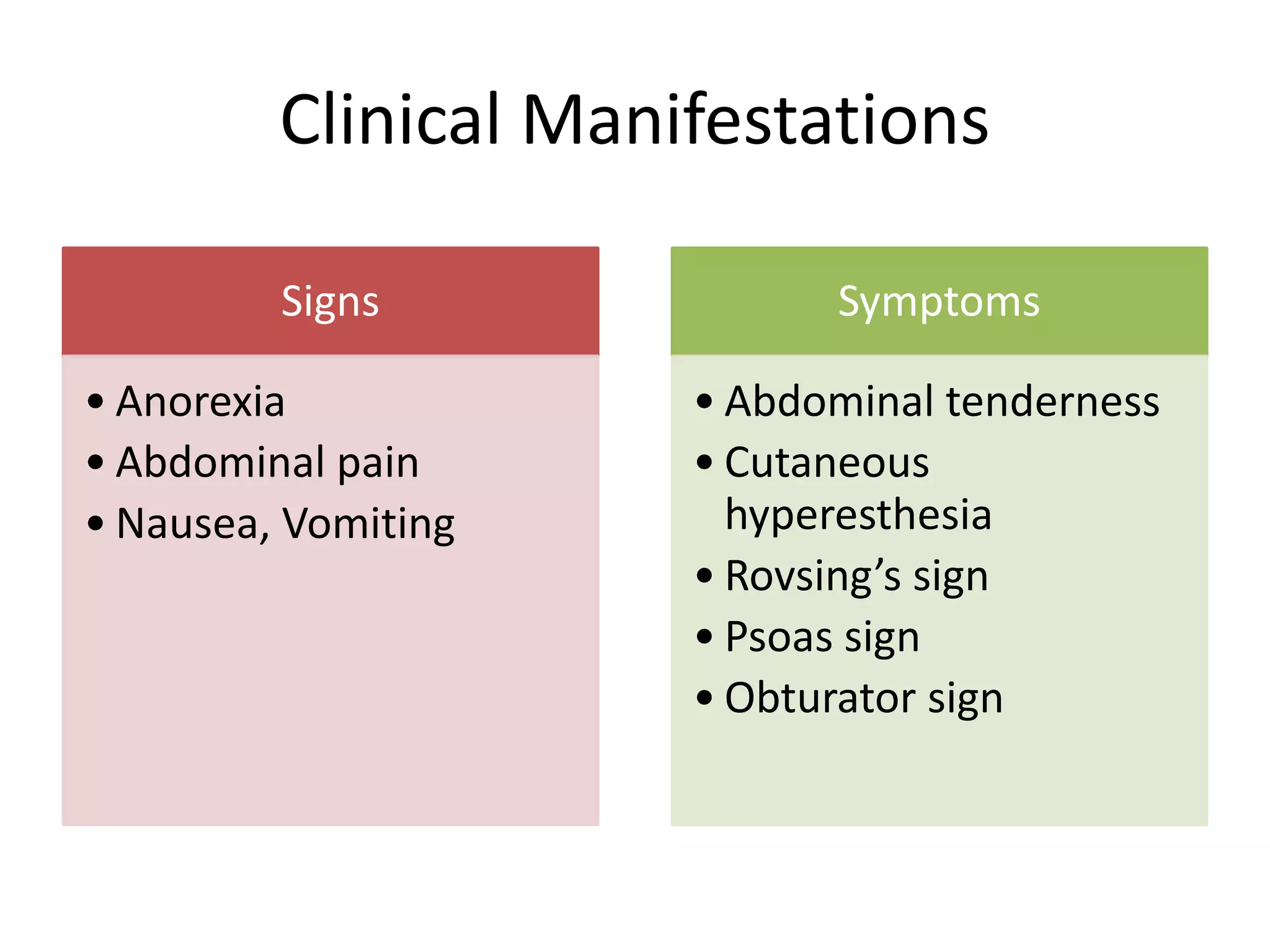
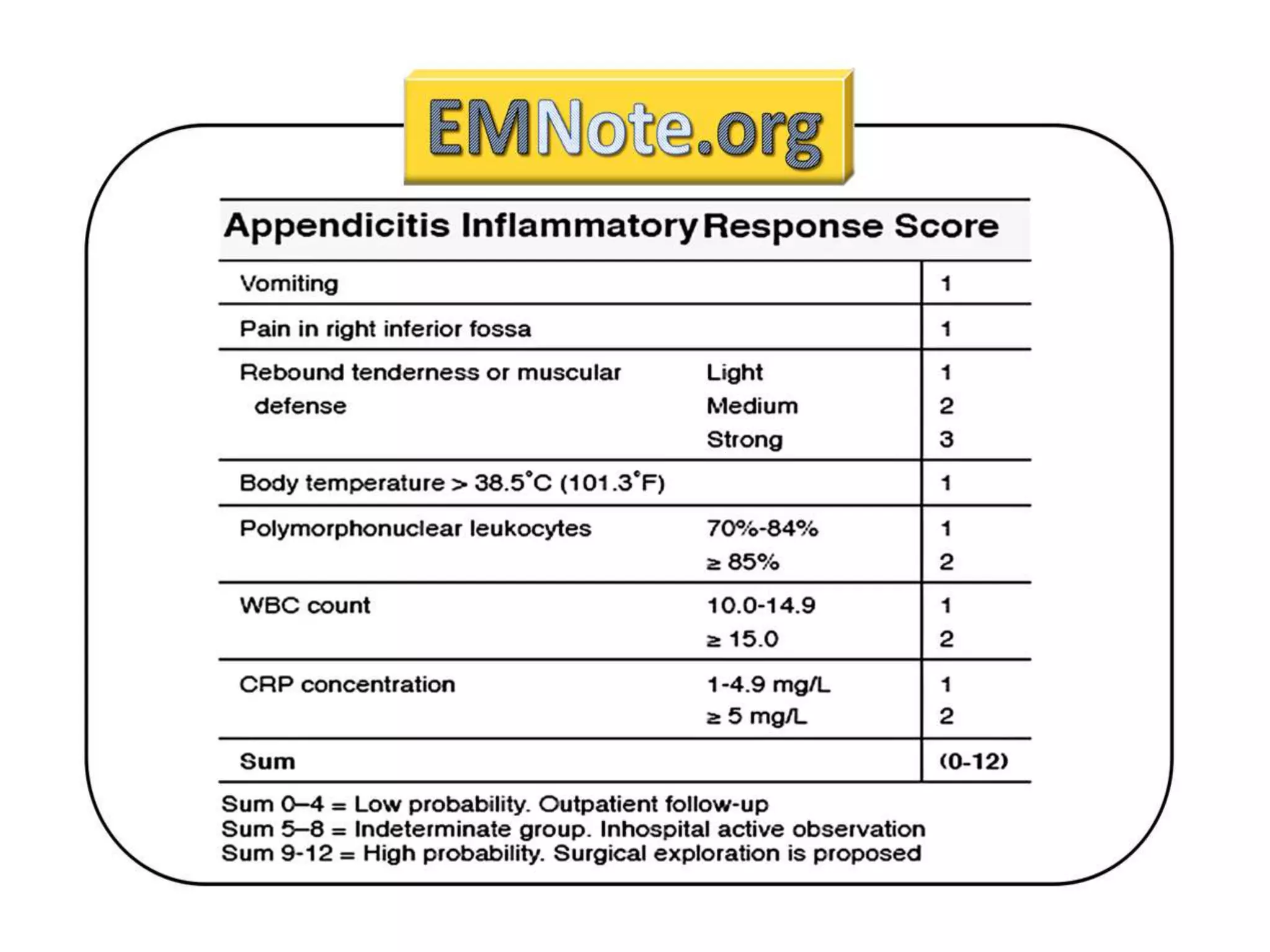
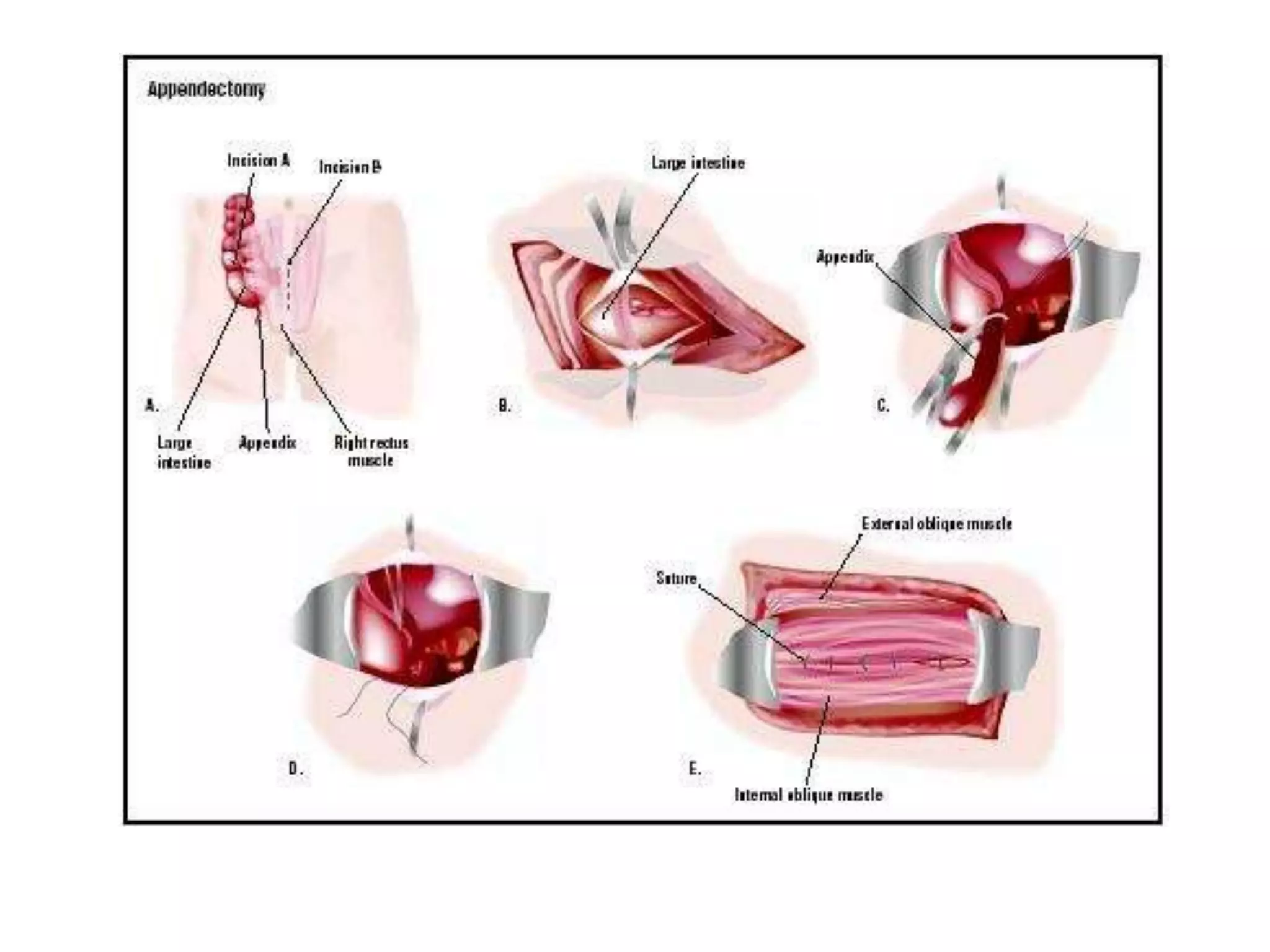
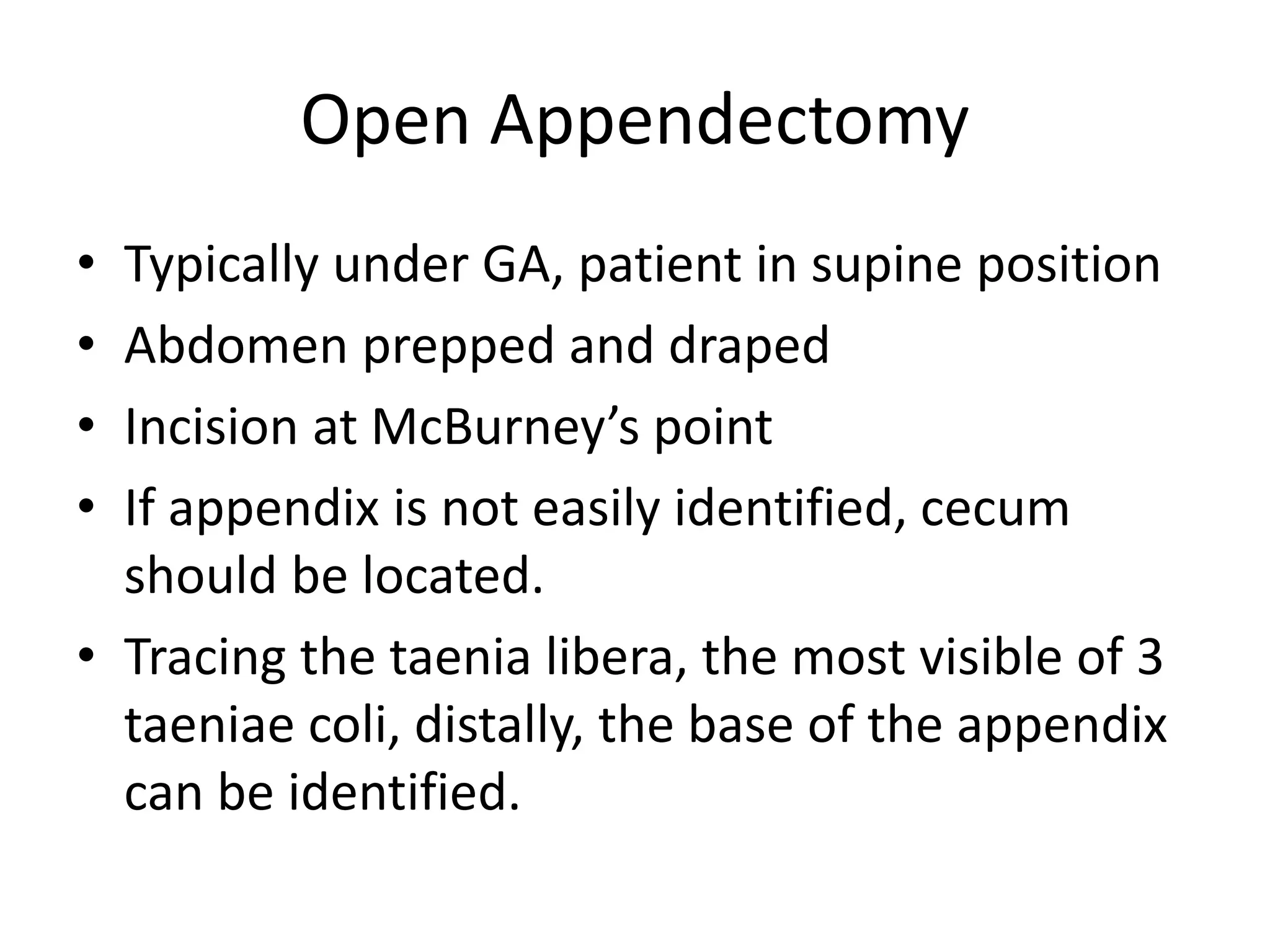
The document discusses acute appendicitis, summarizing the anatomy and physiology of the appendix, signs and symptoms of appendicitis, diagnostic tests used, and treatment options. The appendix is a thin tubular organ located at the base of the cecum that helps with immune function. Acute appendicitis is caused by obstruction leading to bacterial overgrowth and inflammation. Clinical manifestations include abdominal pain and tenderness. Imaging tests like ultrasound and CT scans are used for diagnosis. Treatment involves open or laparoscopic appendectomy to remove the inflamed appendix. Antibiotics are also used before and after surgery depending on the severity of the appendicitis.