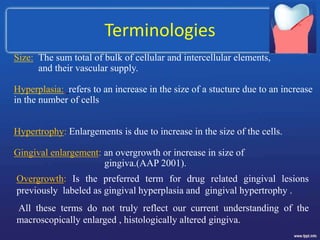
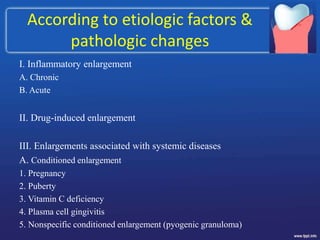
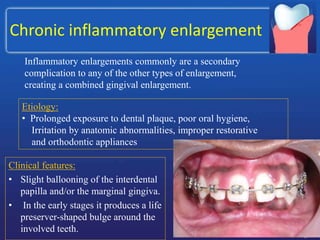
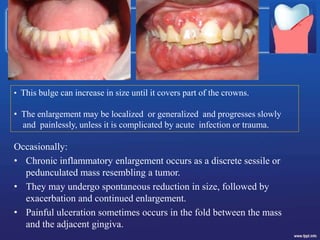
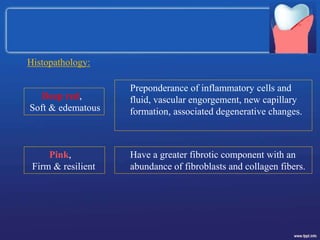
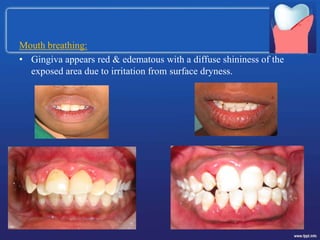
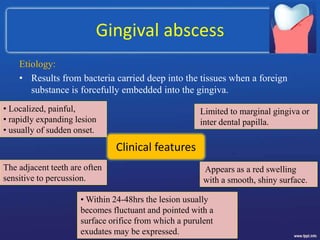
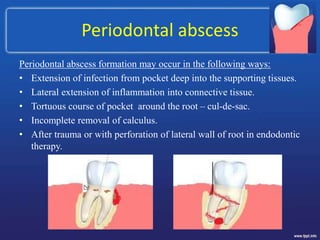
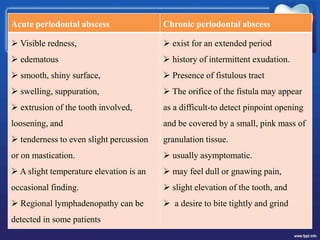
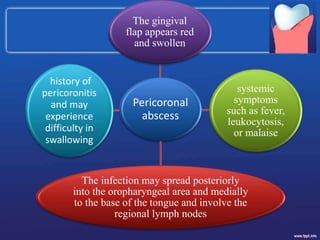
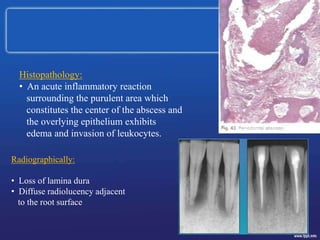
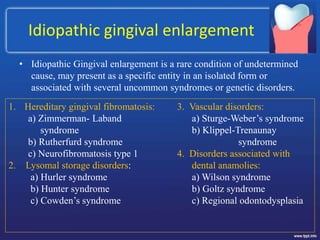
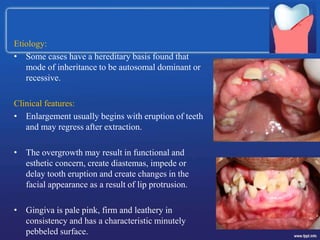
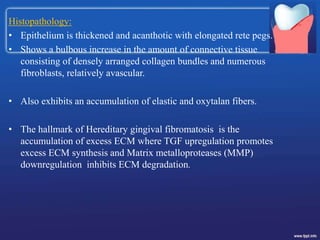
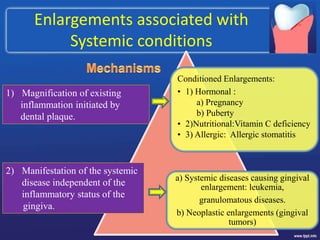
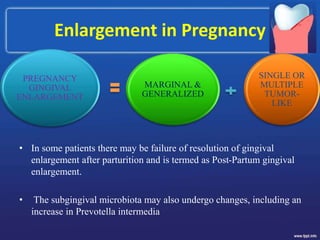
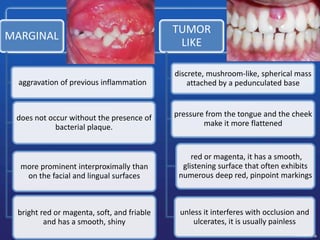
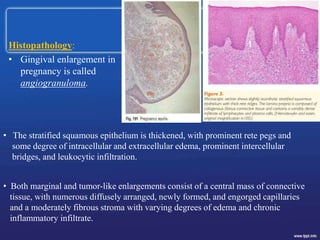
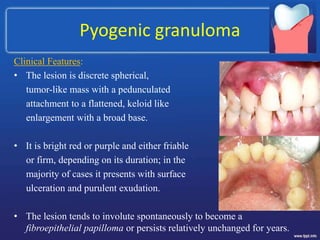
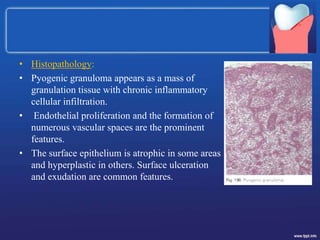
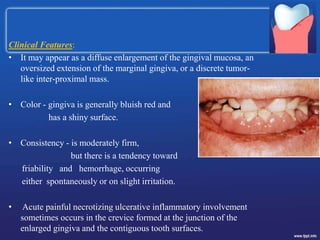
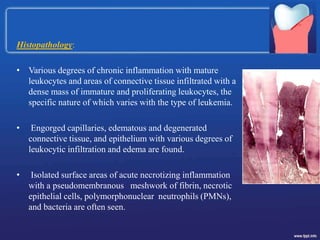
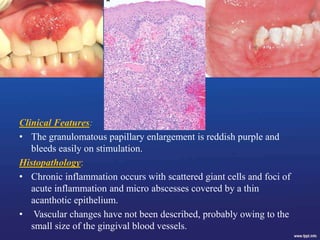
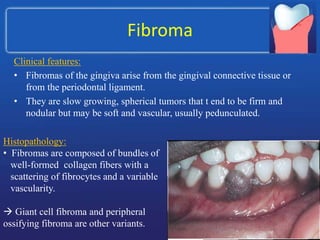
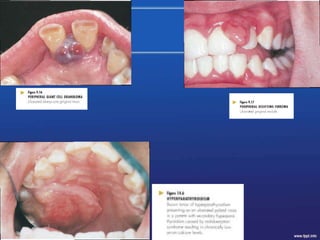
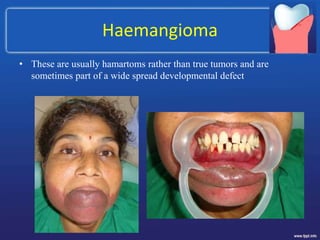
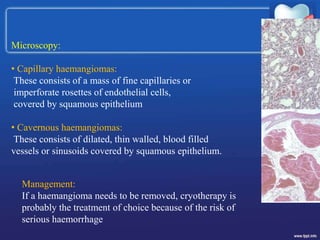
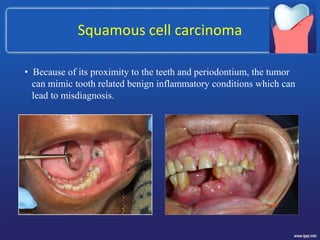
This document discusses gingival enlargement from multiple perspectives. It begins by defining key terms like hyperplasia and hypertrophy. It then categorizes enlargement based on location, etiology, degree, and associated conditions. Chronic inflammatory enlargement and acute conditions like gingival abscesses are explained. Drug-induced, hereditary, and condition-associated enlargements are explored. Systemic diseases that can cause enlargement like leukemia and Wegener's granulomatosis are summarized. The document concludes with an overview of neoplastic enlargements.