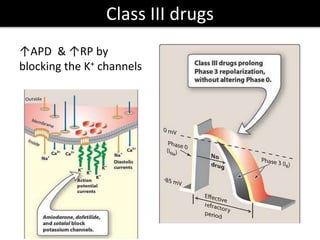
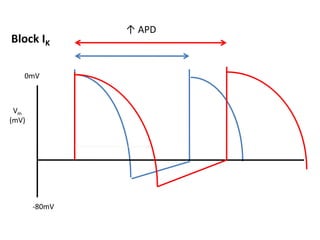
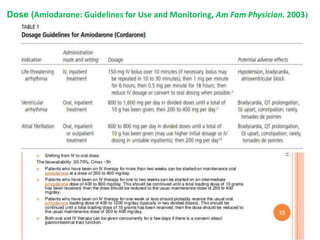
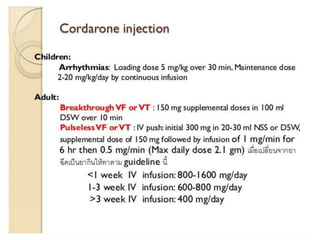
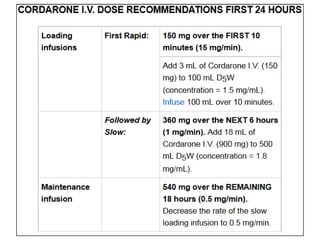
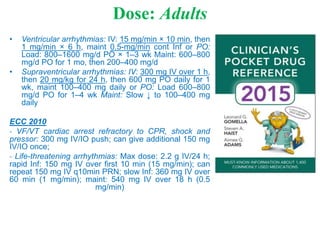
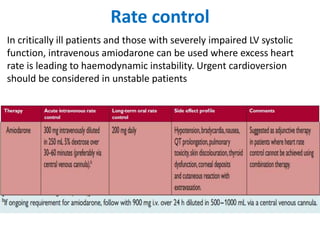
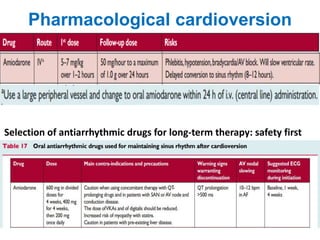
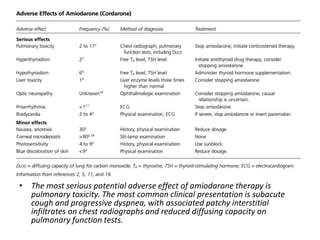
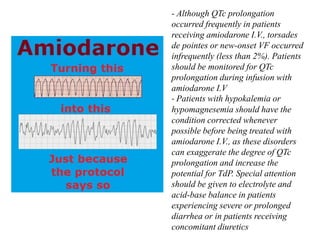
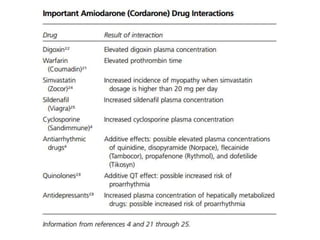
Amiodarone is a unique antiarrhythmic drug that is classified as class III but also possesses class I, II, and IV properties. It works by blocking sodium, calcium, and potassium channels to prolong the action potential duration. Amiodarone has a slow onset due to its high lipid solubility and storage in adipose tissues, resulting in a very long half-life. It can have serious side effects involving the lungs, thyroid, and interactions with other drugs. Amiodarone is effective for treating atrial fibrillation and ventricular arrhythmias when other options are not appropriate. Close monitoring is required due to risks of pulmonary toxicity and QT prolongation.