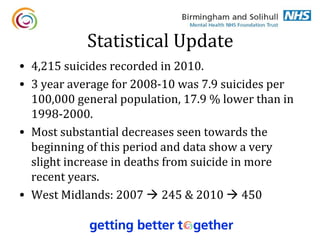
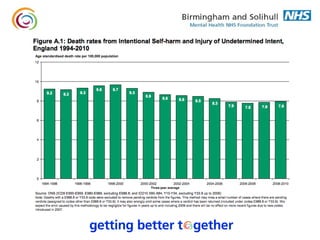
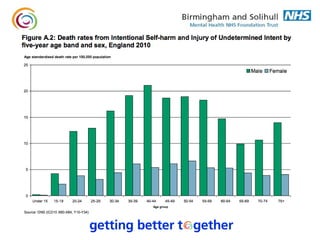
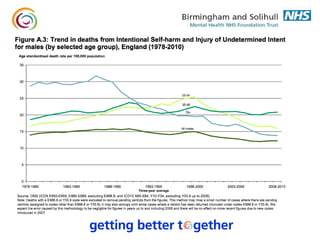
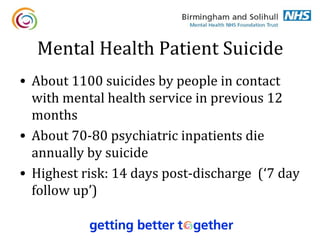
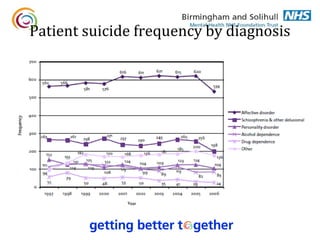
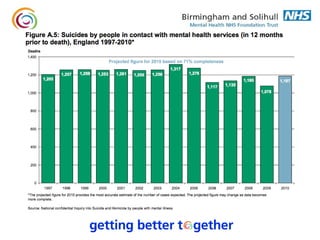
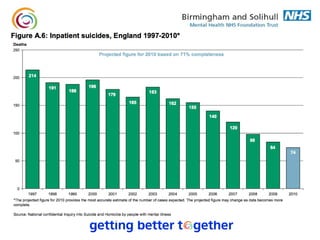
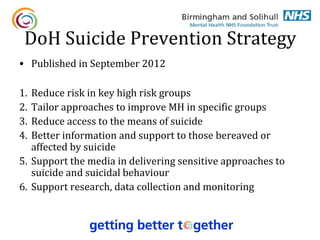
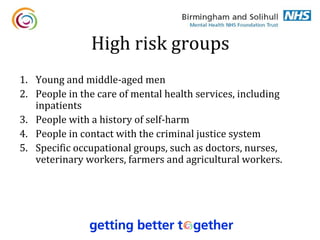
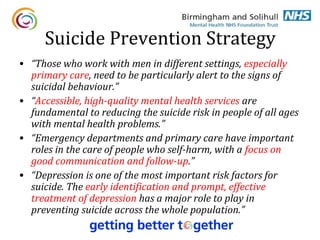
1. The document discusses suicide risk assessment and prevention. It provides an overview of statistical data on suicide rates in the UK, outlines high risk groups, and reviews the Department of Health's suicide prevention strategy.
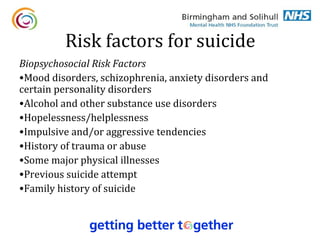
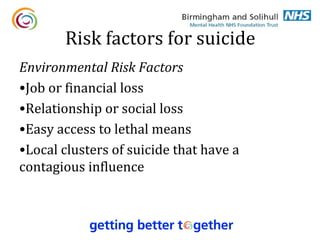
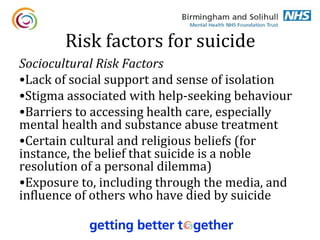
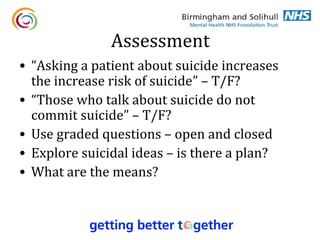
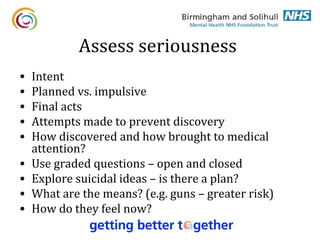
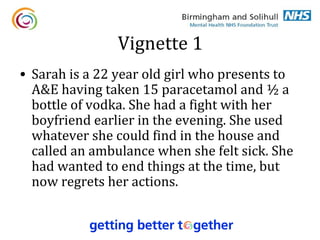
2. Risk factors for suicide include mood disorders, substance abuse, previous suicide attempts, and easy access to lethal means. A thorough risk assessment involves exploring suicidal thoughts and plans through open and closed questioning.
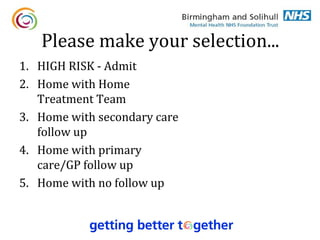
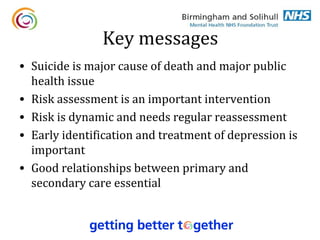
3. Ongoing support and follow-up are important for managing risk, as risk is dynamic and requires regular reassessment. Early identification and treatment of depression can help prevent suicide.




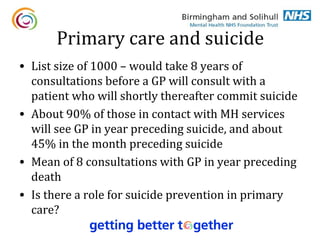
![Primary Care
• “GPs have a key role in the care of people who self-harm.
Good communication between secondary and primary care
is vital, as many people who present at emergency
departments following an episode of self-harm consult their
GP soon afterwards.”
• “Work undertaken by the London School of Economics has
shown that suicide prevention education for GPs can have an
impact as a population level intervention to prevent suicide.”
[ASIST course costs about £200 per GP]](https://image.slidesharecdn.com/suicide250213-130225155749-phpapp02/85/Suicide-Risk-Assessment-and-Prevention-22-320.jpg)