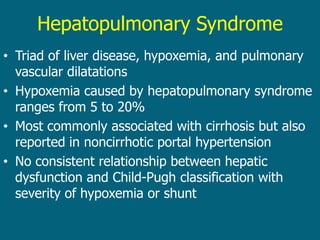
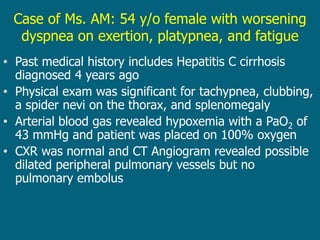
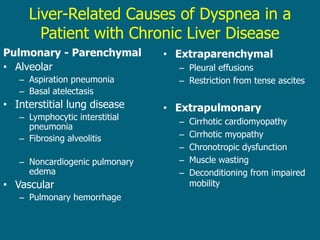
This document discusses hepatopulmonary syndrome (HPS), a condition characterized by liver disease, hypoxemia, and pulmonary vascular dilatations. HPS causes hypoxemia ranging from 5-20% and is most commonly associated with cirrhosis. Orthotopic liver transplantation is currently the only effective treatment for HPS as it resolves the hypoxemia. Screening for HPS with arterial blood gases is recommended for patients with chronic liver disease reporting dyspnea.