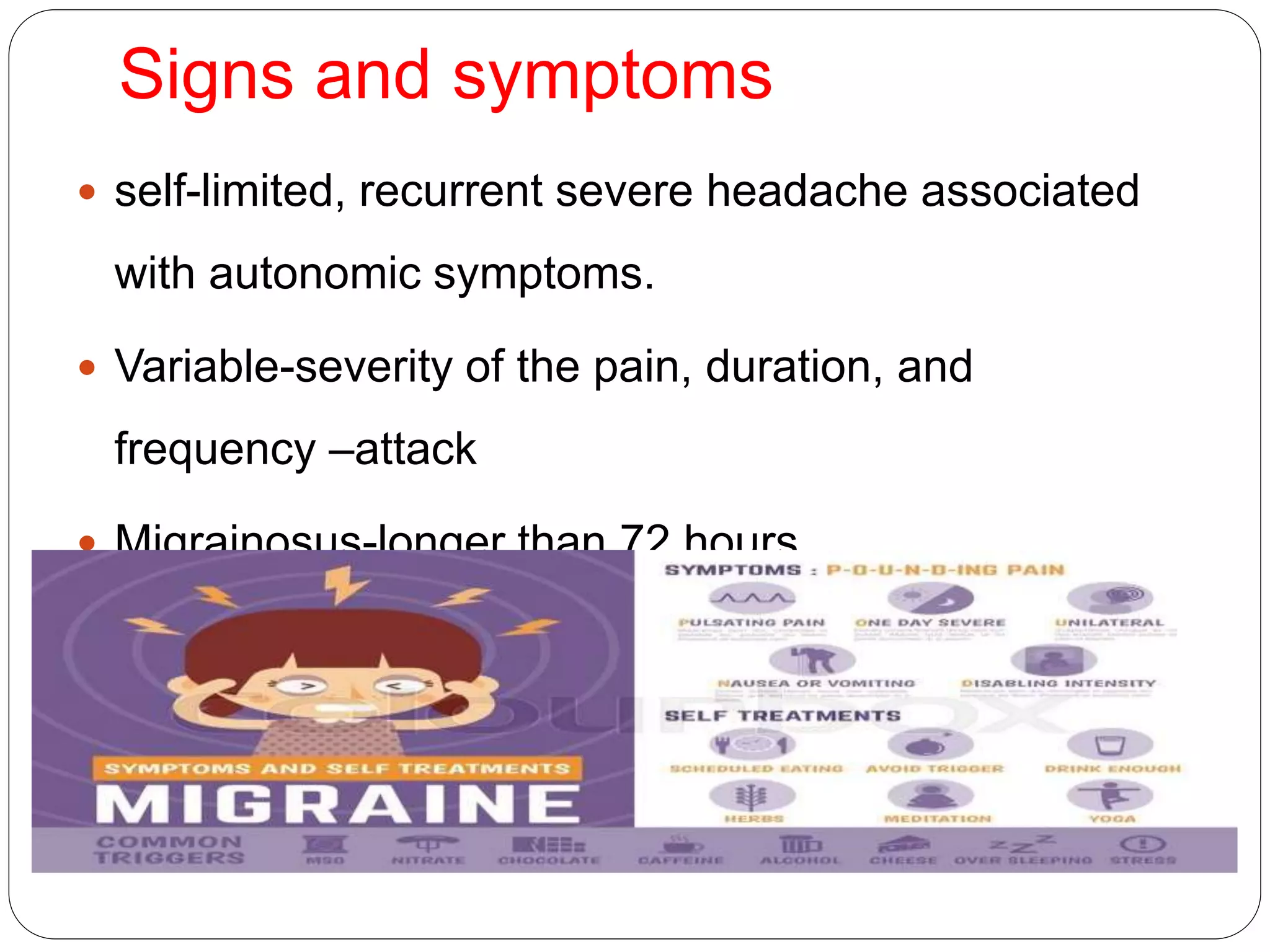
Migraine is a primary headache disorder characterized by recurrent headaches that can range from moderate to severe in intensity. It typically affects one half of the head and is pulsating in nature, lasting between 2 to 72 hours. Associated symptoms include nausea, vomiting, and sensitivity to light, sound or smell. Migraines are thought to be caused by a combination of genetic and environmental factors. They often run in families and can be triggered by changes in hormone levels, stress, hunger, or certain foods and drinks. Diagnosis is based on signs and symptoms according to established diagnostic criteria. Treatment involves lifestyle modifications, medications for prevention or acute attacks, and avoiding triggers.
























![symptoms
Pakshat kupyati maasat vaa swayameva cha
shamyati
ati vridhastu nayanam sravanam vaa vinashayet [A
H. u 23]
Yasya uthamaga ardhamateeva jantho: sambhedha
toda bhrama shoolajushtam,
pakshadhashaahad adhava api aakasmaat tasya
ardhavabhedakam tritasyat vyavasthade. [S S. u
25/15]](https://image.slidesharecdn.com/migraine-170226034243/75/Migraine-28-2048.jpg)








