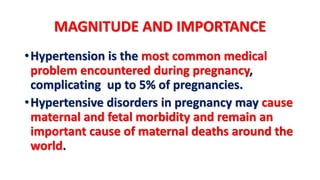
1. Hypertension is a common medical complication during pregnancy, affecting up to 5% of pregnancies. It can cause morbidity for both the mother and fetus.
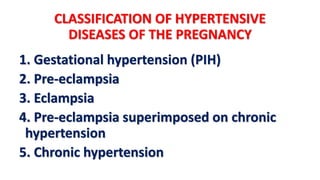
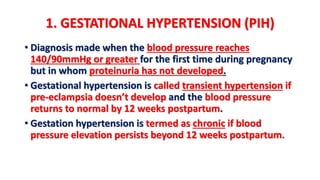
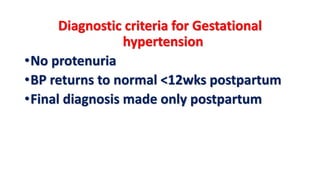
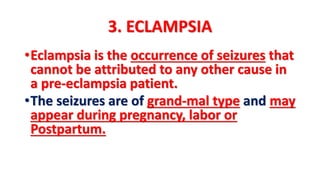
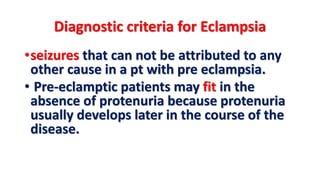
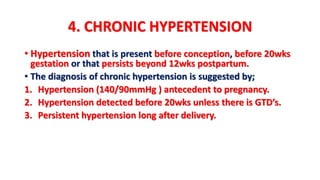
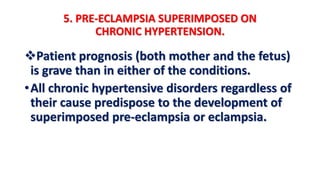
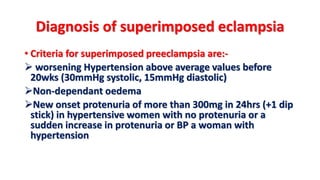
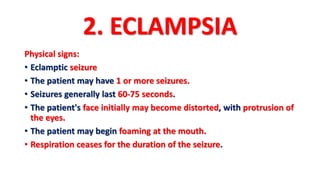
2. There are several classifications of hypertensive disorders of pregnancy, including gestational hypertension, preeclampsia, eclampsia, chronic hypertension, and preeclampsia superimposed on chronic hypertension.
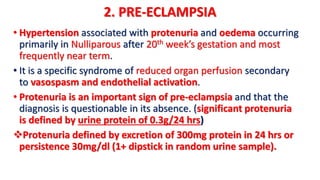
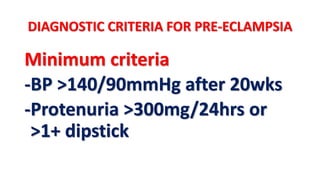
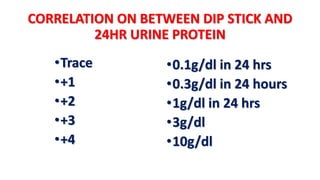
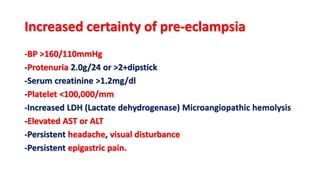
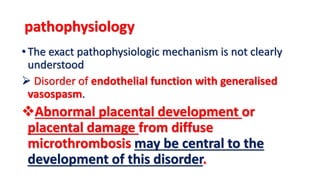
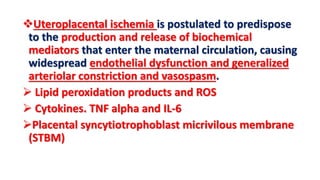
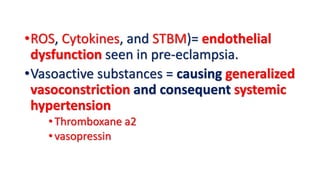
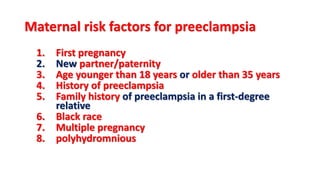
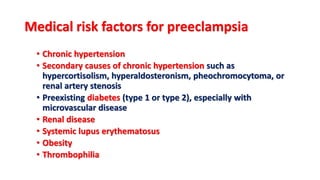
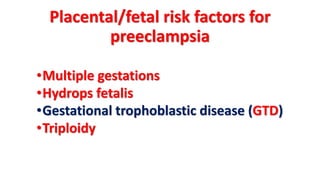
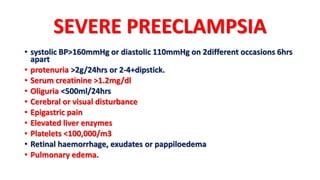
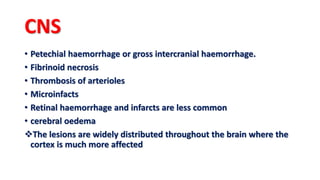
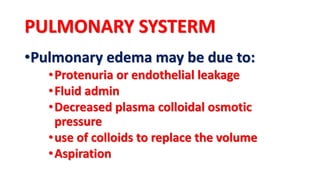
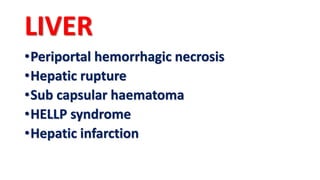
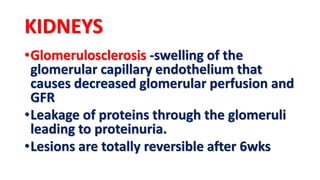
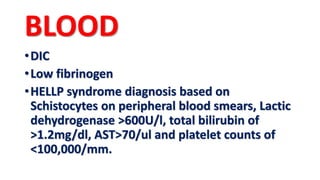
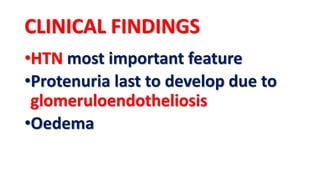
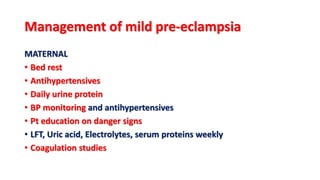
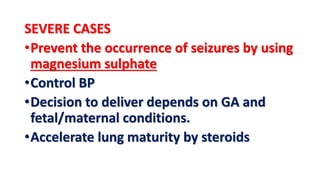
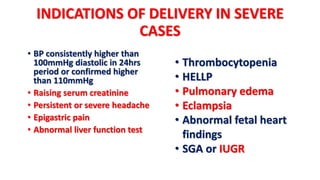
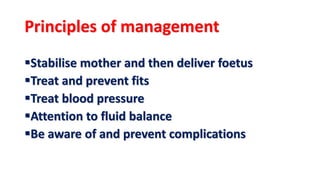
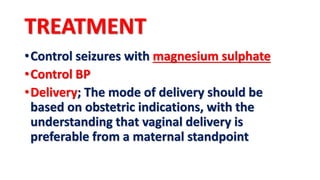
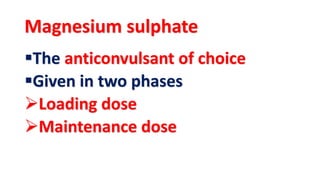
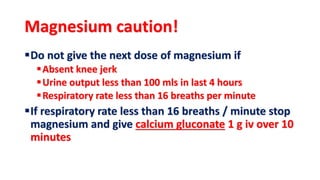
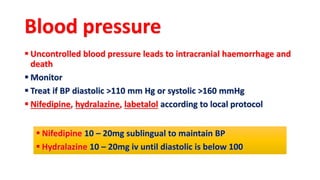
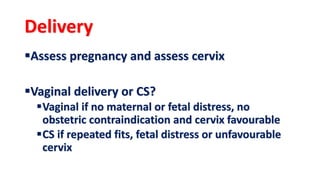
3. Preeclampsia is defined as new onset hypertension and proteinuria after 20 weeks of gestation. It is caused by placental ischemia and endothelial dysfunction leading to widespread vasoconstriction. Management involves monitoring, controlling blood pressure, delivering the baby if conditions warrant, and preventing seizures with magnesium sulfate.