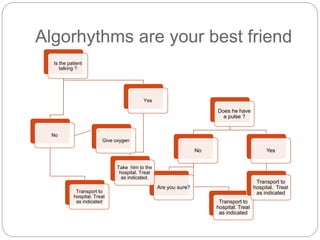
This document provides an overview of algorithms and treatments for common cardiac conditions paramedics may encounter, including:
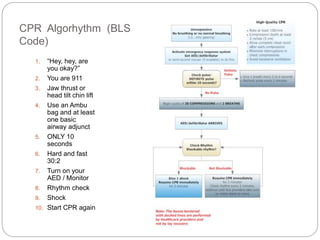
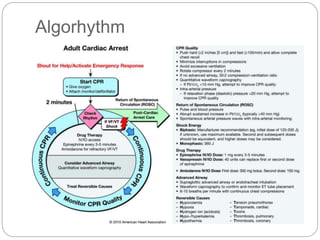
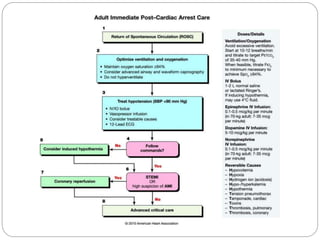
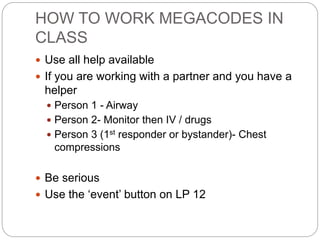
1. The CPR algorithm outlines the basic steps for assessing and treating a patient in cardiac arrest.
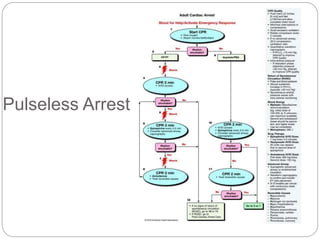
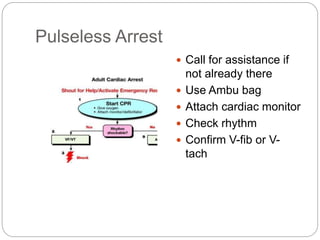
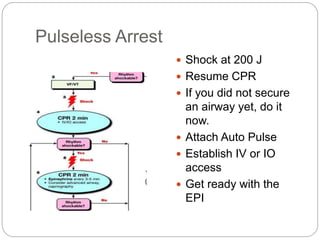
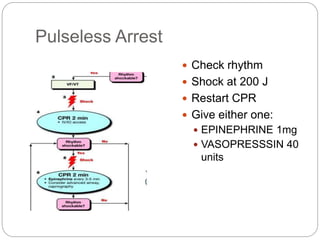
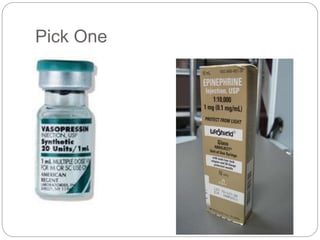
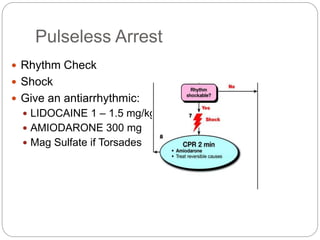
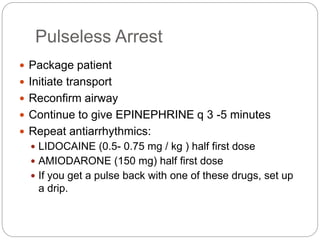
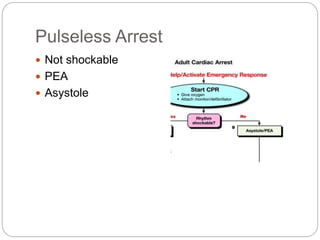
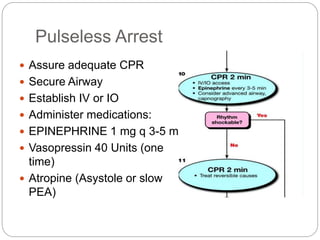
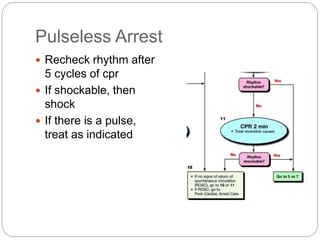
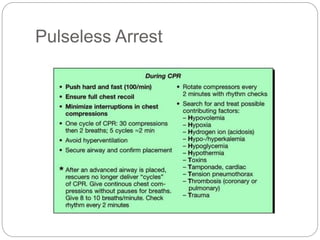
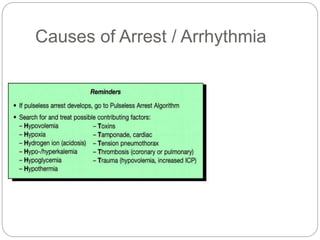
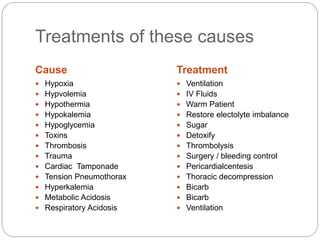
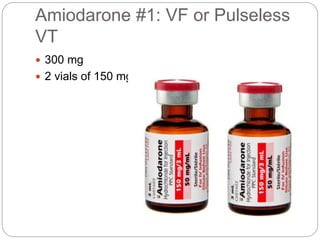
2. The pulseless arrest algorithm details the treatment sequence for a patient without a pulse, including establishing an airway, defibrillation, CPR, IV/IO access, and medication administration.
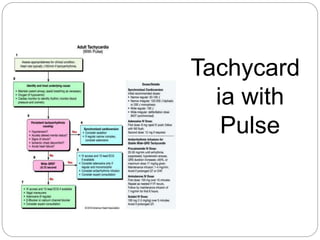
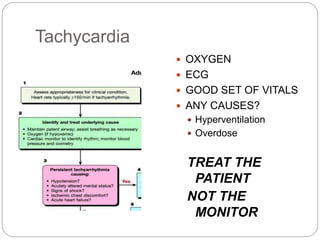
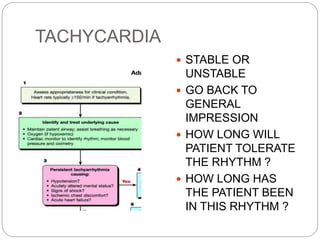
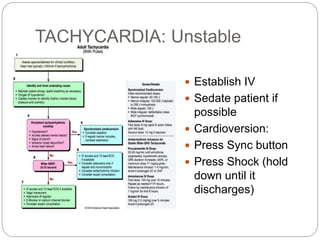
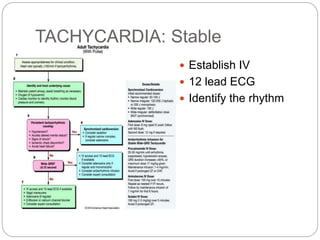
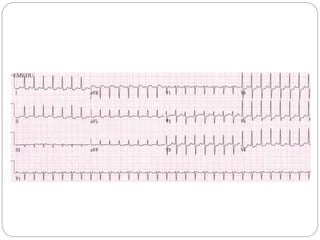
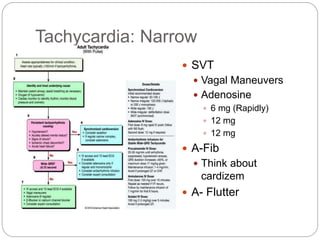
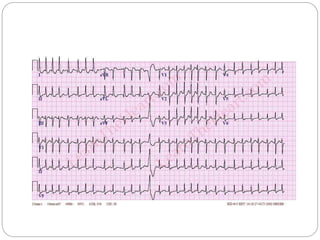
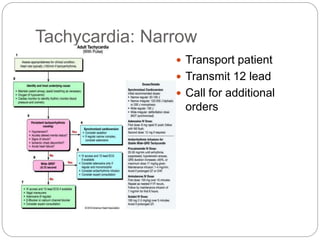
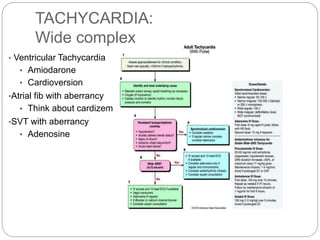
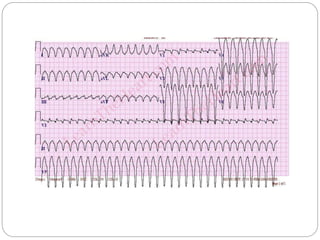
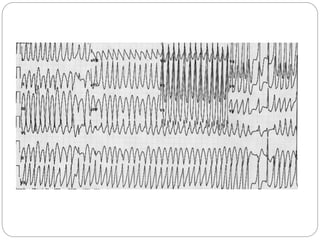
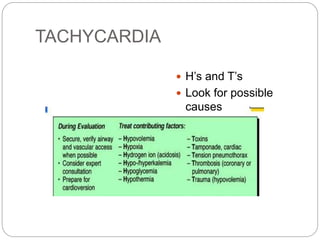
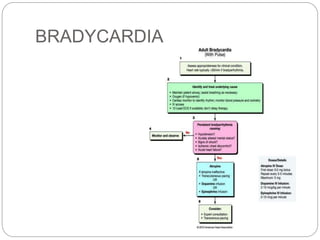
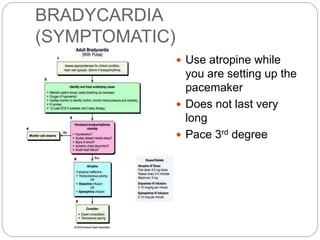
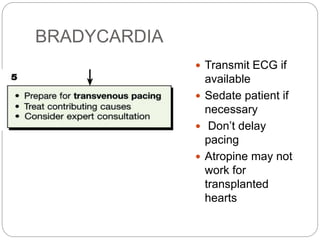
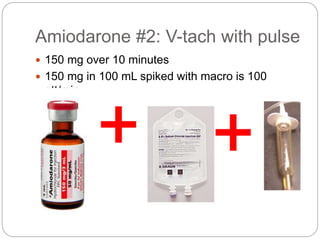
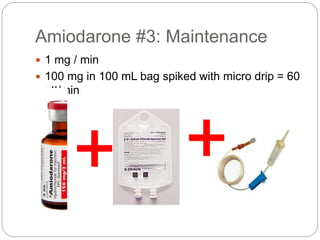
3. Algorithms are provided for tachycardia with a pulse (stable vs. unstable), narrow vs. wide complex tachycardia, and bradycardia. Treatment options like cardioversion, vagal maneuvers, adenosine, and pacing are discussed.
4