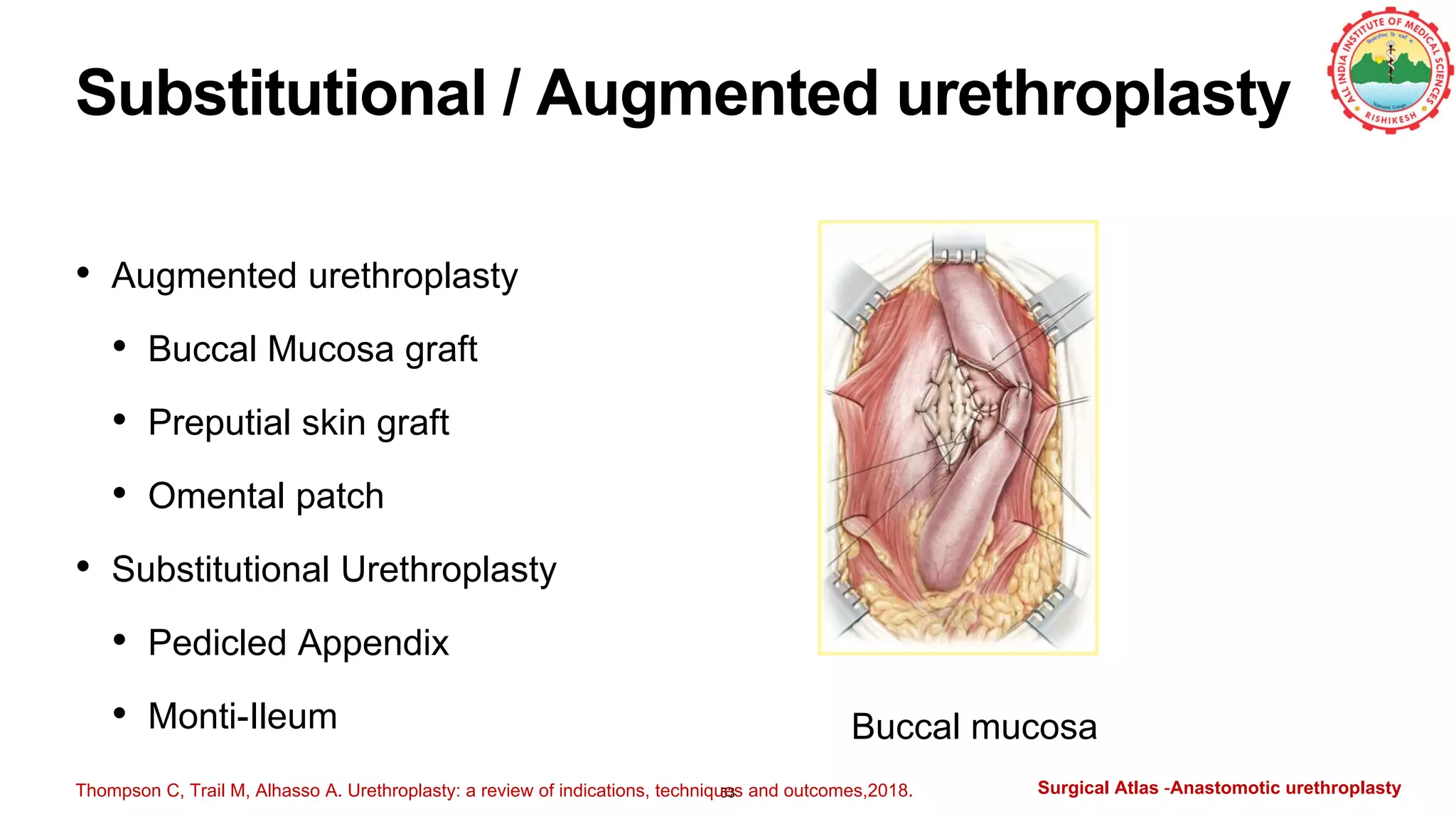
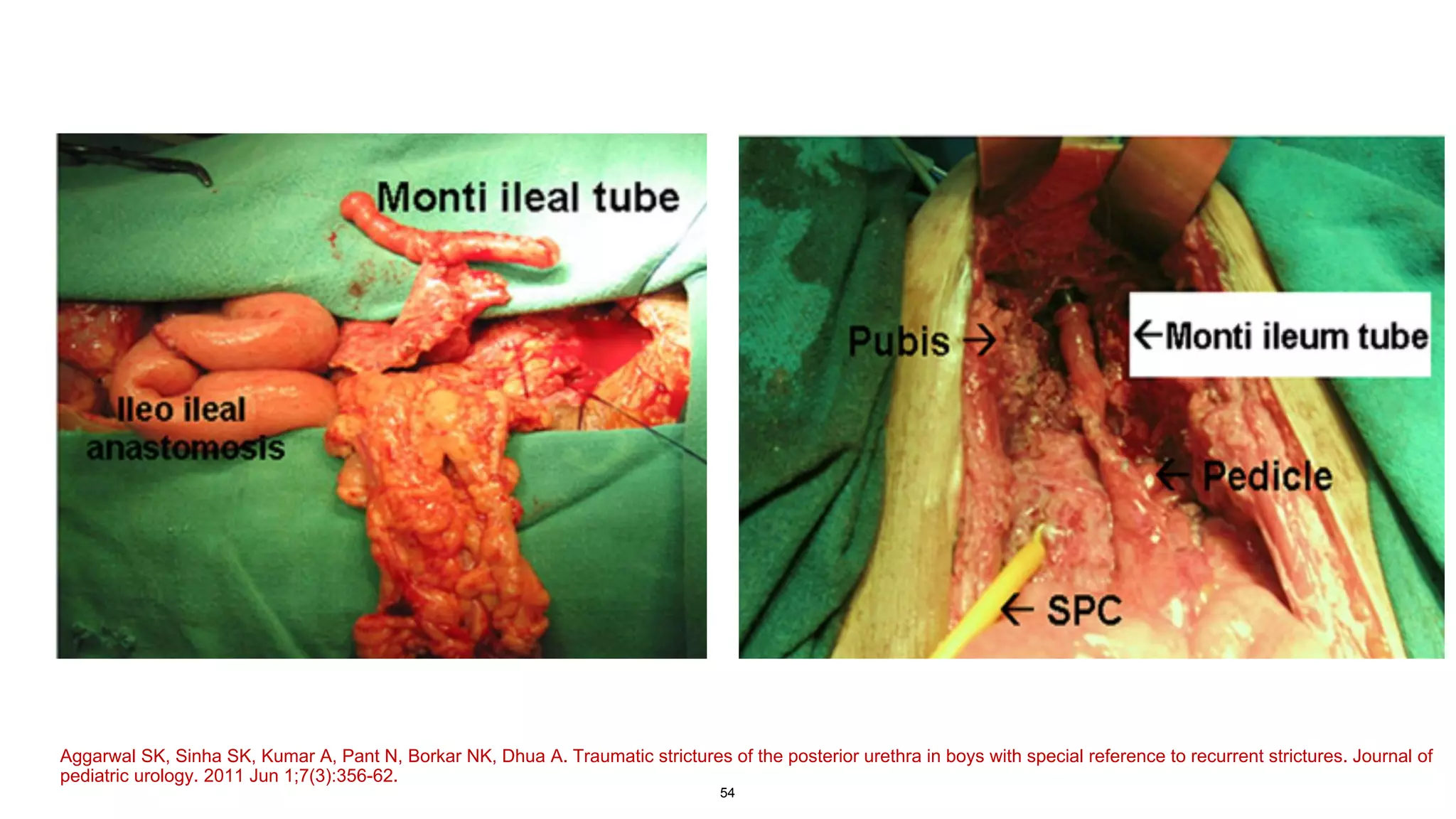
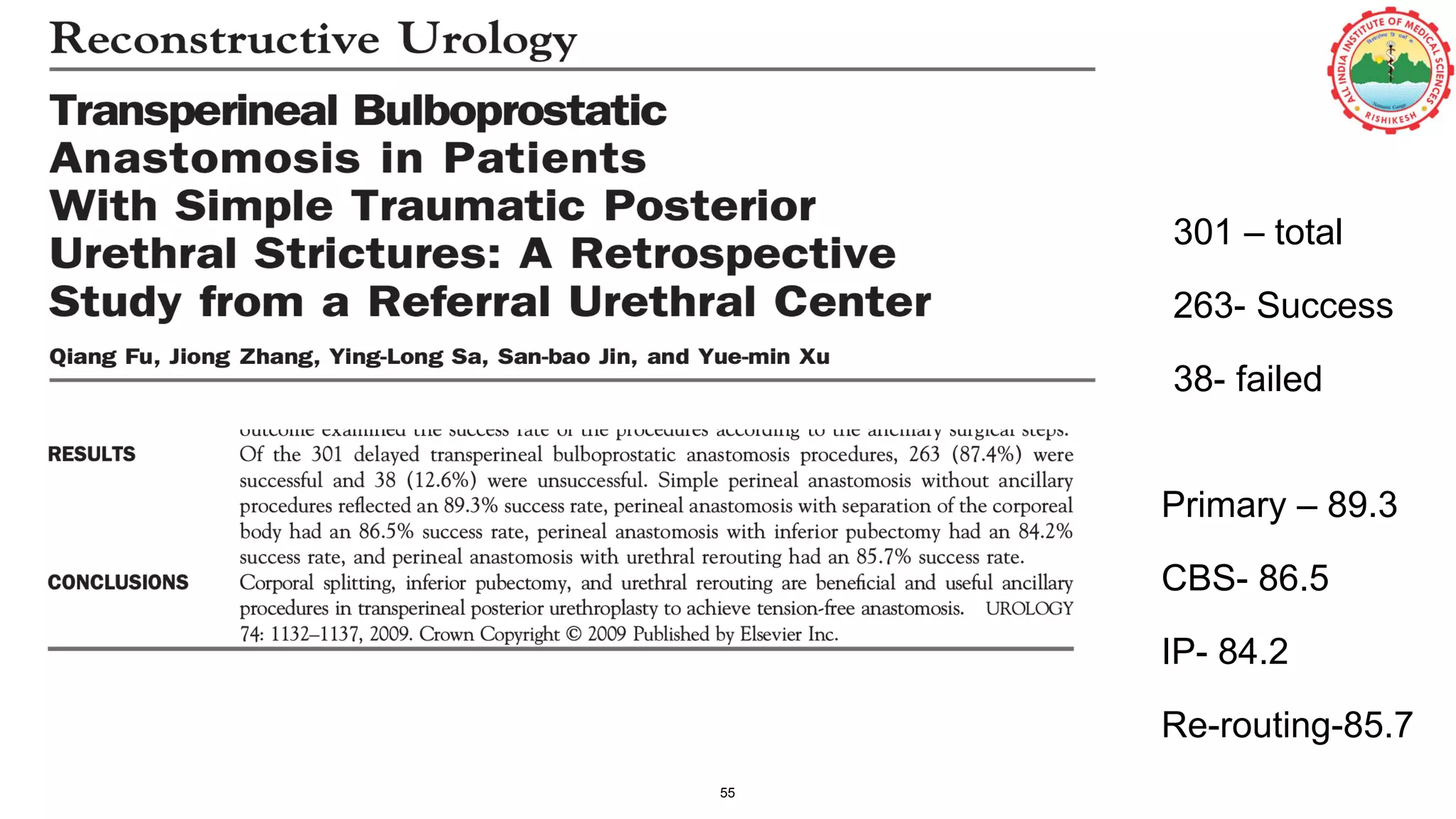
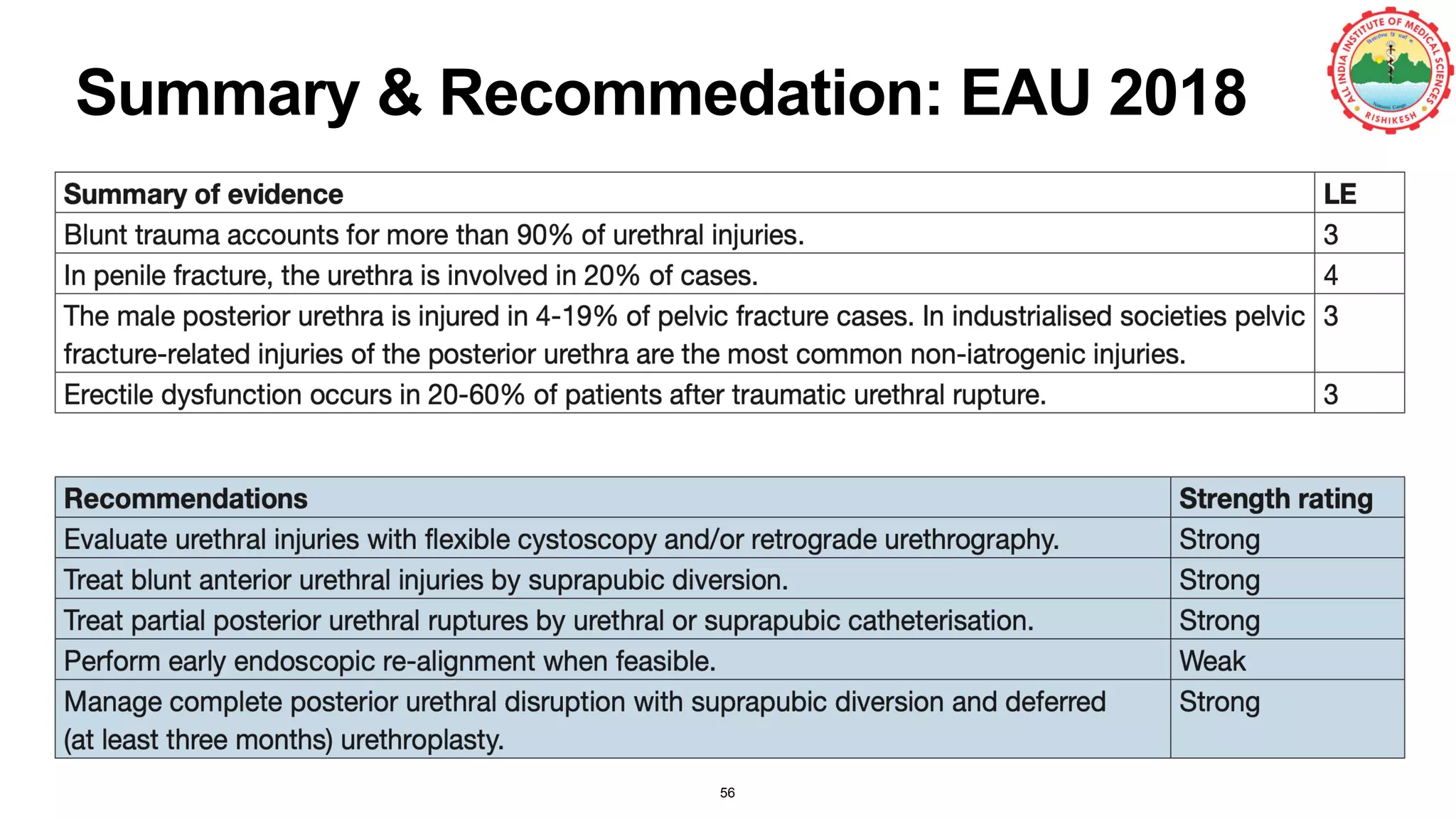
The document discusses the clinical approach to urethral trauma, emphasizing the assessment, diagnosis, and management of patients with suspected urethral injuries, particularly in cases of pelvic fractures. It highlights case studies, types of urethral injuries, grading systems, and guidelines for immediate and delayed interventions. The management strategies include surgical techniques and considerations for effective treatment and monitoring of complications.