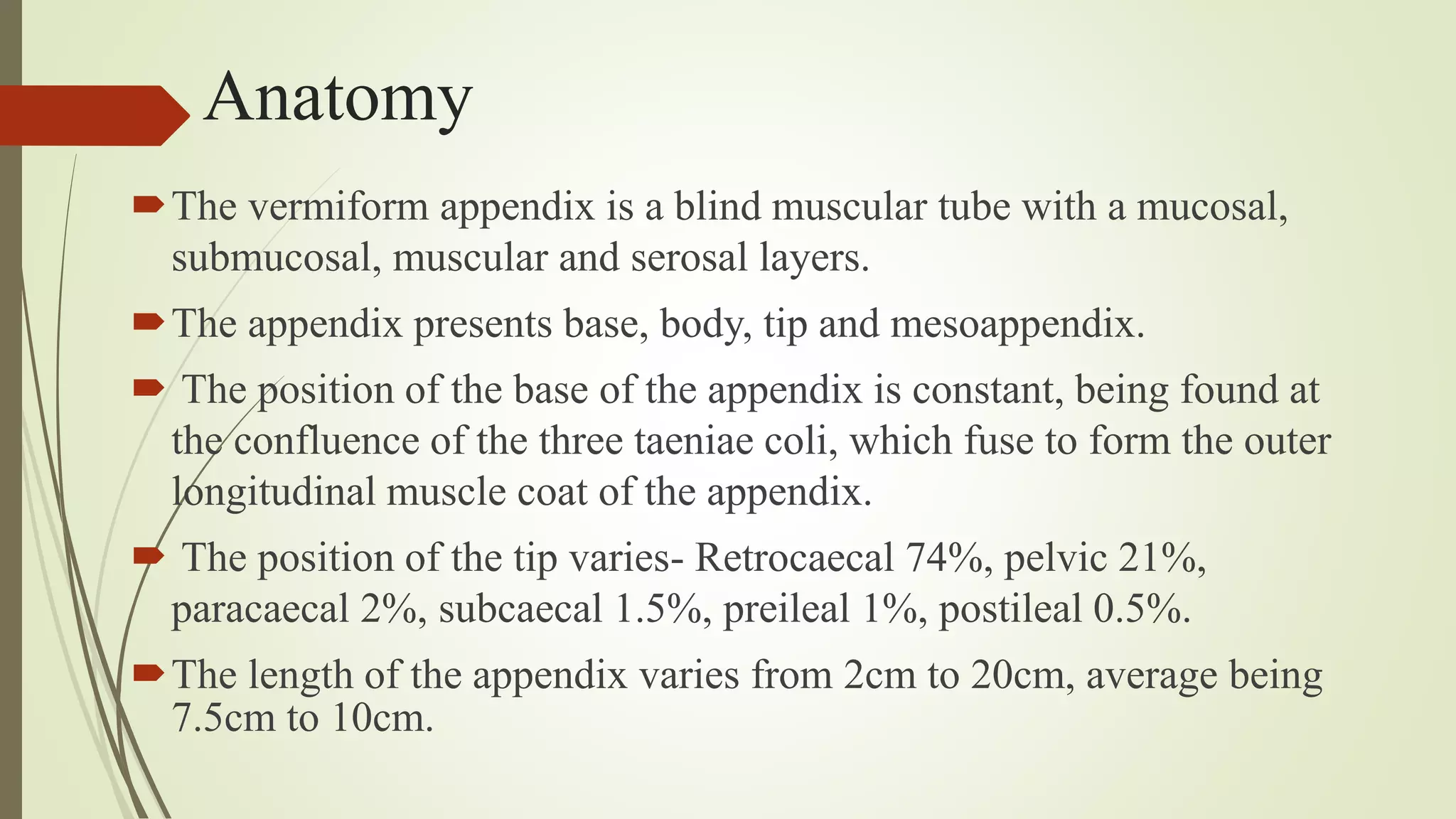
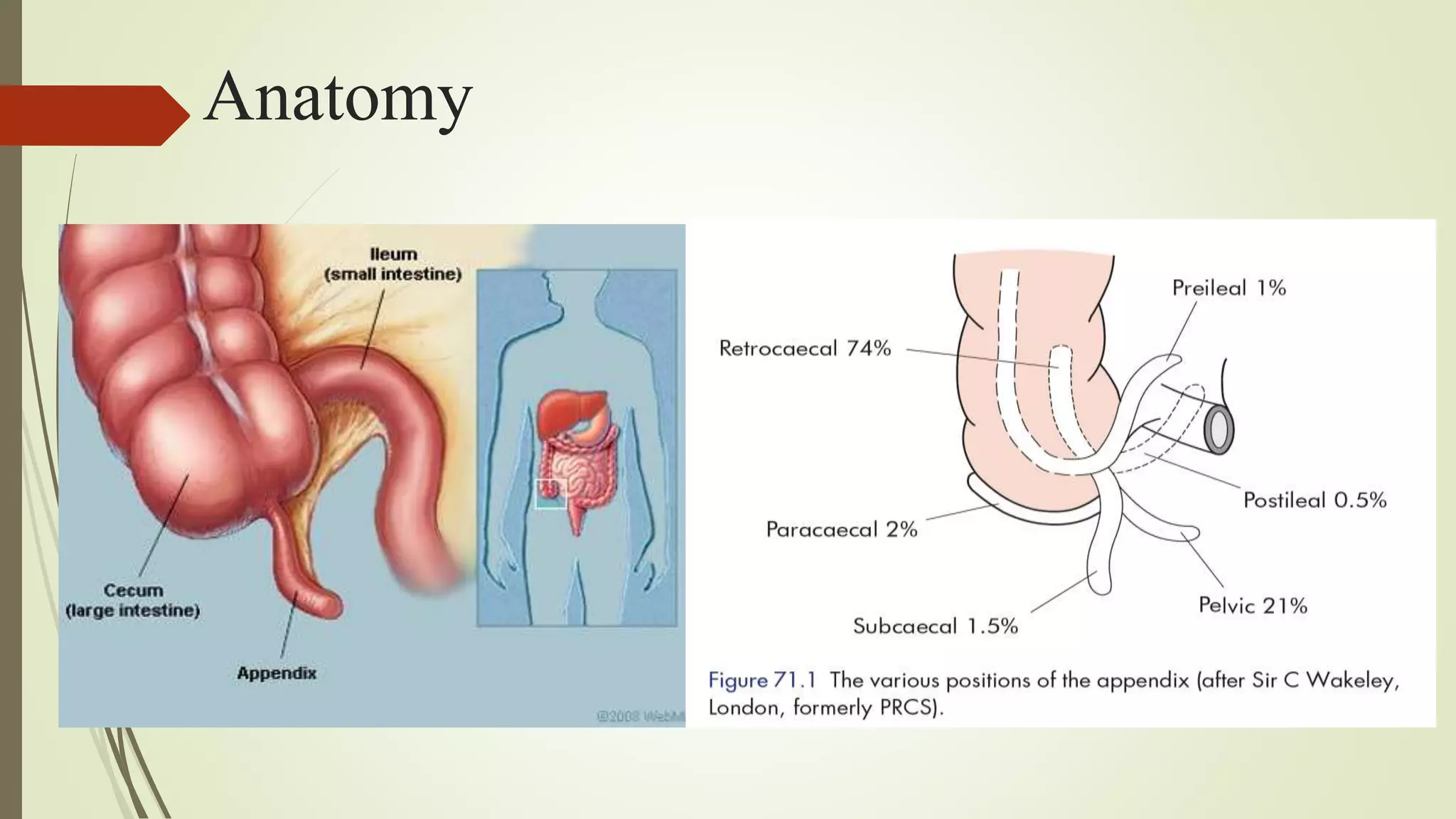
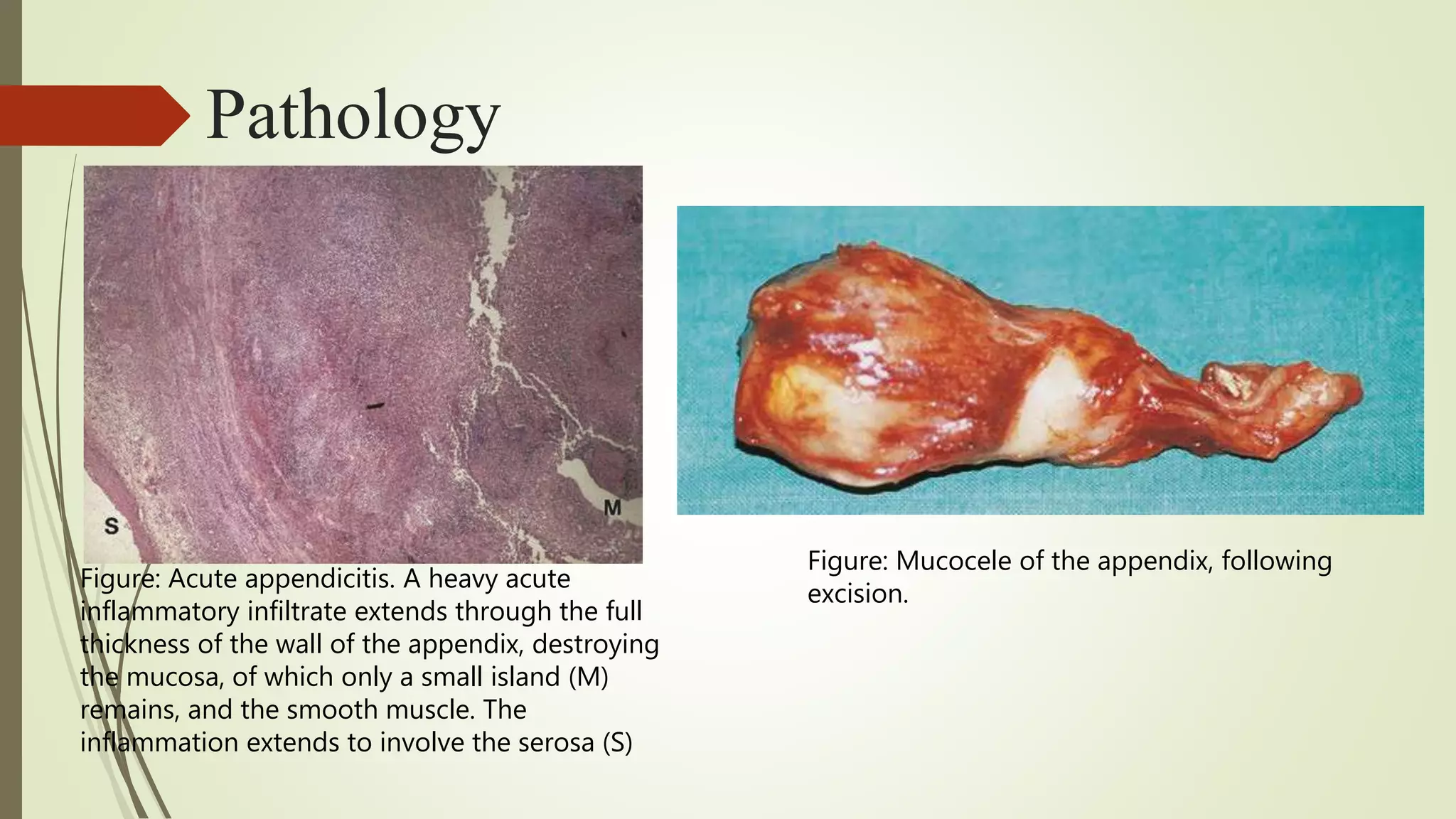
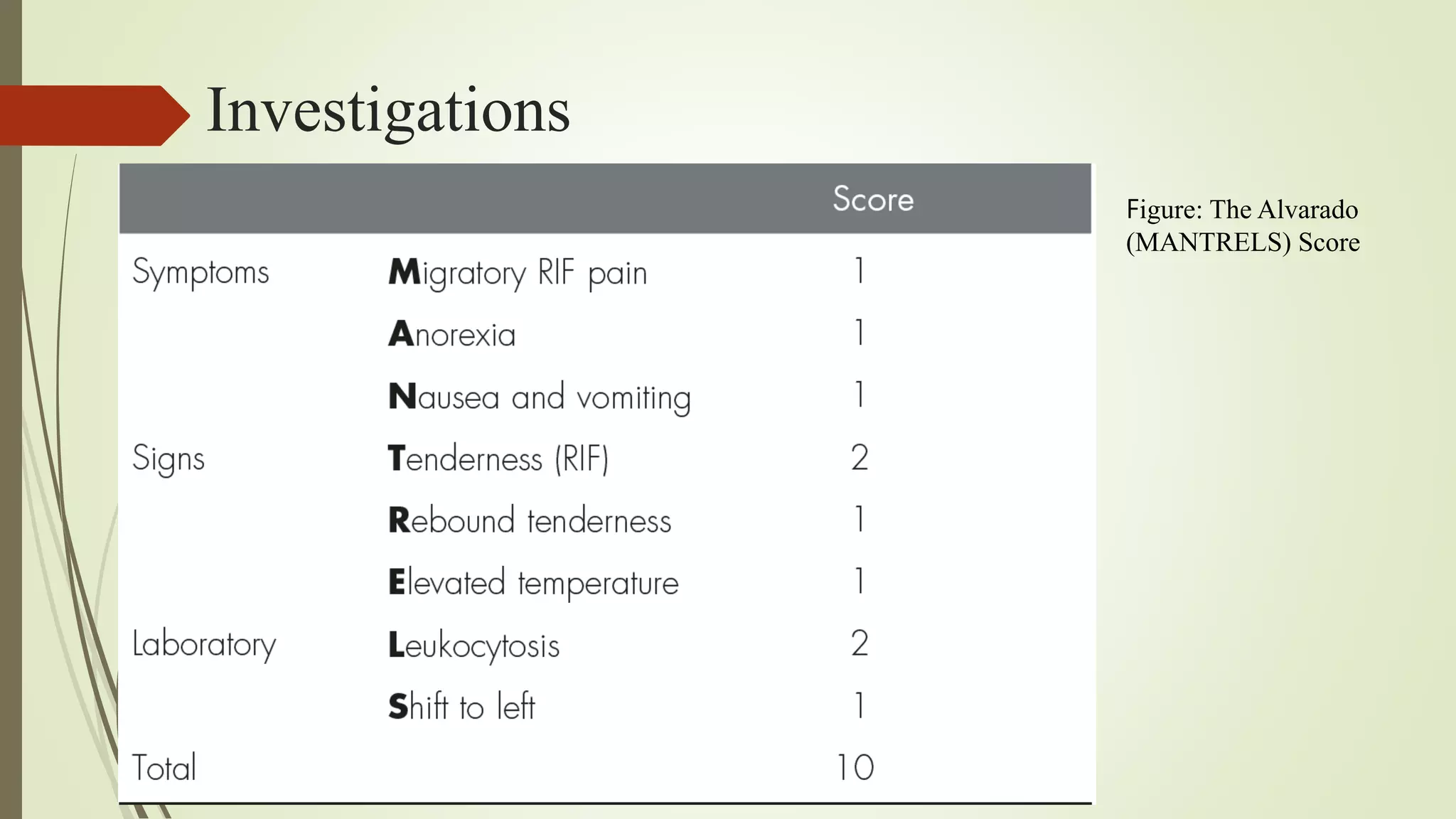
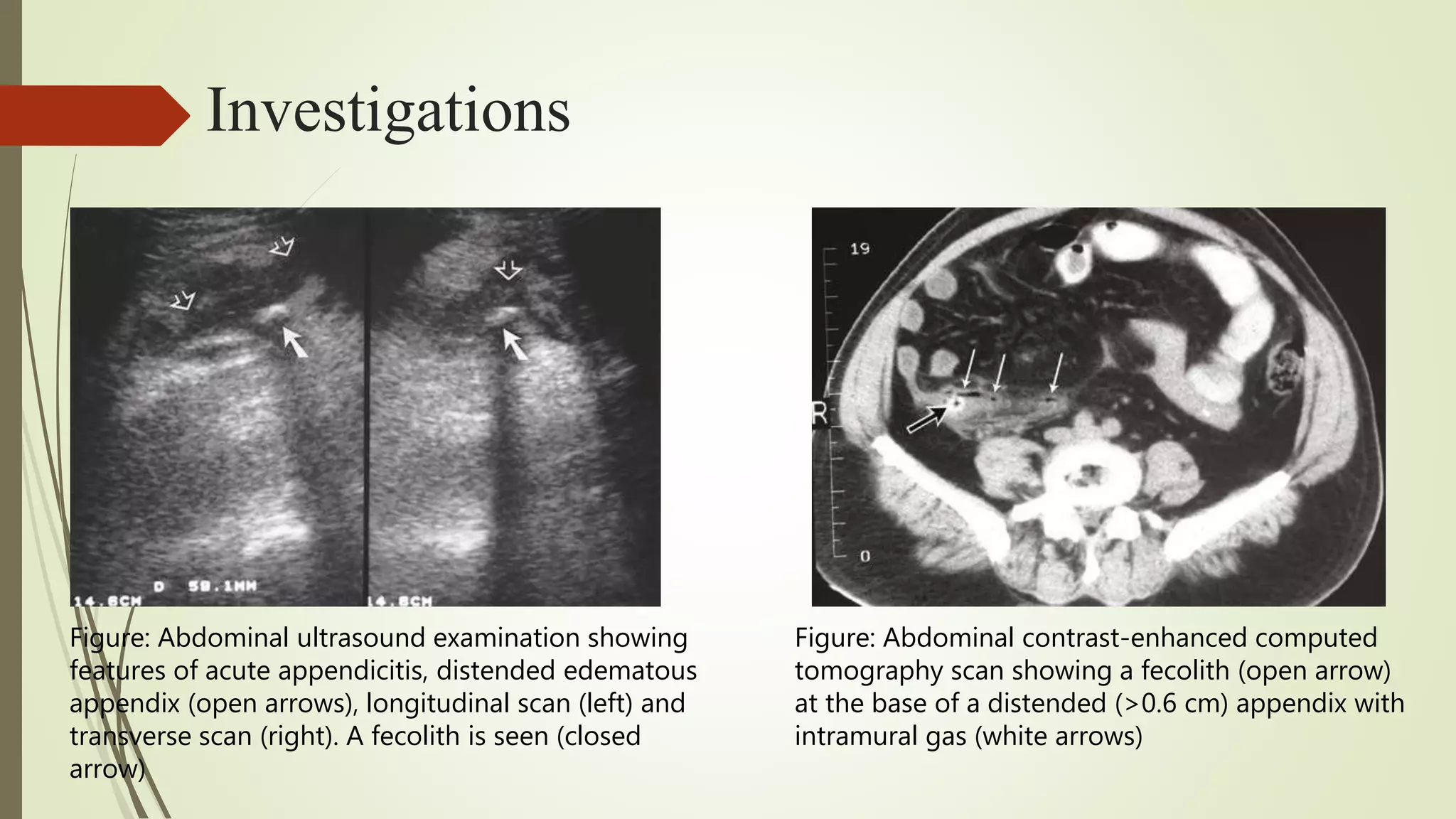
The vermiform appendix is primarily known for its role in acute appendicitis, a common surgical emergency, particularly in young adults. The document covers the embryology, anatomy, and clinical significance of the appendix, emphasizing its pathology during appendicitis and the surgical approaches to appendicectomy. Additional details include the various complications, potential neoplasms, and the importance of accurate diagnosis and management in appendiceal conditions.