This document discusses the evaluation and management of abdominal pain using imaging modalities. It covers:
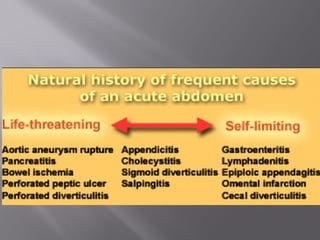
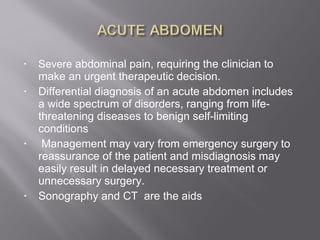
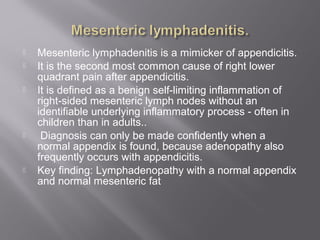
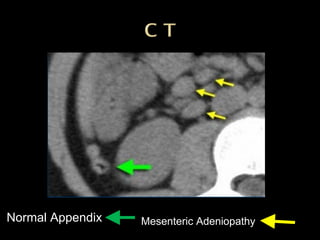
1) Differential diagnosis for acute abdomen is wide, ranging from life-threatening to benign conditions. Management varies from emergency surgery to reassurance depending on diagnosis.
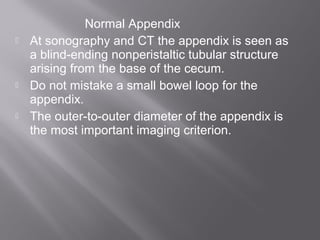
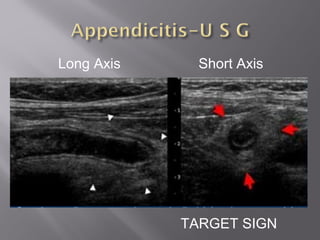
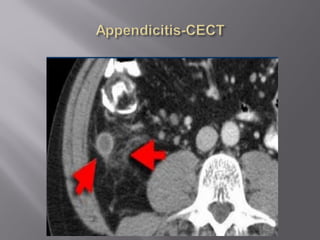
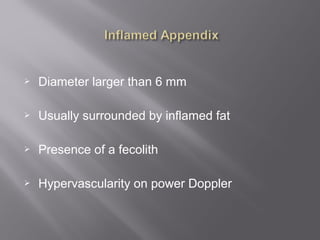
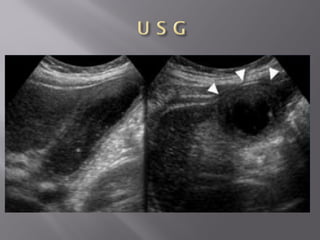
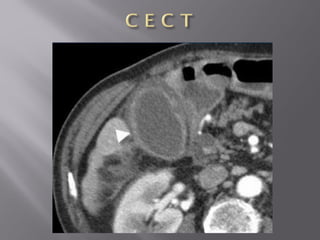
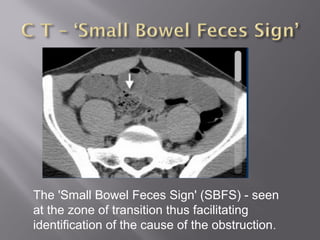
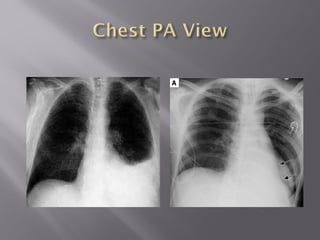
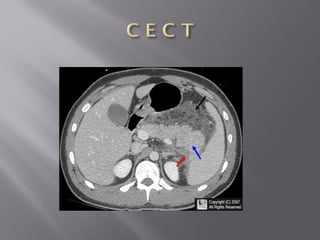
2) Sonography and CT are important aids but findings may be normal in urgent cases or abnormal without surgical disease.
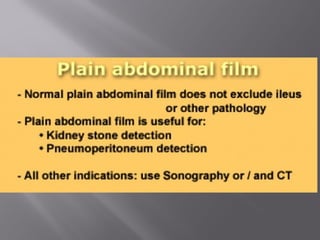
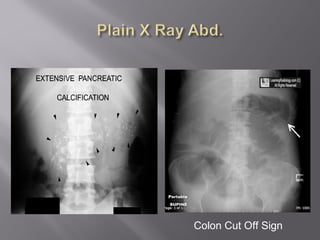
3) A plain abdominal x-ray has limited value and may falsely reassure as normal does not rule out pathology.
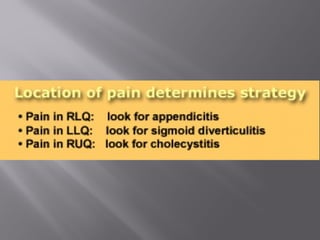
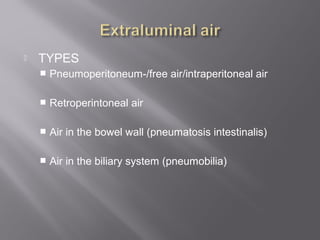
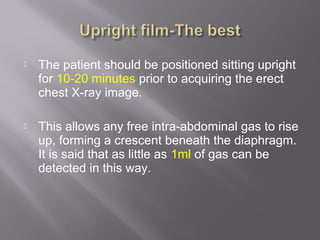
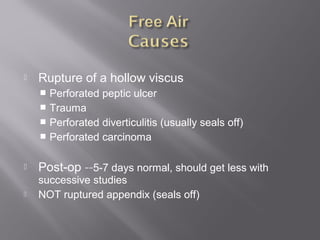
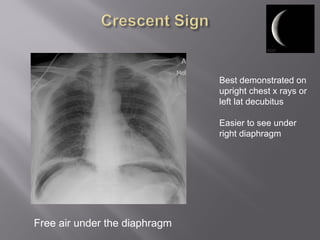
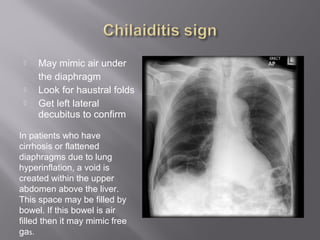
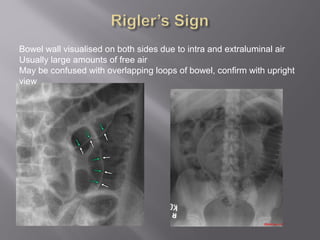
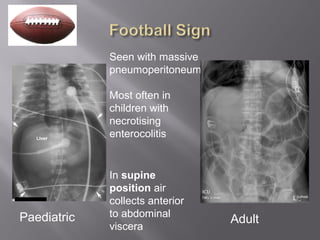
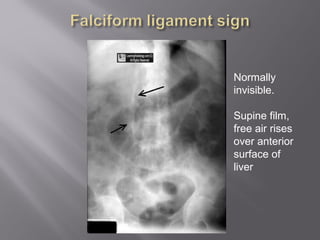
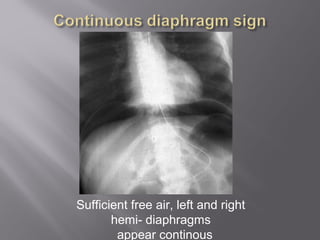
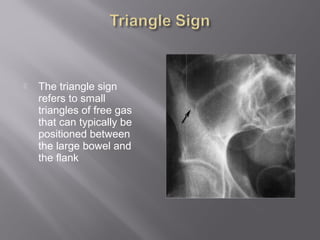
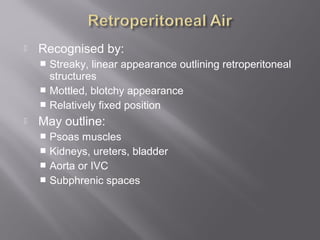
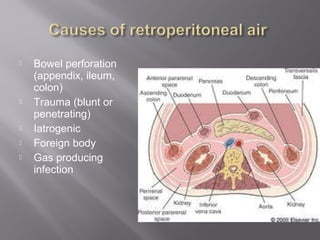
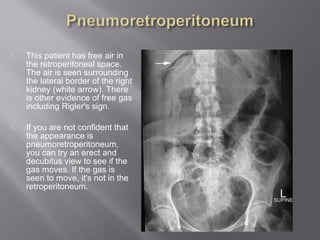
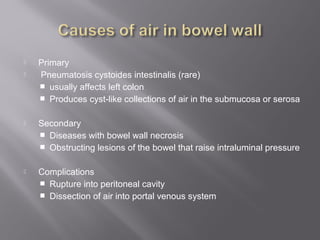
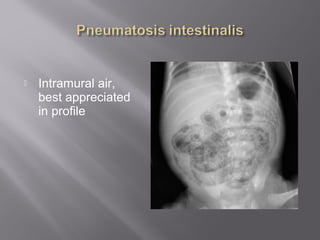
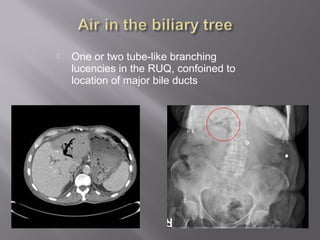
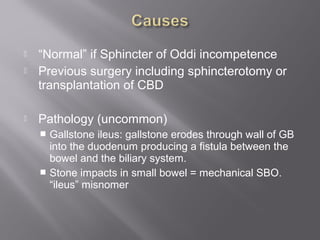
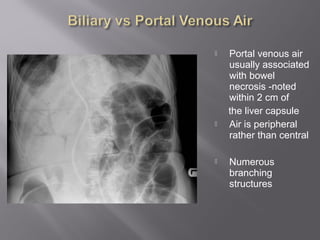
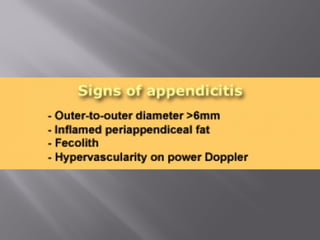
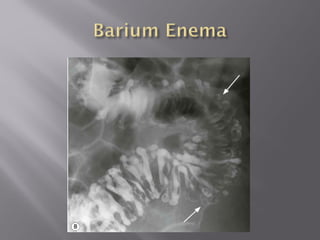
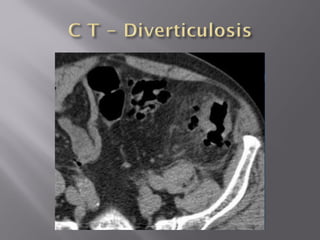
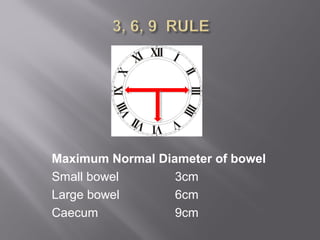
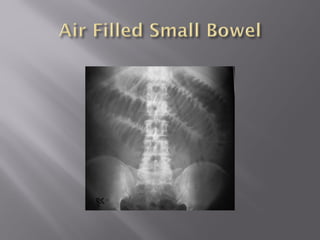
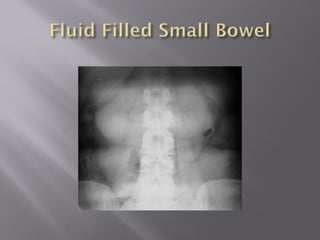
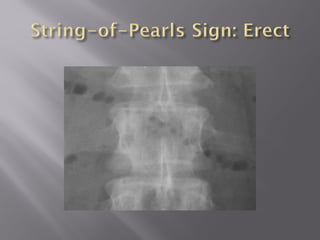
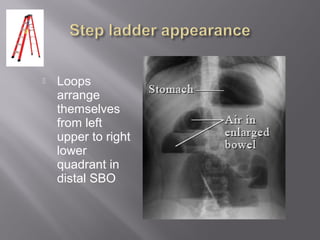
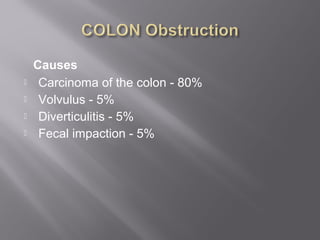
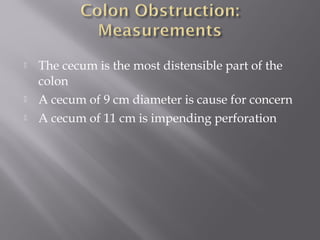
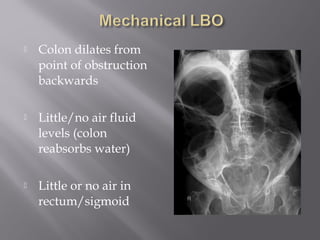
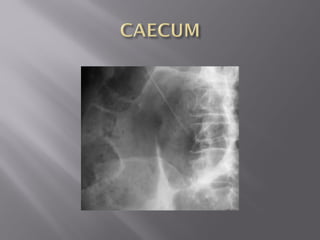
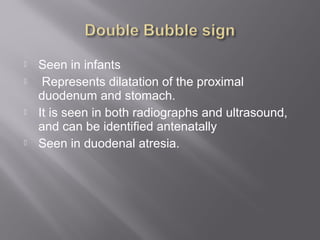
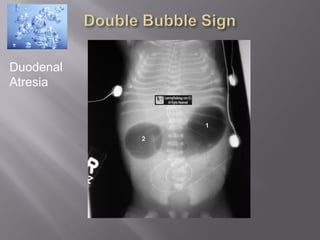
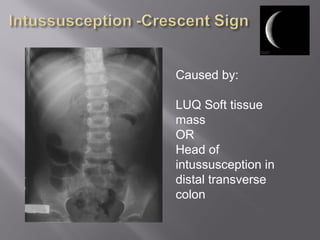
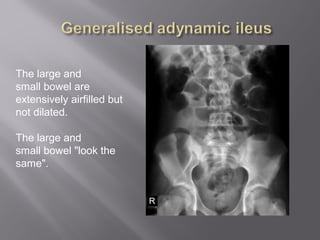
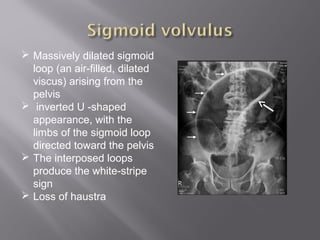
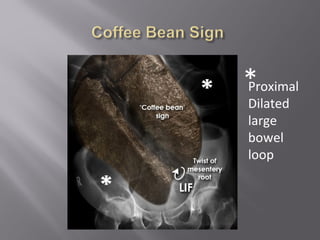
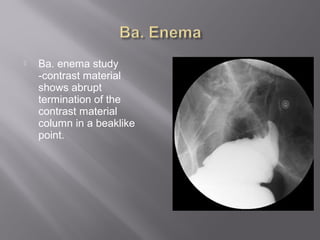
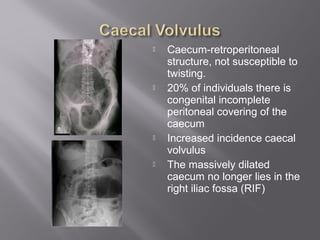
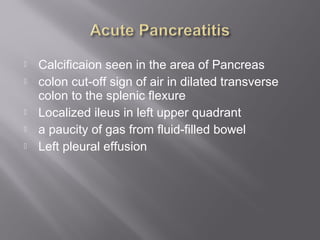
4) The document then discusses various x-ray findings that help diagnose conditions like perforation, obstruction, appendicitis, diverticulitis, and others.