The document provides an overview of the anatomy of the abdomen, including:
1) It describes the surface anatomy of the abdomen using planes and regions.
2) It details the layers of the anterior abdominal wall including muscles and fascia.
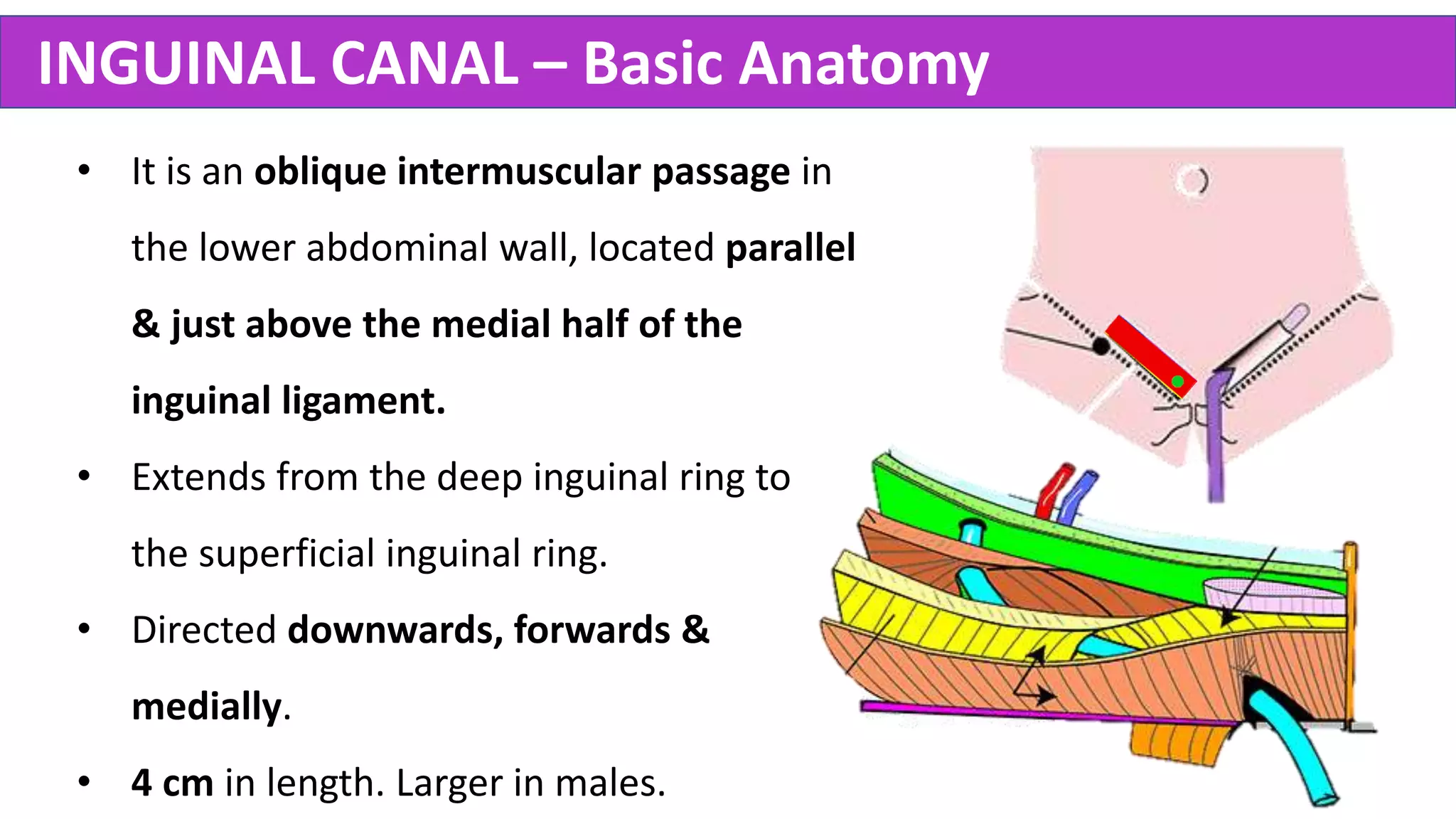
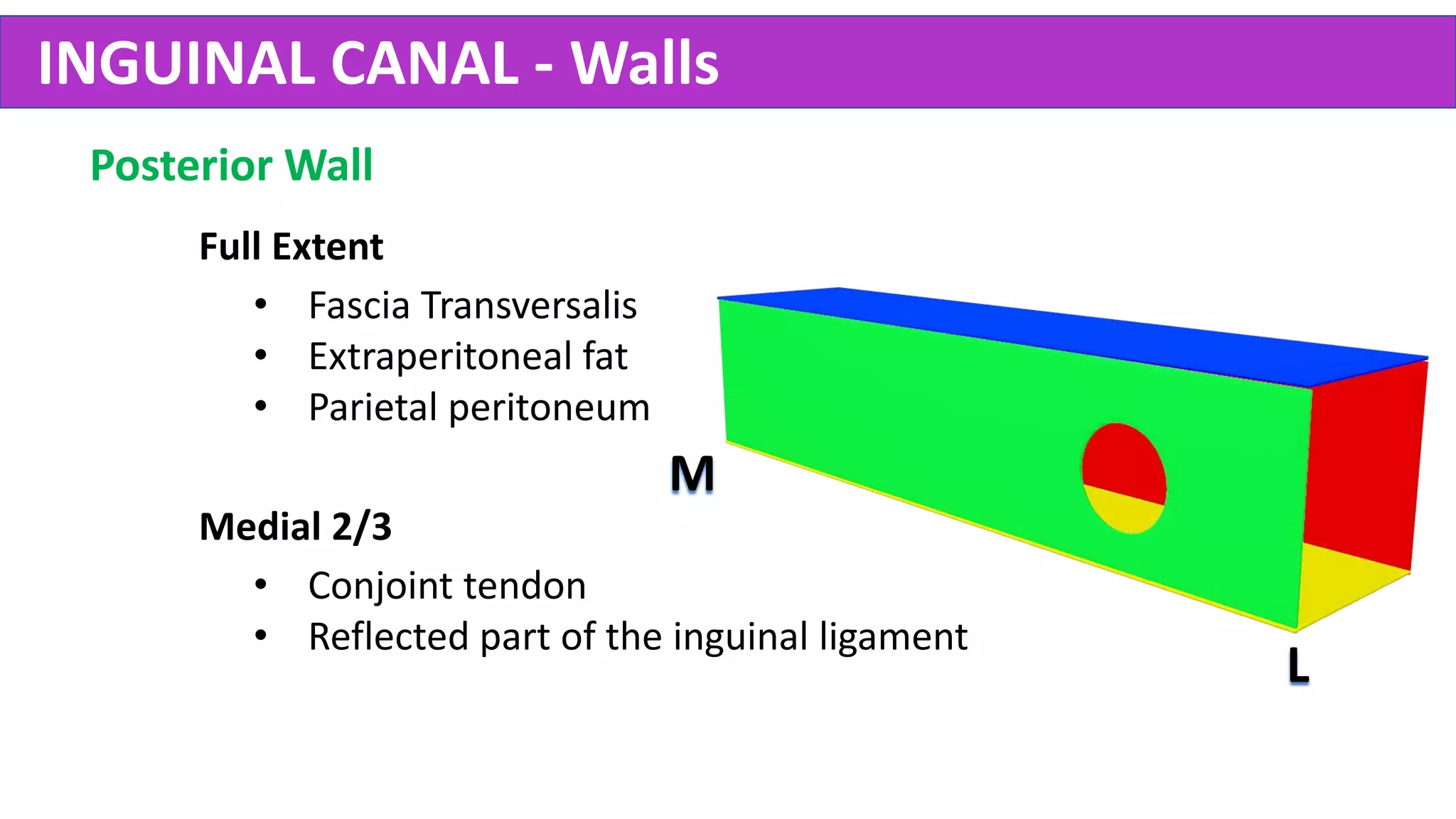
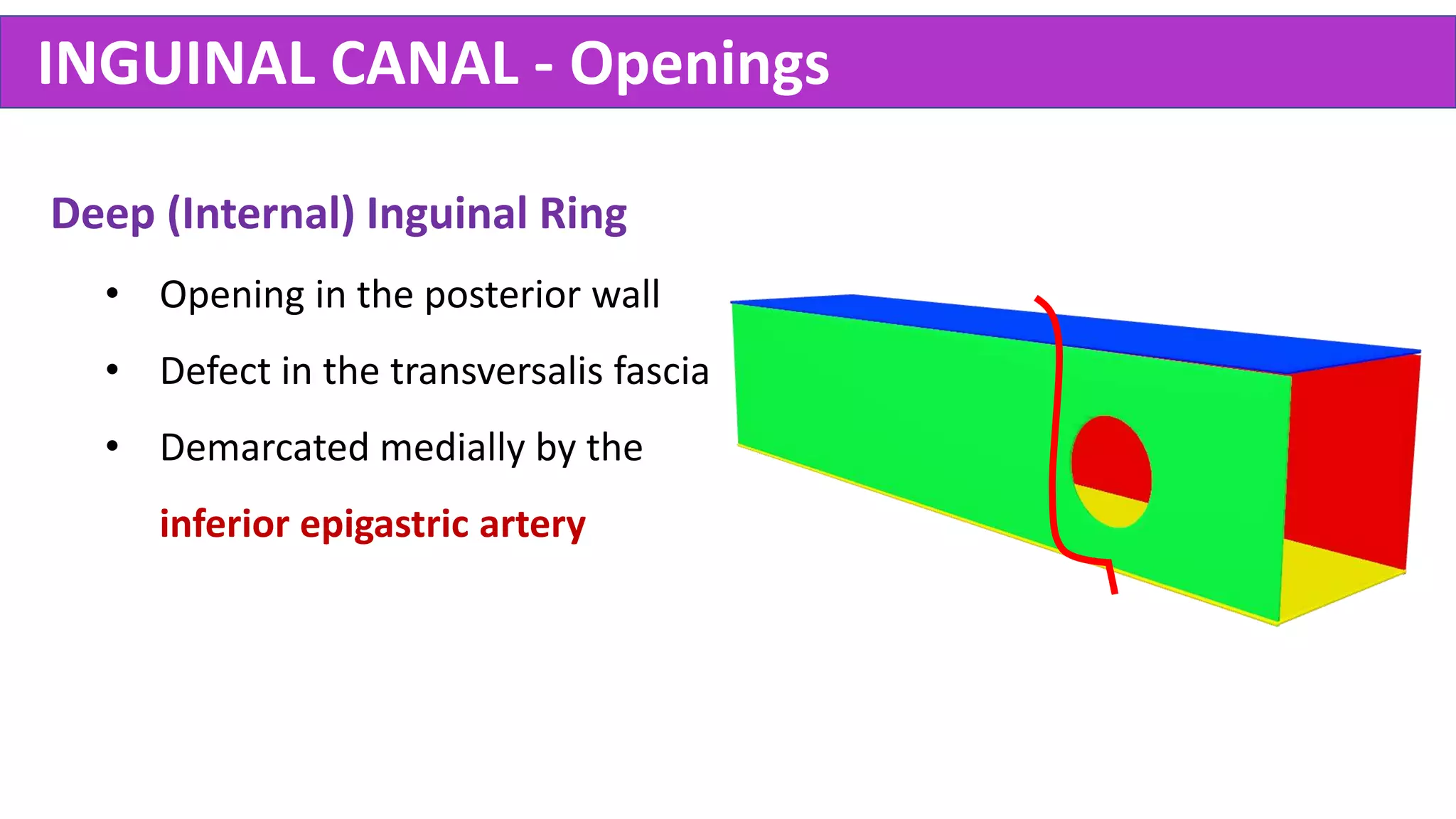
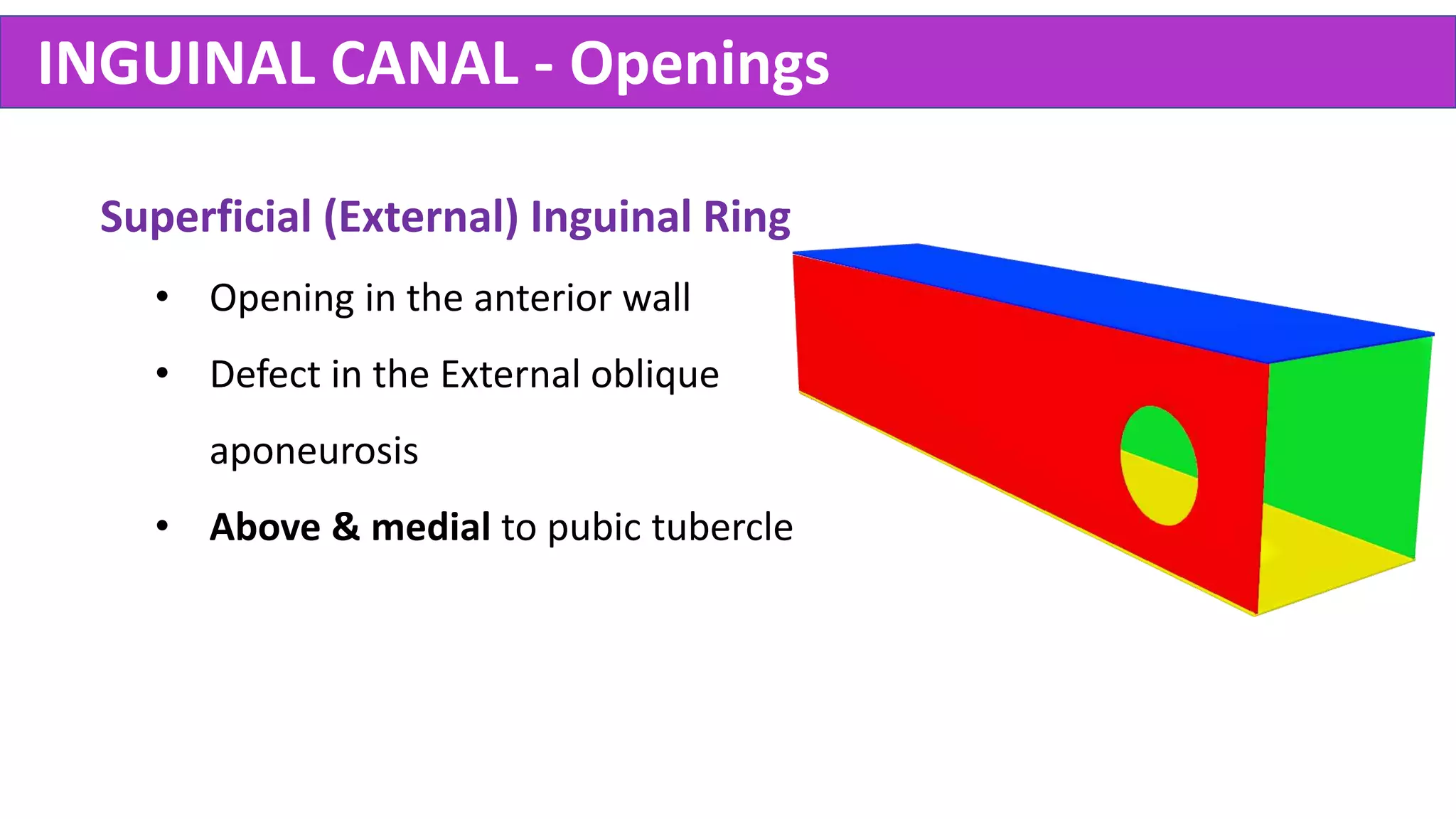
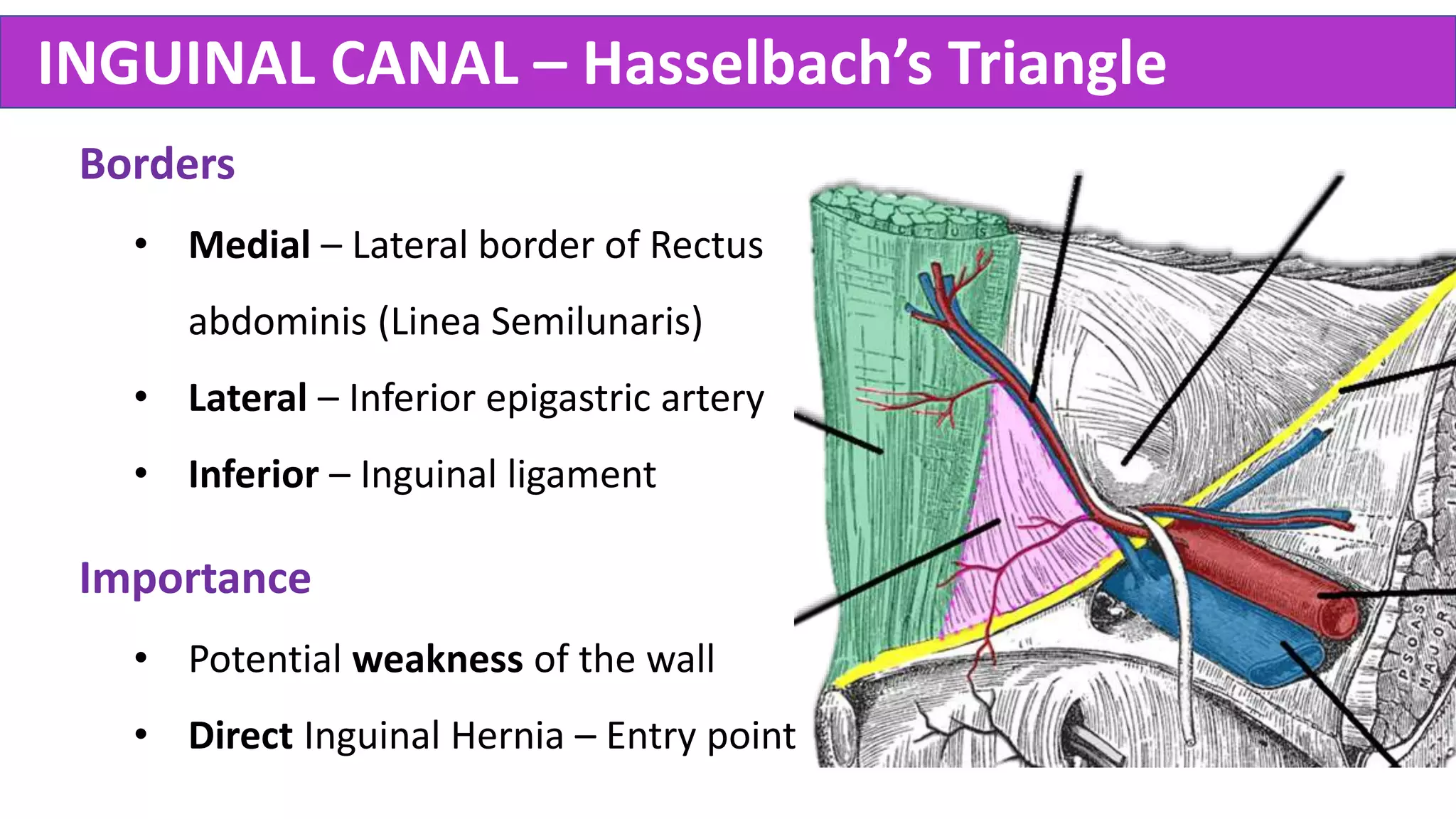
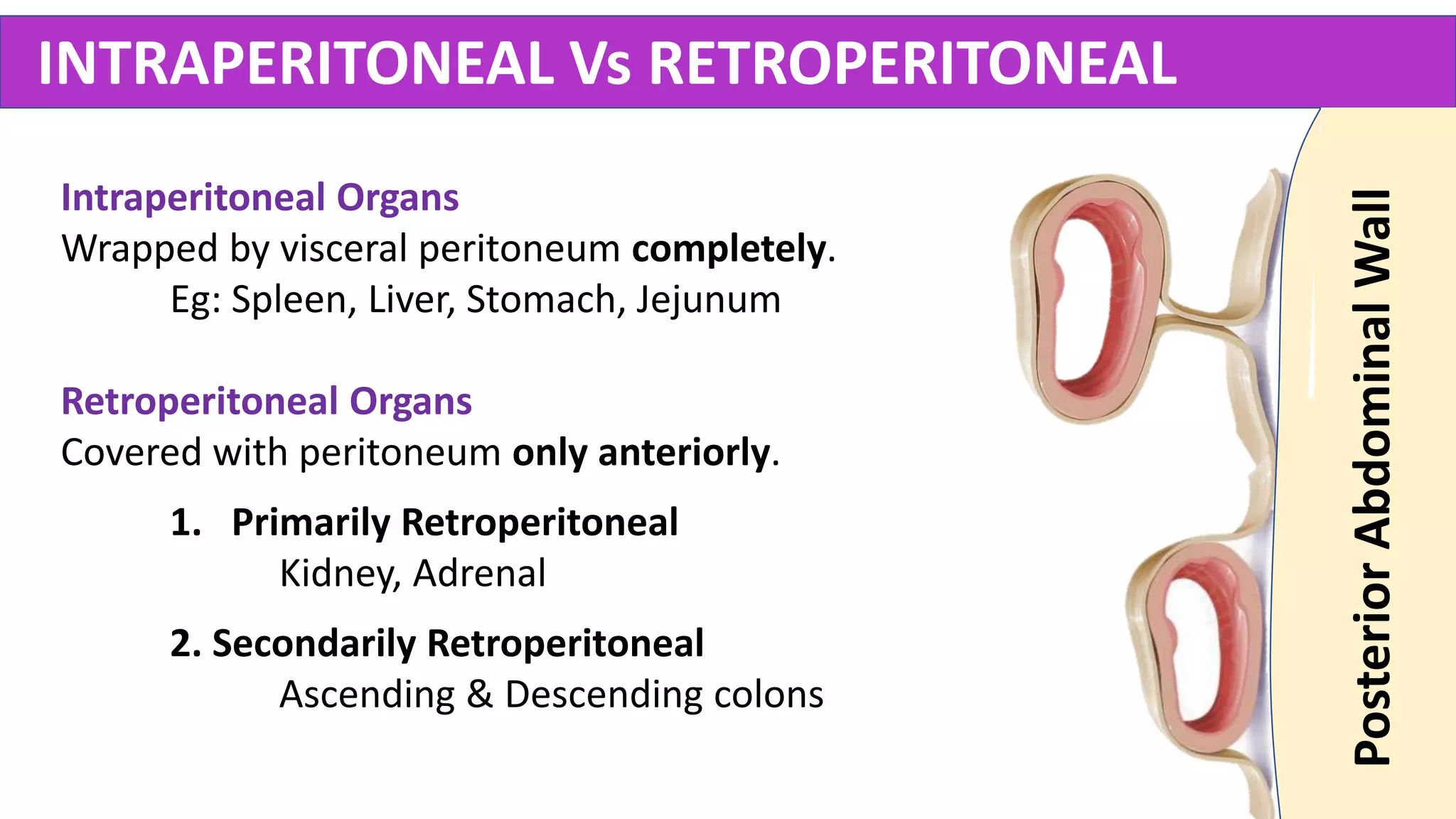
3) It explains the anatomy of the inguinal canal including its walls, openings, contents and Hasselbach's triangle.
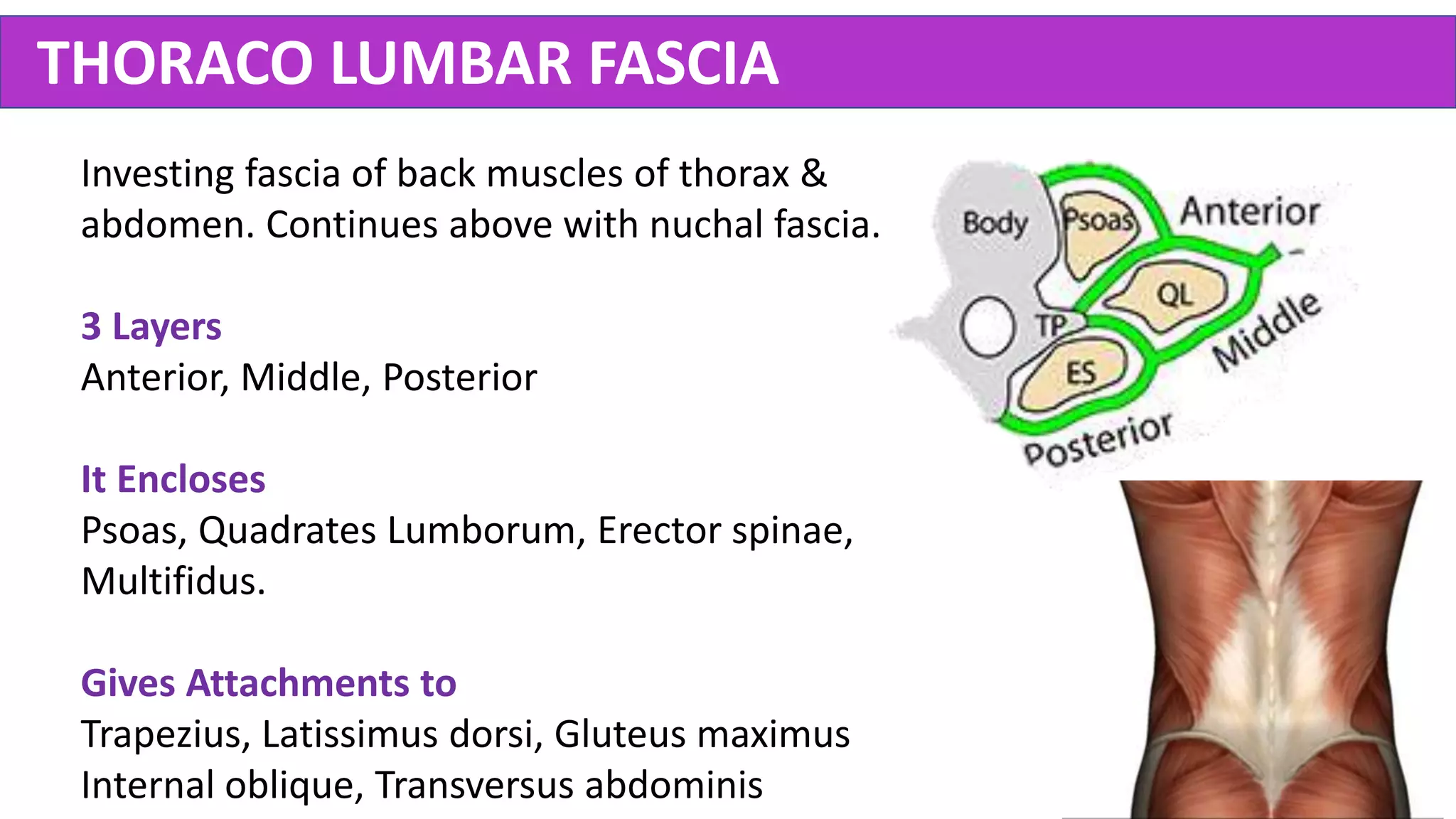
4) It briefly outlines the muscles and fascia of the posterior abdominal wall.