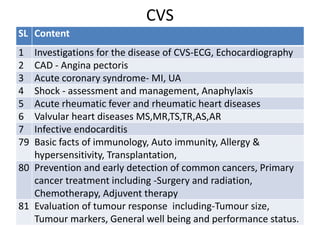
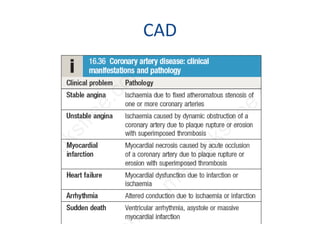
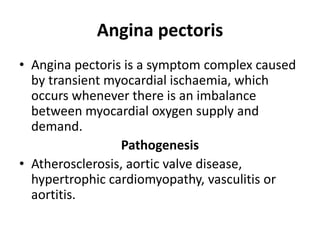
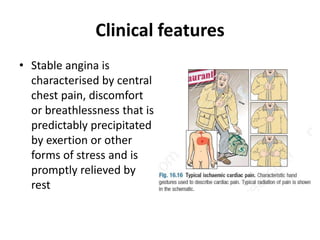
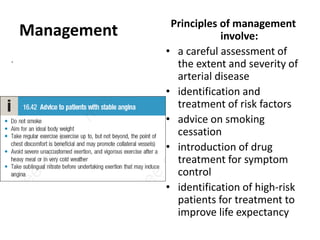
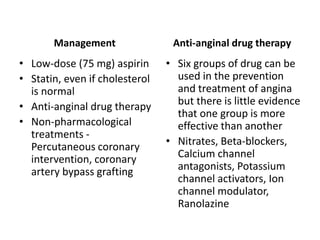
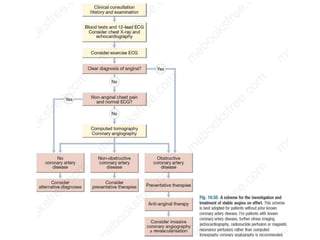
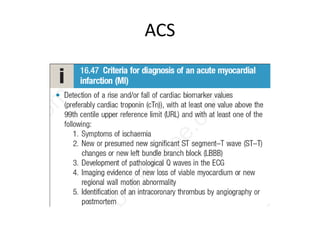
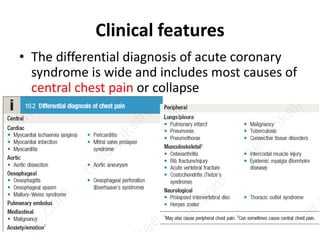
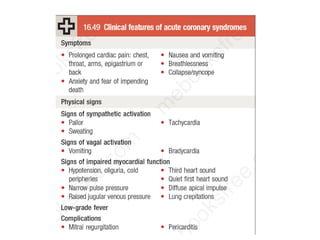
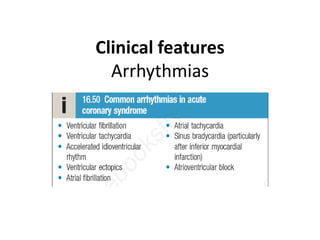
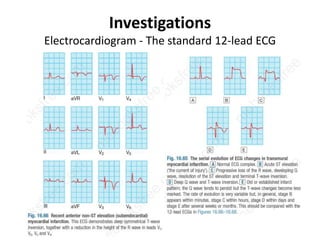
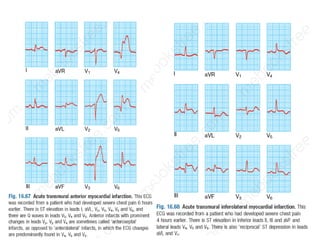
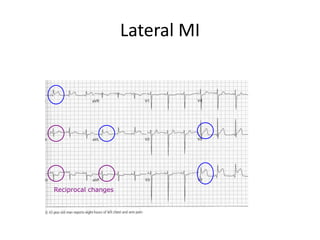
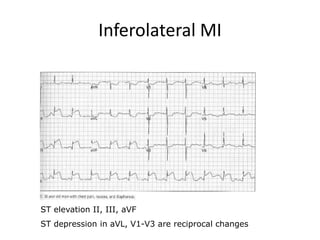
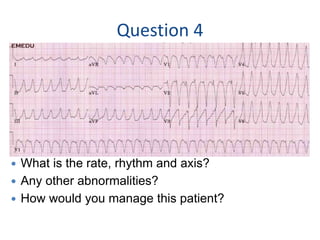
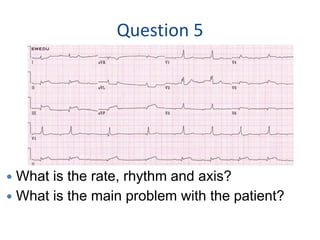
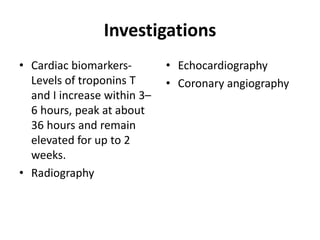
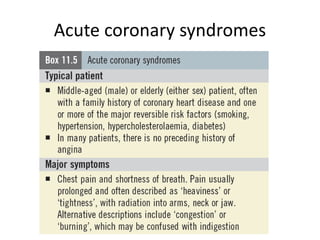
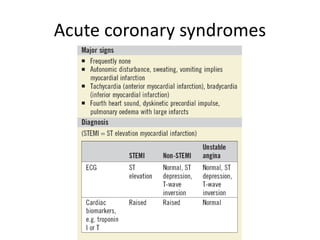
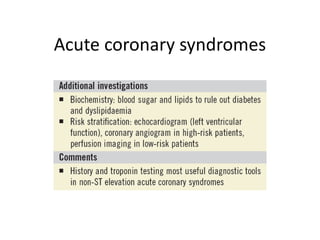
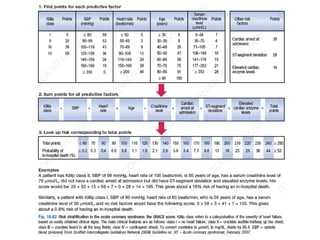
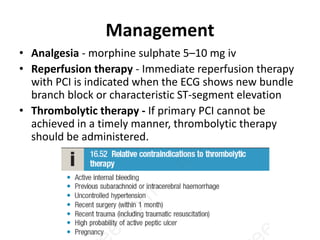
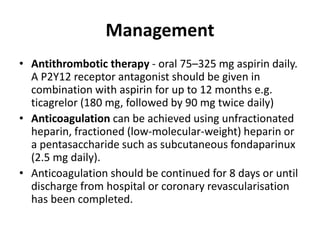
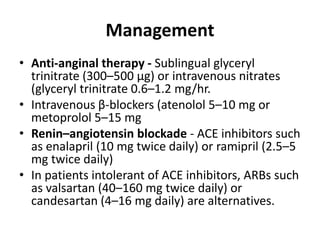
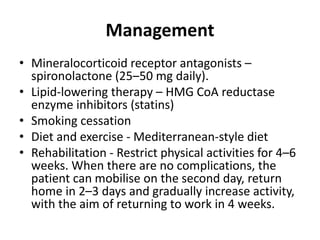
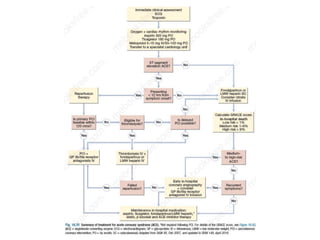
The document outlines the evaluation, management, and treatment principles for cardiovascular diseases, particularly focusing on coronary artery disease (CAD) and acute coronary syndrome (ACS). It details risk factors, clinical features, diagnostic investigations, and various treatment options including pharmacological therapies and lifestyle modifications. The importance of early detection and specific management strategies for high-risk patients is emphasized to improve outcomes.