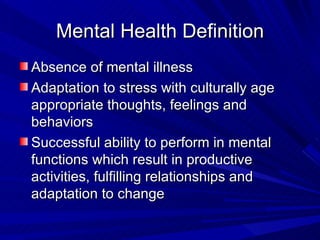
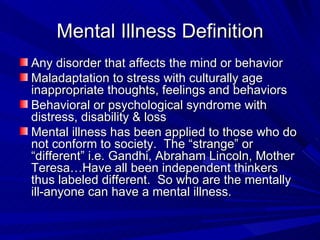
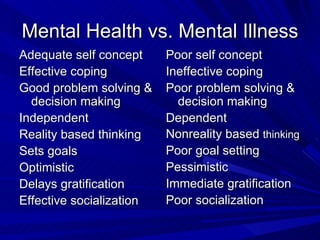
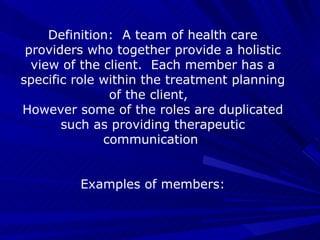
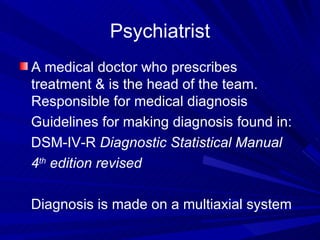
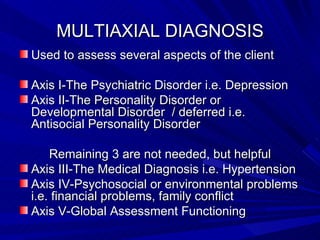
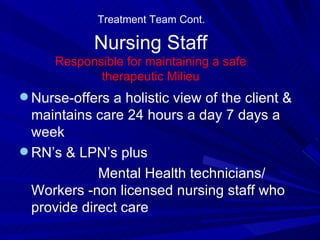
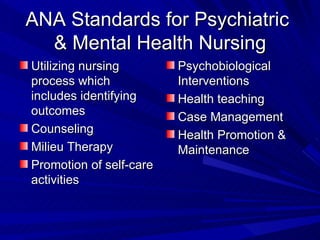
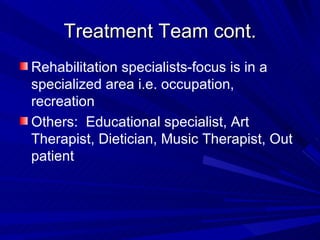
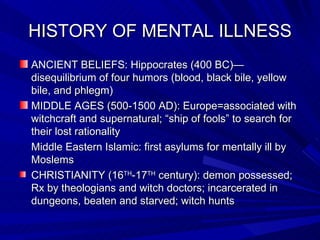
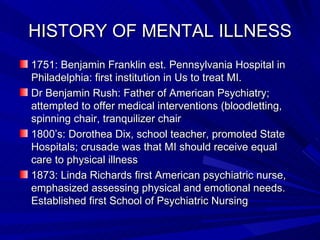
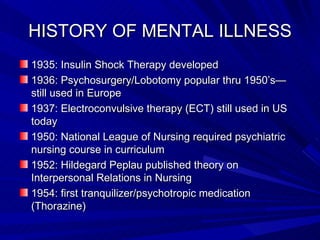
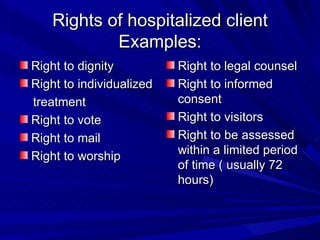
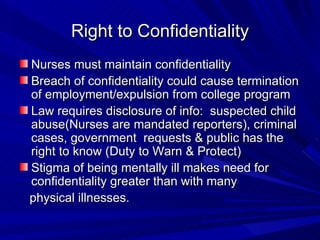
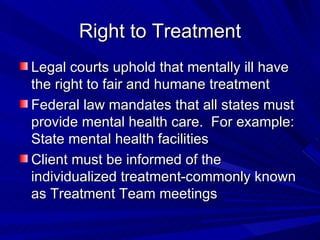
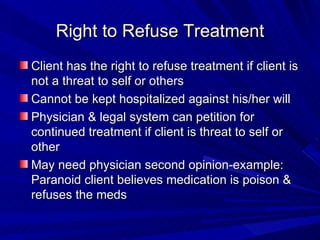
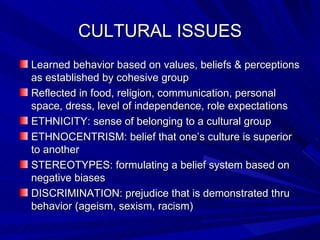
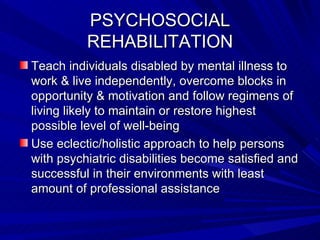
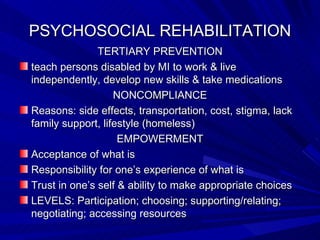
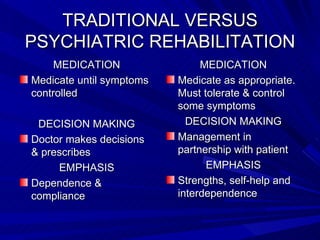
This document provides an overview of psychiatric mental health nursing. It discusses the roles of various members of the interdisciplinary treatment team, including psychiatrists, nurses, psychologists, social workers and more. It also covers topics like the history of mental illness, cultural issues, rights of patients, and psychosocial rehabilitation approaches.