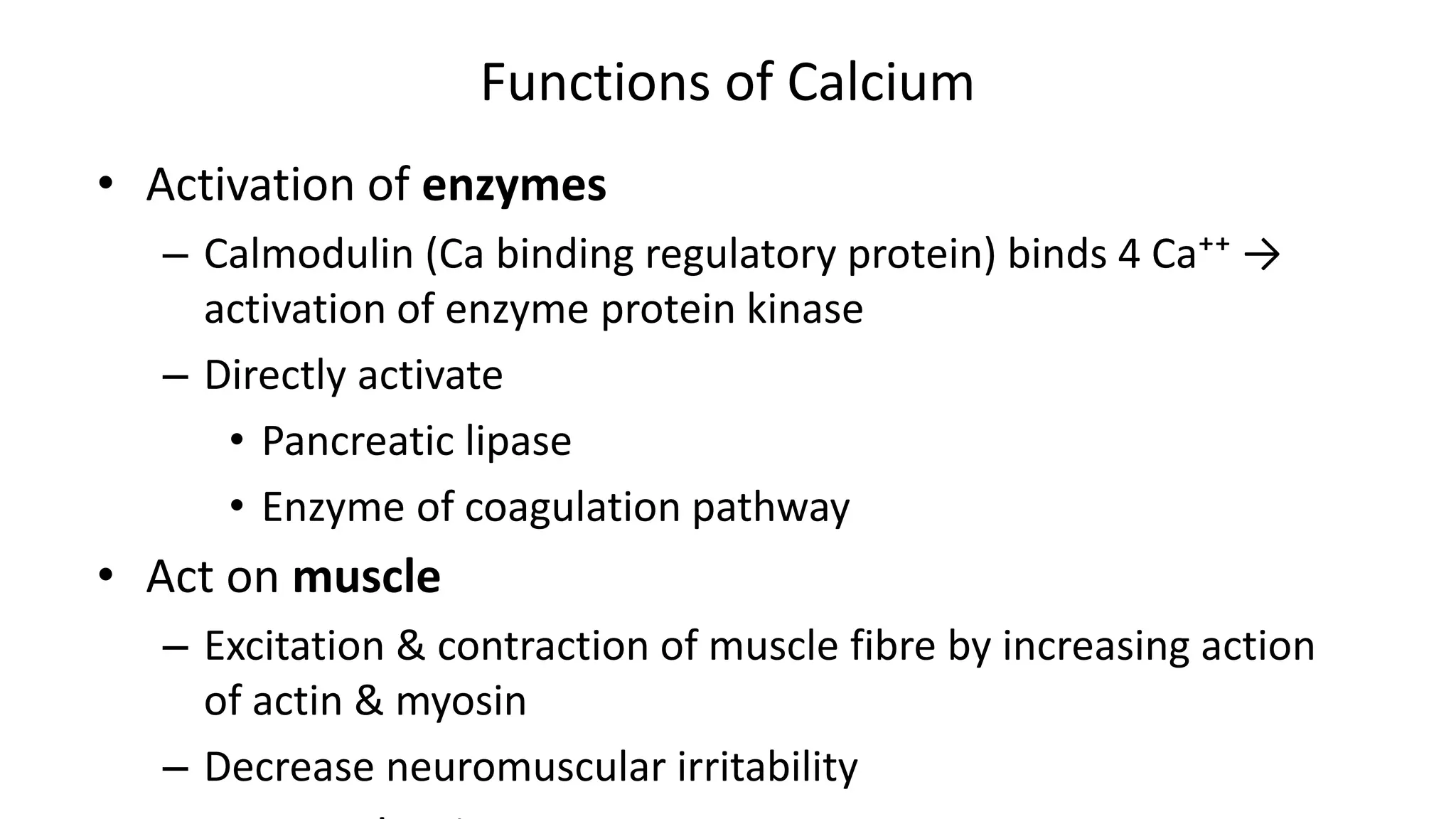
Minerals are inorganic elements required by the body in small amounts. They are classified as macrominerals, trace elements, and ultratrace elements based on daily requirements. Minerals serve important structural and functional roles. They are components of bones, teeth, cell membranes, and enzymes. Minerals help regulate processes like acid-base balance, fluid balance, nerve impulse transmission, and muscle contraction. Deficiencies can cause conditions like anemia, while excessive intake of some minerals can be toxic. Minerals are absorbed in the small intestine and their levels in the body are tightly controlled by hormones and homeostatic mechanisms.

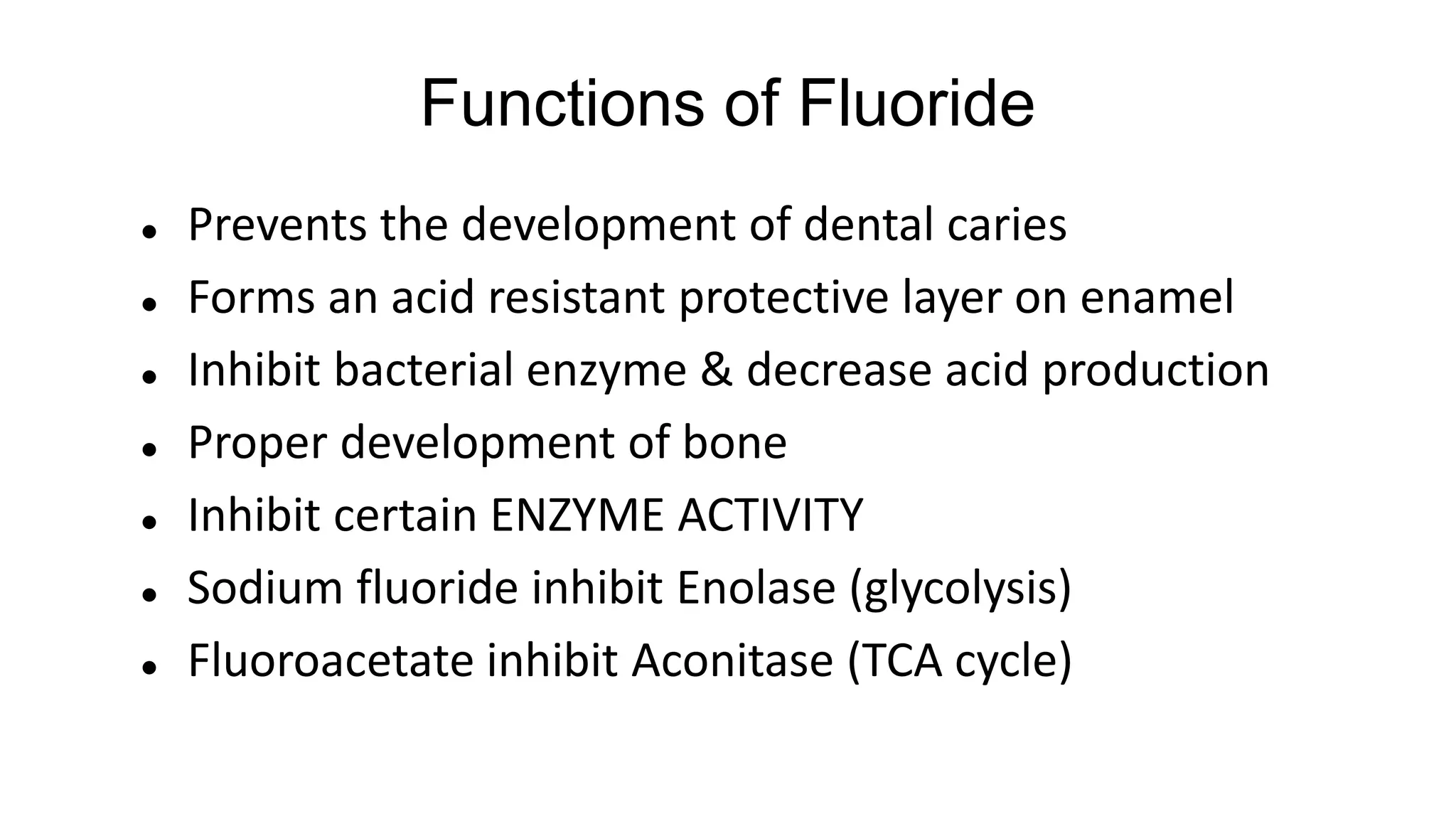
![Minerals
Minerals are inorganic elements required in small
amounts by the body (micronutrients).
• Widely distributed in food
• Requirement vary from g/day [Na, Ca], mg/day [Fe, Zn] or
µg/day [Iodine]
• Mixed diet provide sufficient amount
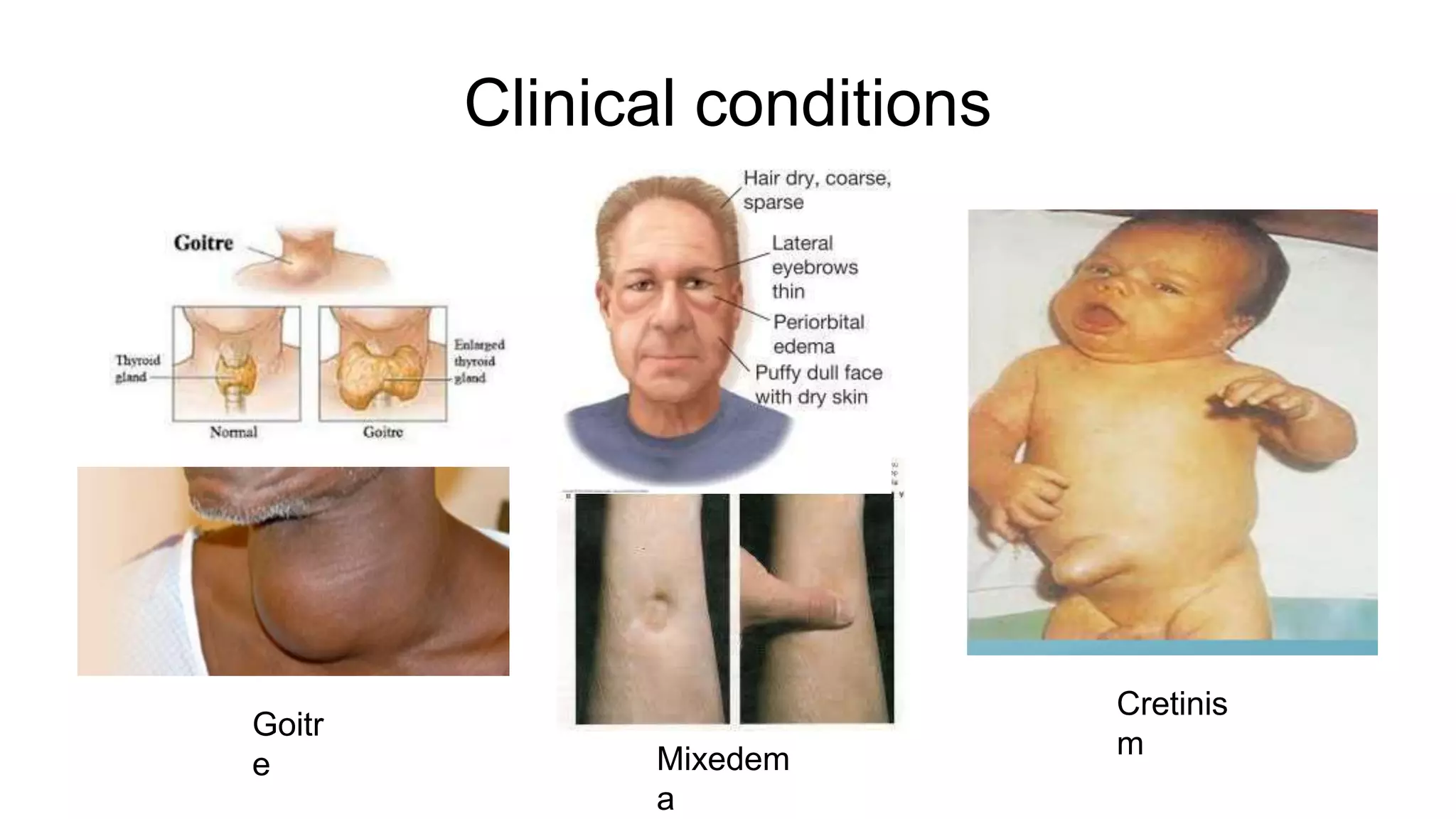
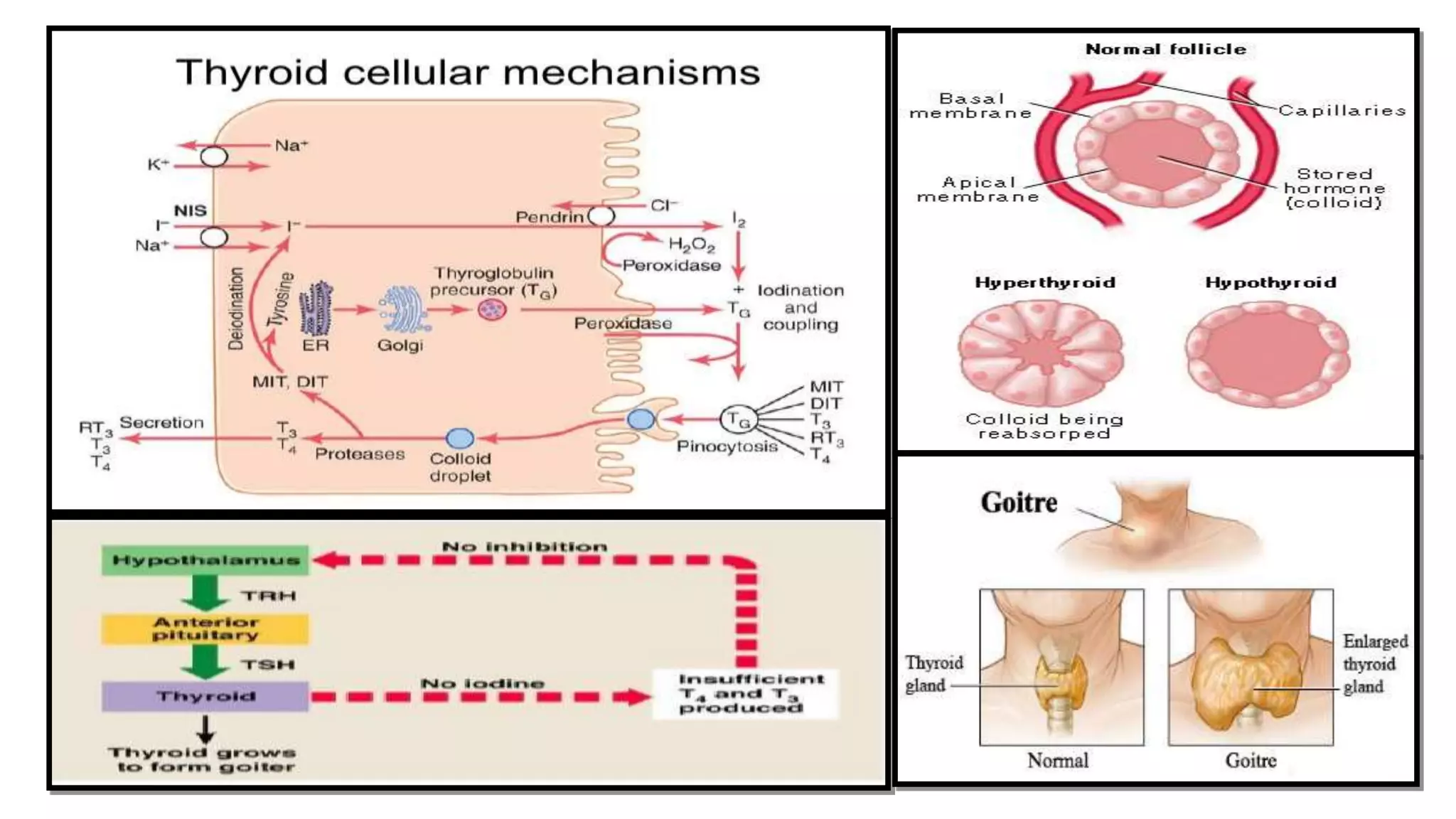
• Insufficient intake produce deficiency sign (anemia,
cretinism, goiter)
• Excessive intake may be toxic](https://image.slidesharecdn.com/minerals2-200719050115/75/Minerals-as-Nutrients-2-2048.jpg)
















![RBC life span: 120 days
Damaged erythrocytes are phagocytosed by macrophages of RES
Hb → Heme [+ globin]→ Fe+ Biliverdin
3-4 mg
20-25mg/d
5mg/d
2500mg
1000mg](https://image.slidesharecdn.com/minerals2-200719050115/75/Minerals-as-Nutrients-35-2048.jpg)



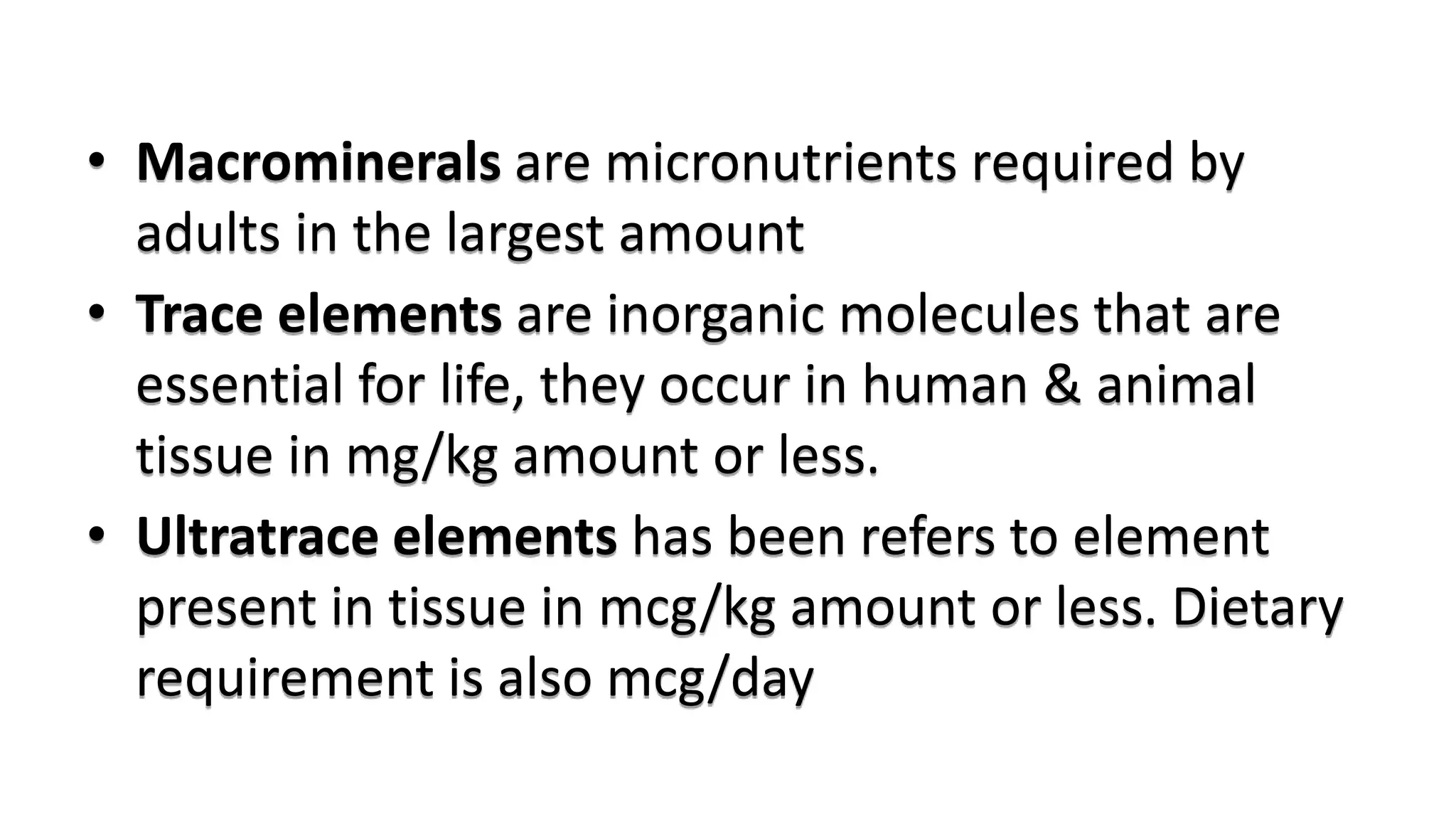
![Vitamin D & Ca Homeostasis
Condition GIT Bone Kidney
↓ [Ca] ↑ Ca
absorption
↑ mobilization Active vit D formation
↑ [Ca] ↓ Ca
absorption
[+] Calcitonin
[-] Ca mobilization
↑ excretion (calcitonin)
↓ reabsorption (PTH)
Inactive vit D formation
↓ vit D No absorption [+] Ca mobilization
(PTH)
↓ excretion (PTH)
↑ reabsorption (PTH)
↑ vit D ↑ absorption ↑↑ mobilization
↑ accumulation
↑ excretion (calcitonin)
Inactive vit D formation](https://image.slidesharecdn.com/minerals2-200719050115/75/Minerals-as-Nutrients-40-2048.jpg)