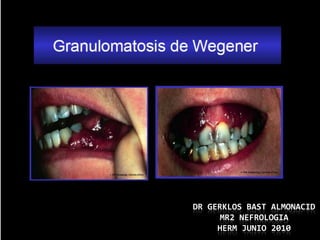
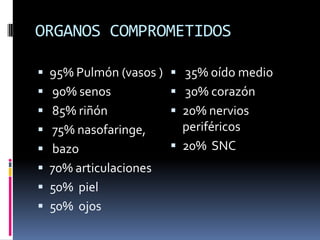
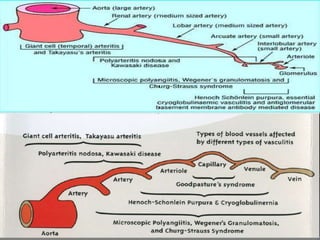
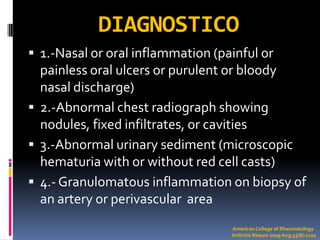
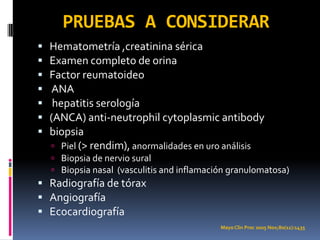
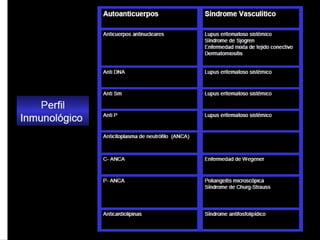
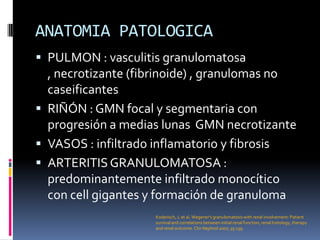
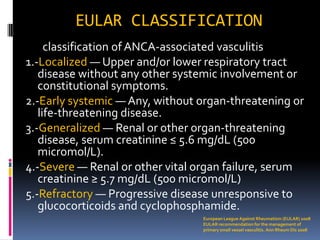
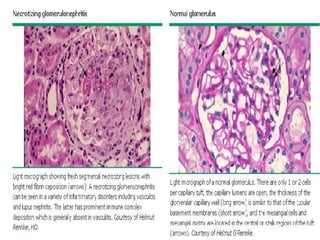
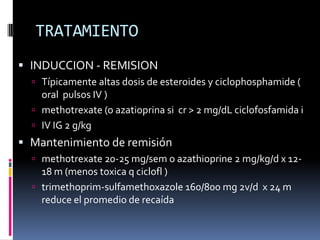
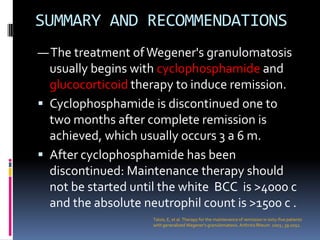
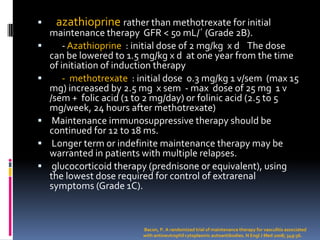
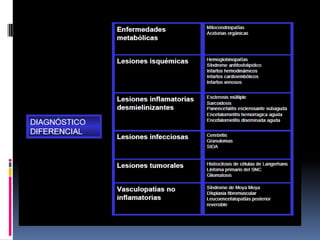
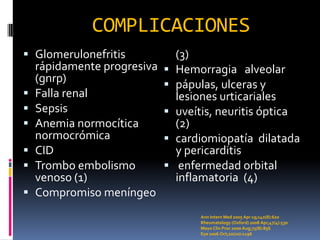
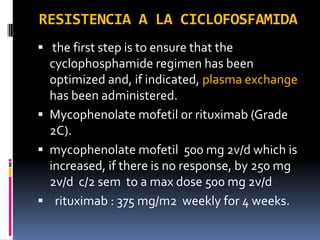
The document summarizes Wegener's granulomatosis (WG), a rare necrotizing vasculitis that commonly involves the respiratory tract and kidneys. It describes the pathogenesis as a type III hypersensitivity reaction mediated by immune complexes. Treatment typically involves cyclophosphamide and glucocorticoids to induce remission, followed by azathioprine or methotrexate as maintenance therapy to sustain remission for 12-18 months. Complications can include rapidly progressive glomerulonephritis, renal failure, and other organ involvement.