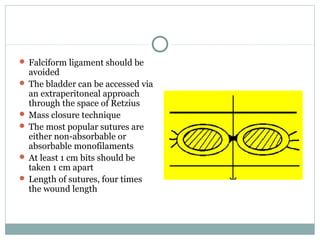
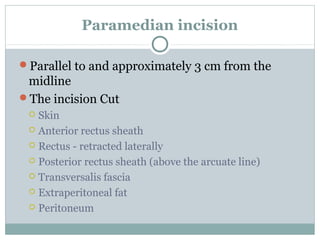
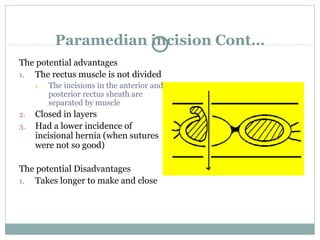
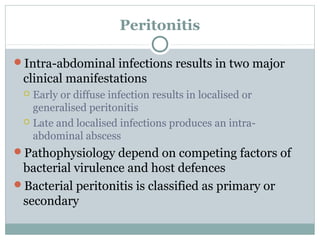
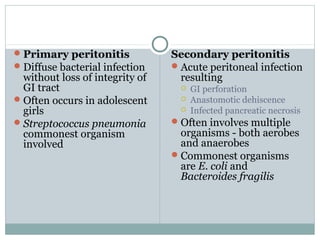
This document discusses abdominal incisions and the management of peritonitis and intra-abdominal abscesses. It describes the midline and paramedian incisions for abdominal access. It defines primary and secondary peritonitis and discusses the surgical management including source control, reducing bacterial contamination, and preventing recurrent infection. It also outlines the clinical features and management of intra-abdominal abscesses.