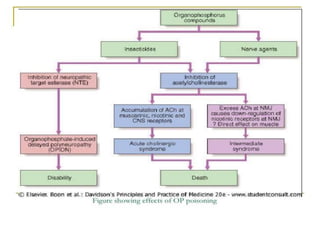
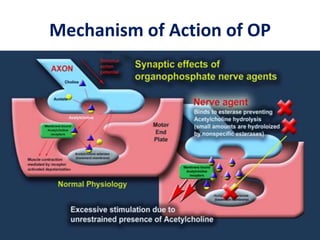
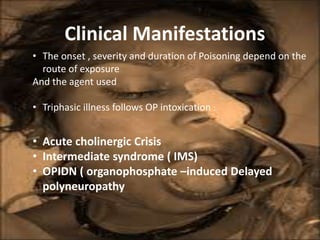
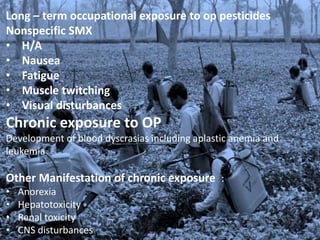
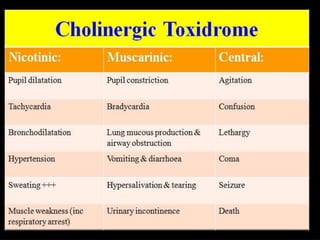
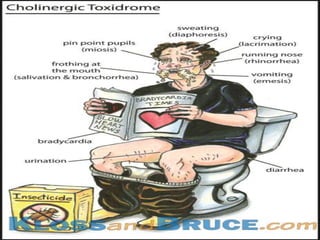
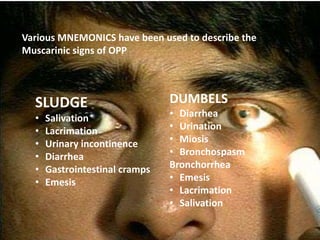
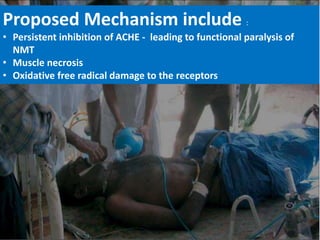
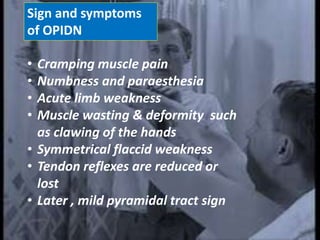
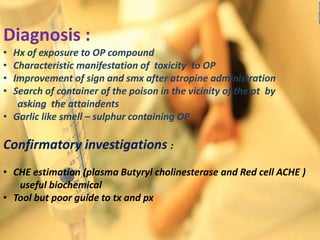
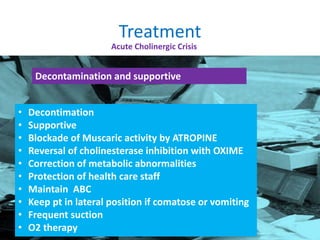
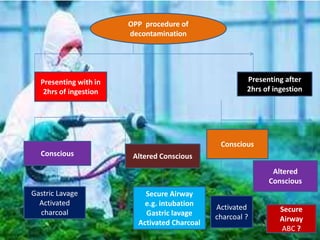
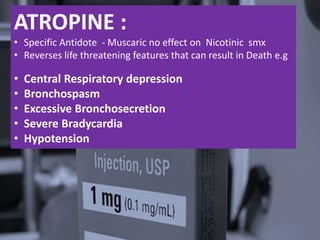
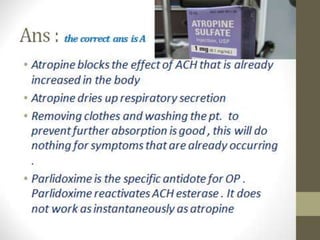
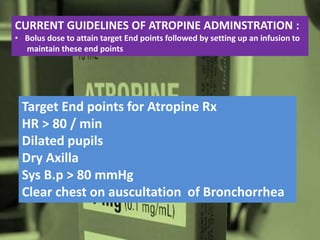
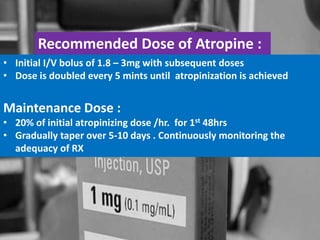
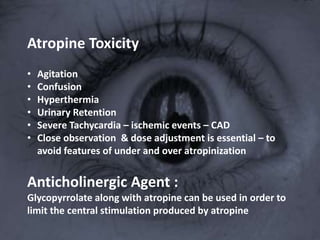
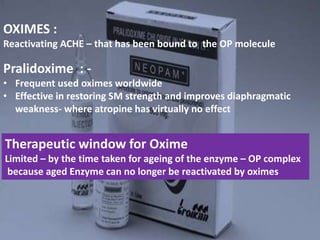
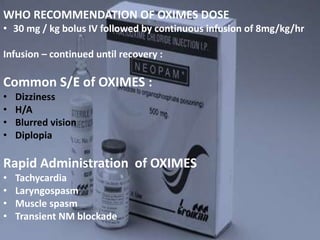
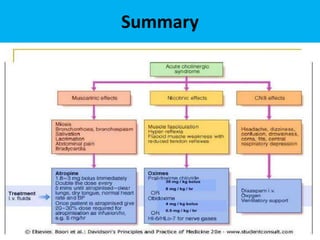
The document discusses the use and effects of organophosphates (OP) in poisoning cases, including symptoms, diagnosis, and treatment protocols. It highlights the clinical manifestations arising from acute, intermediate, and delayed exposure, emphasizing the need for immediate management and specific agents like atropine and oximes for treatment. Long-term exposure risks and strategies for recovery and prevention of complications are also addressed.