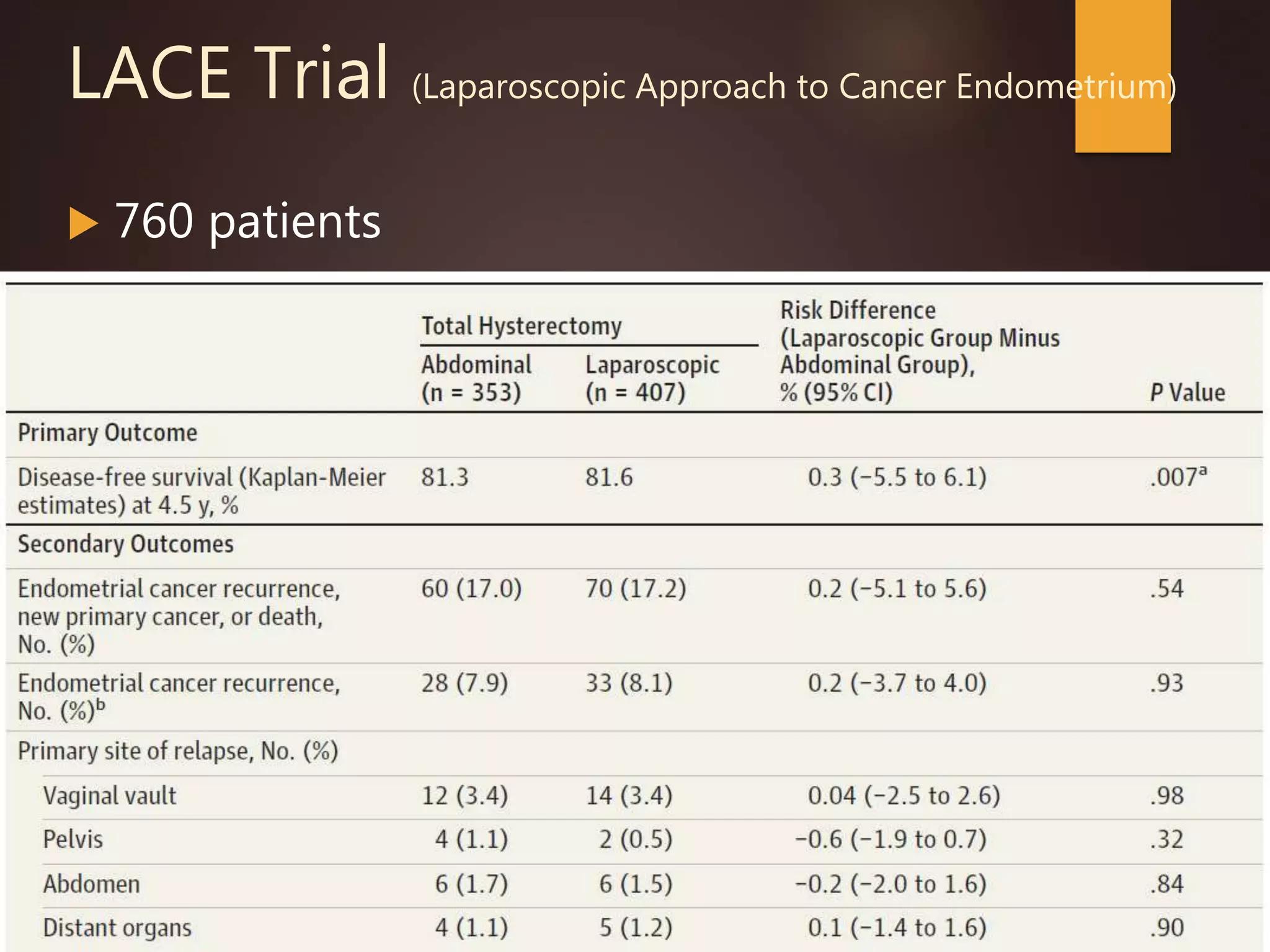
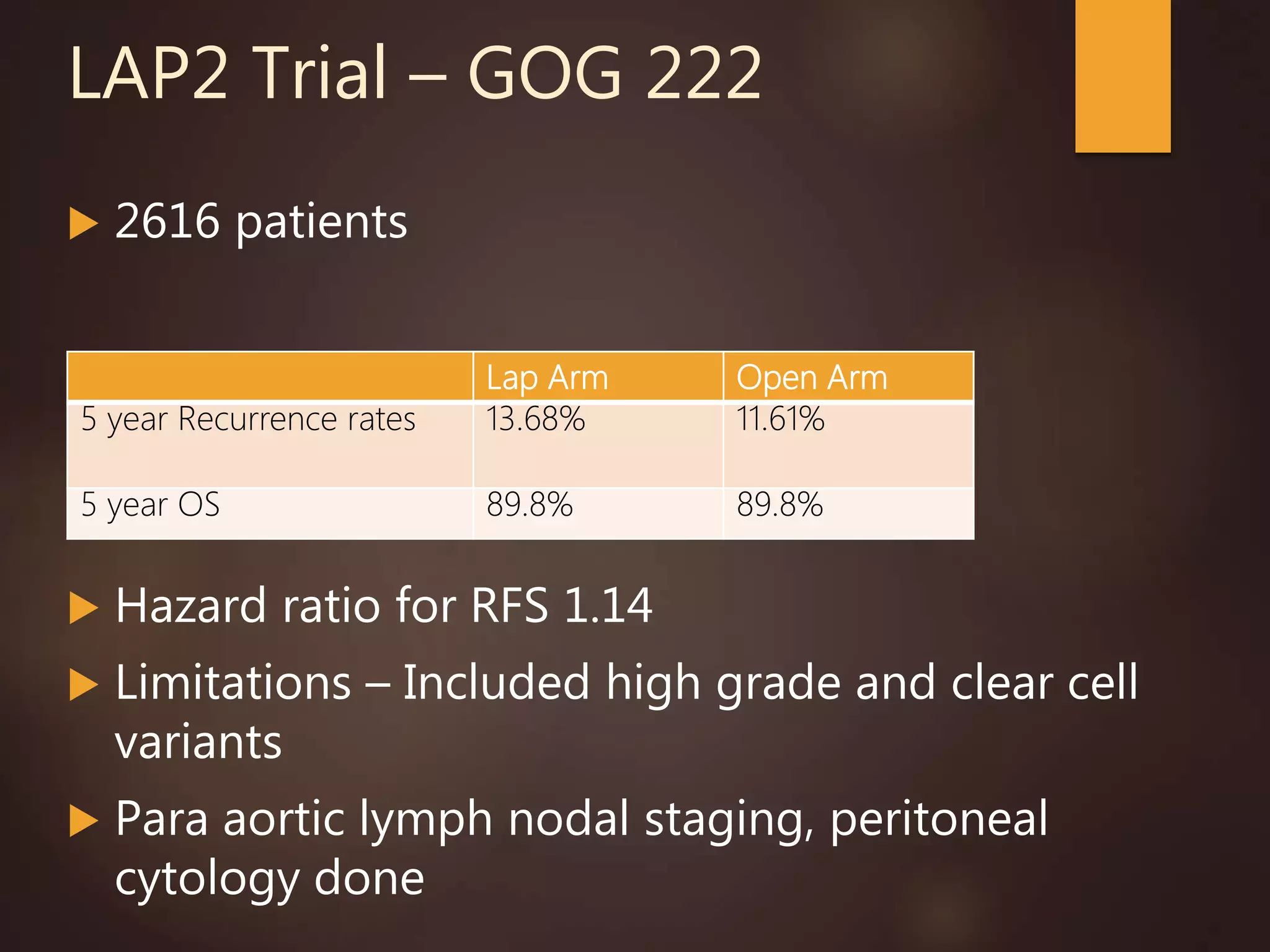
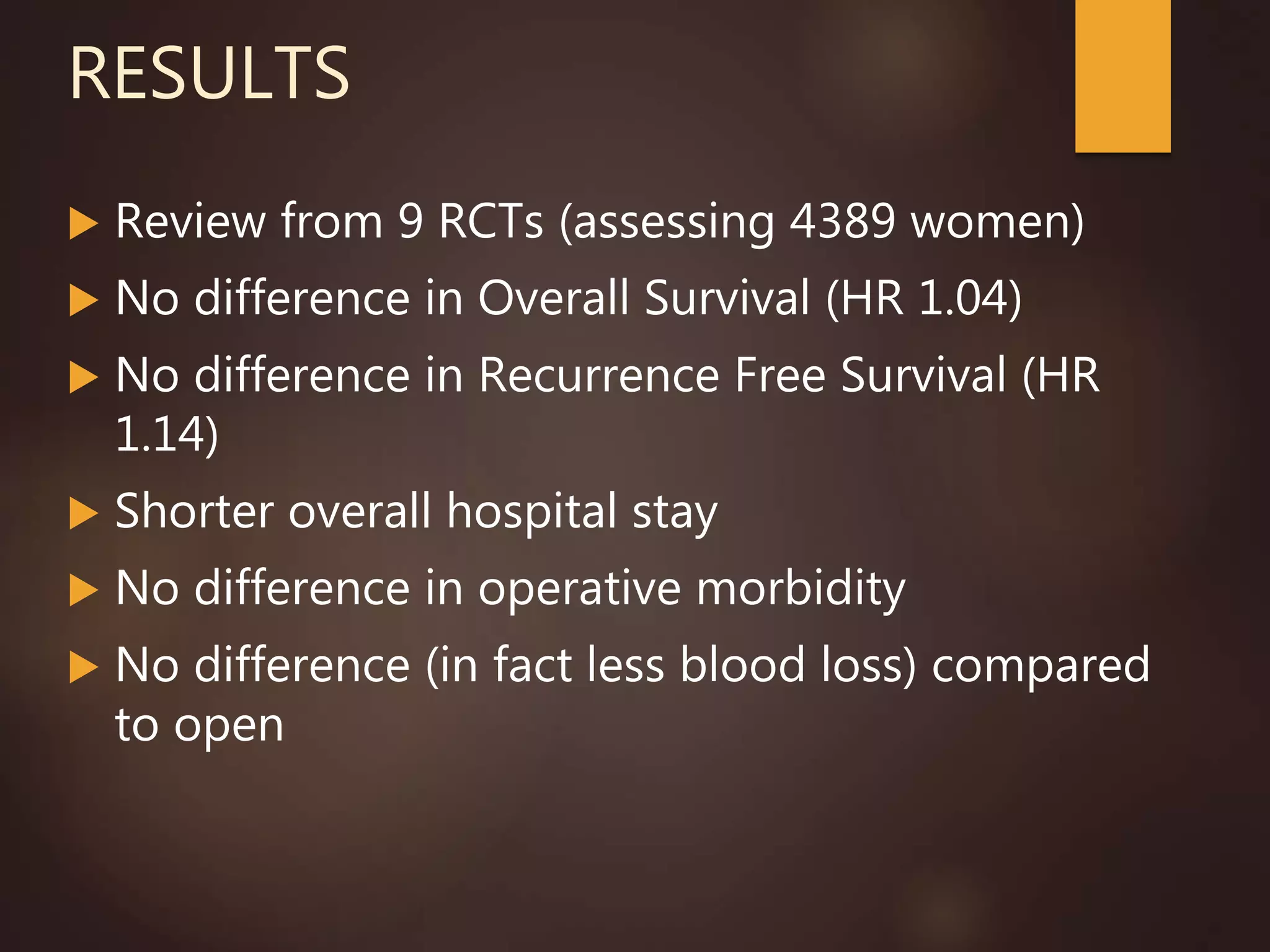
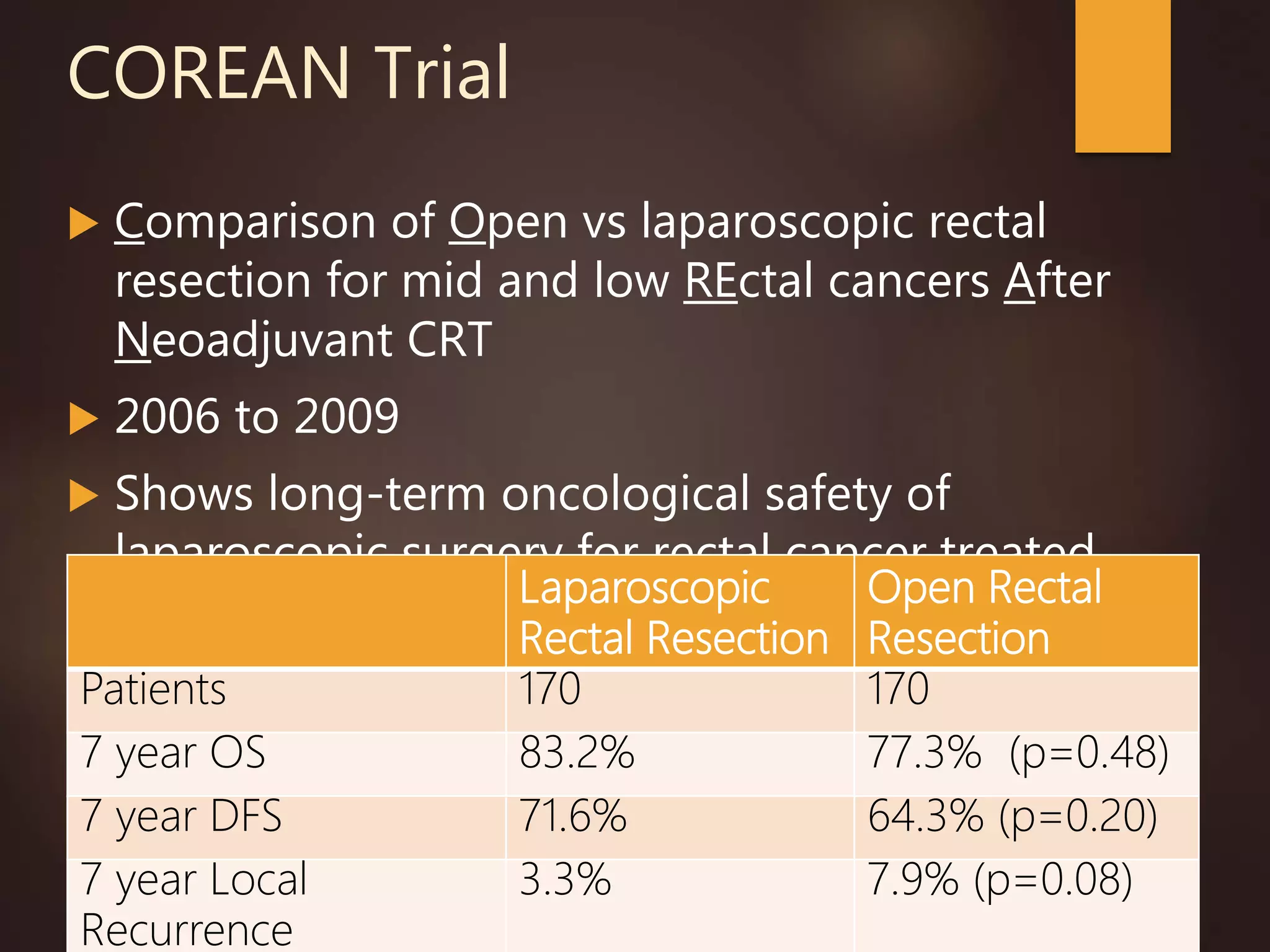
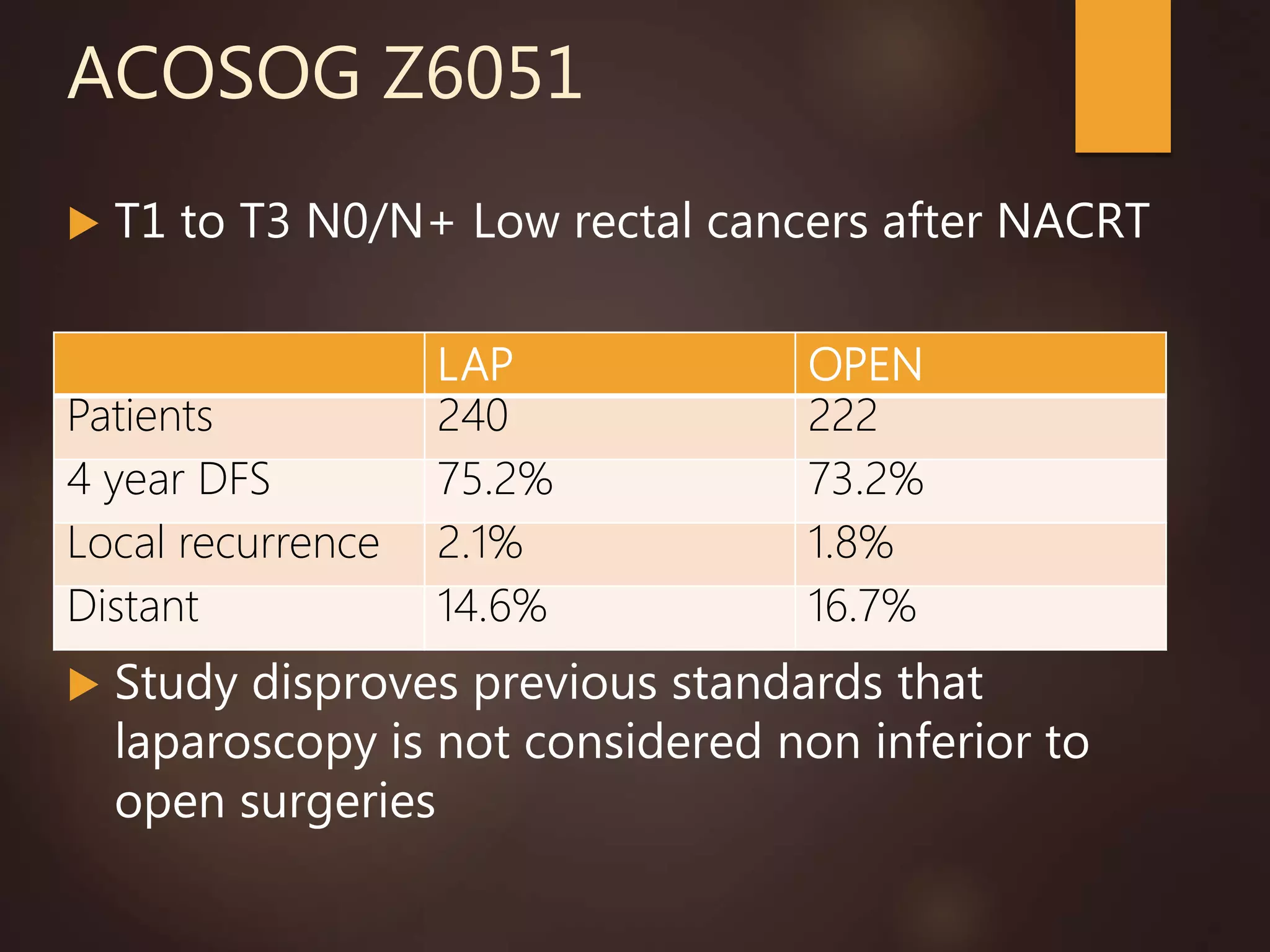
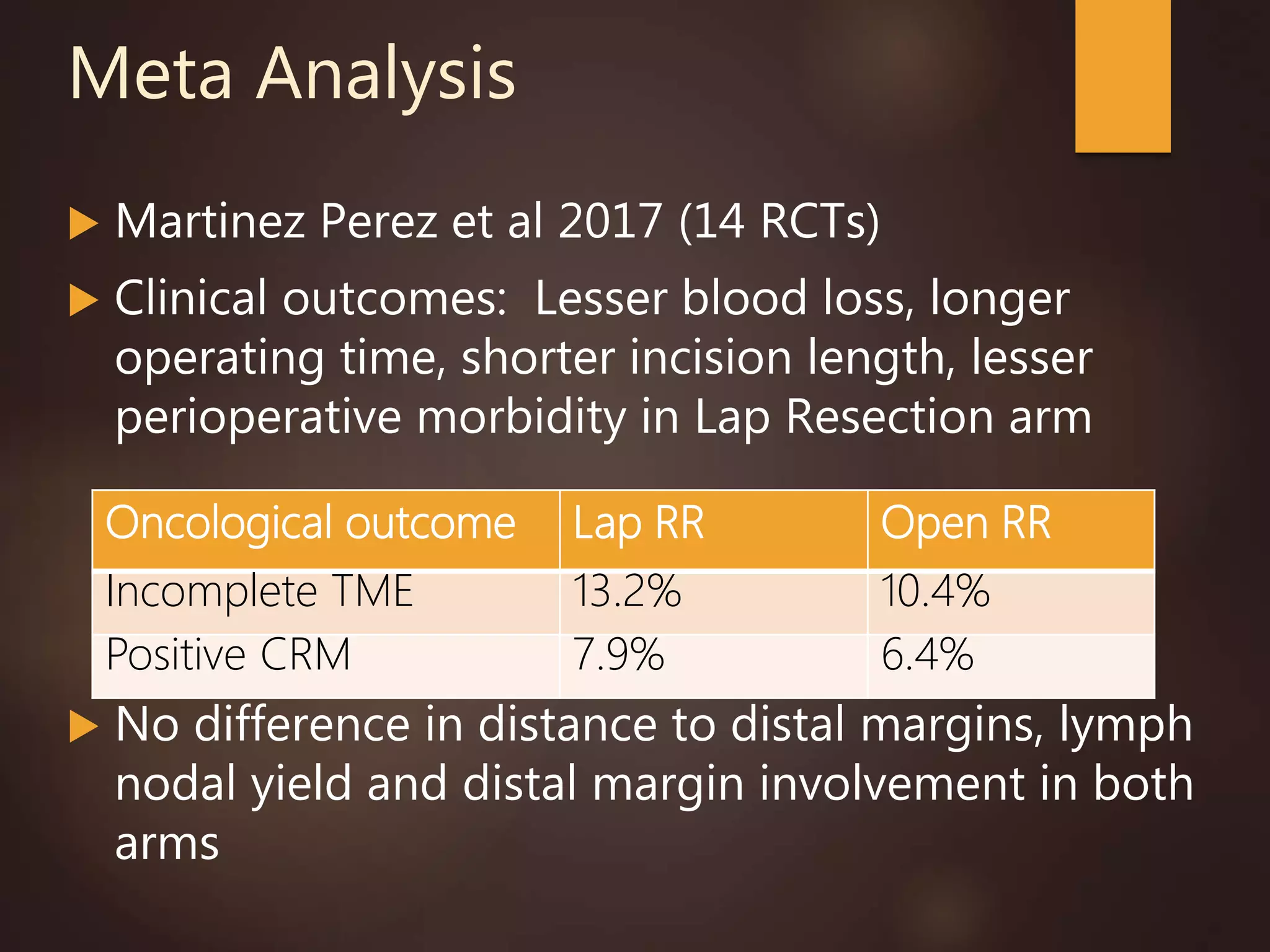
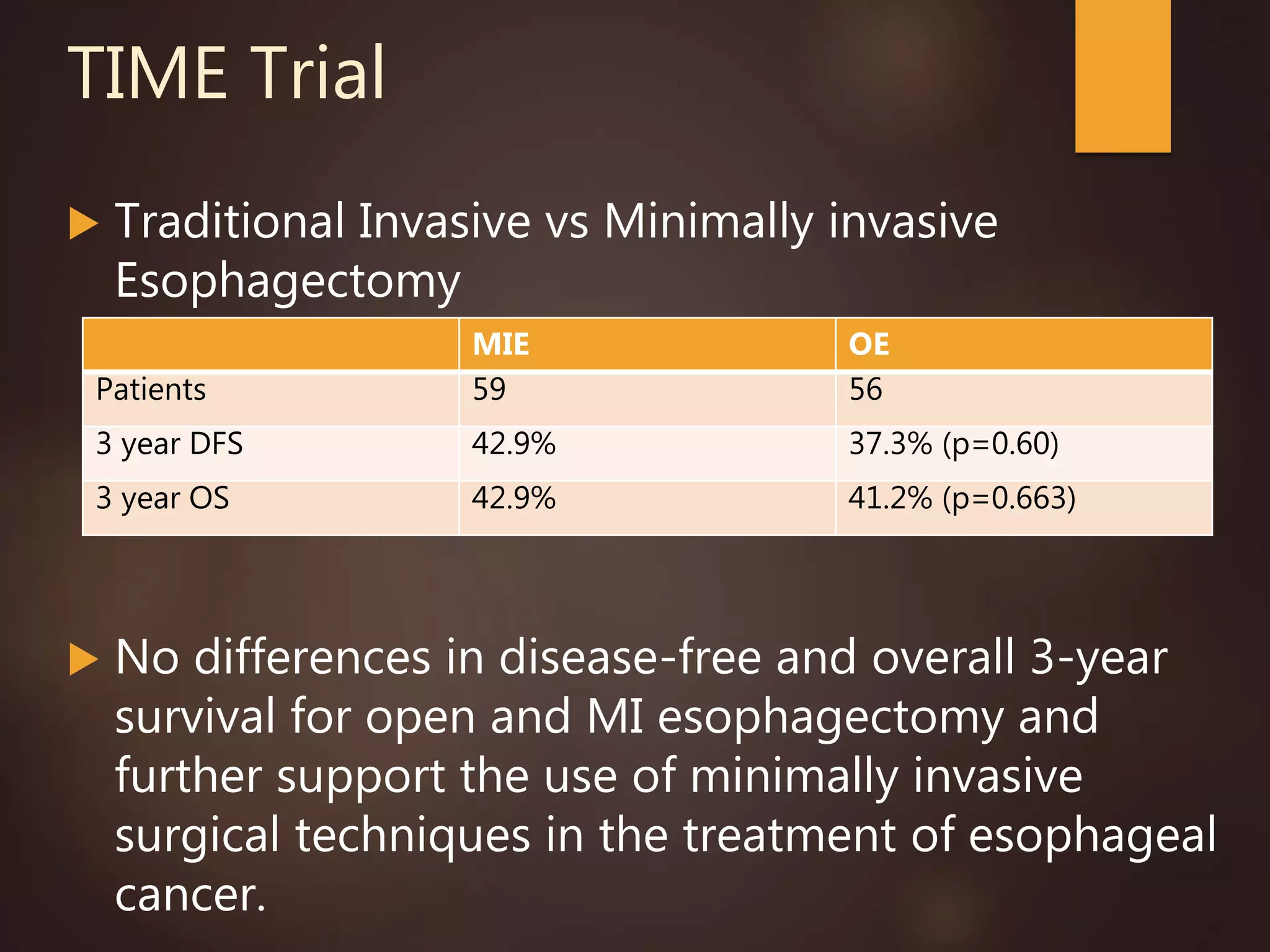
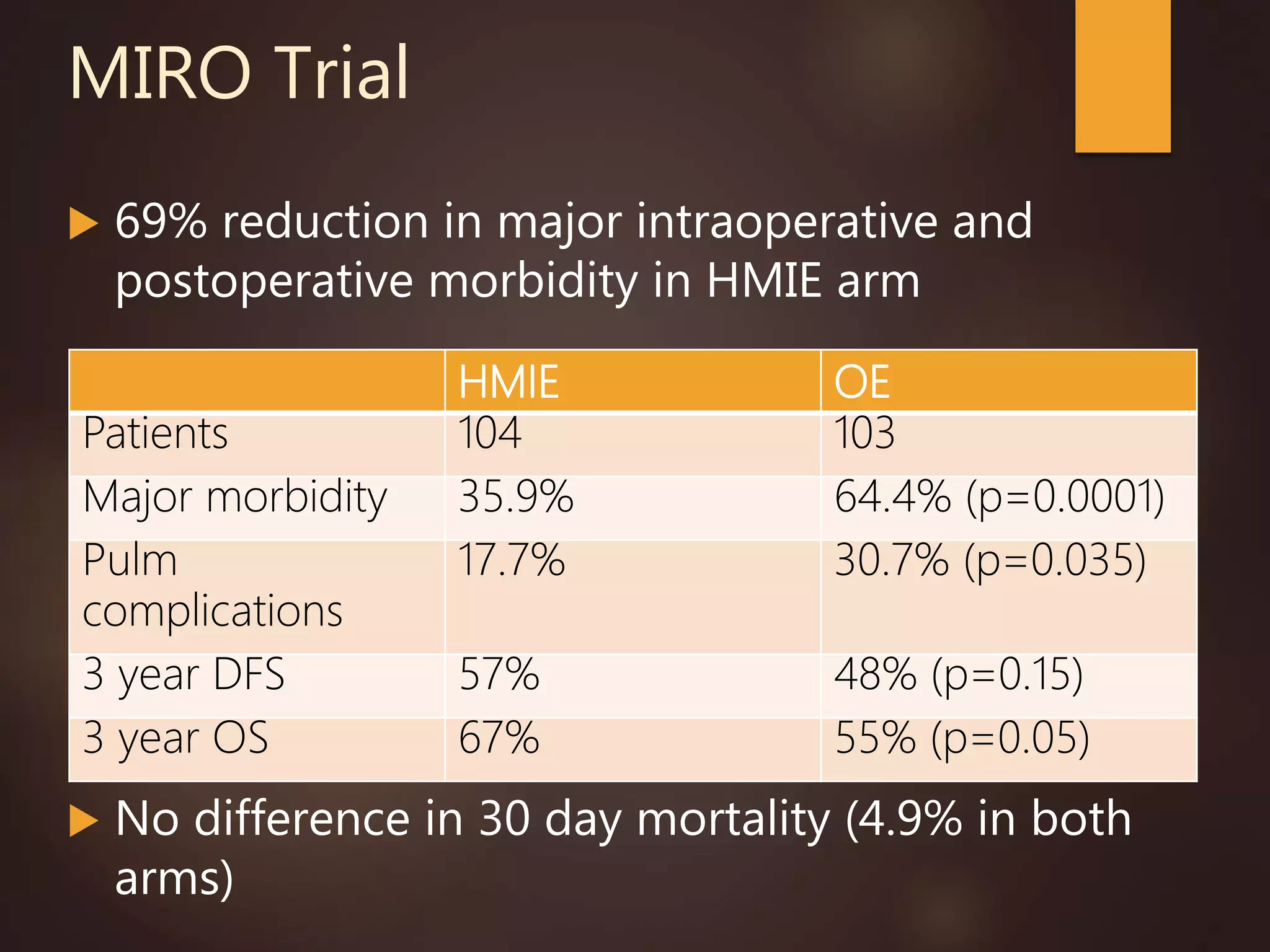
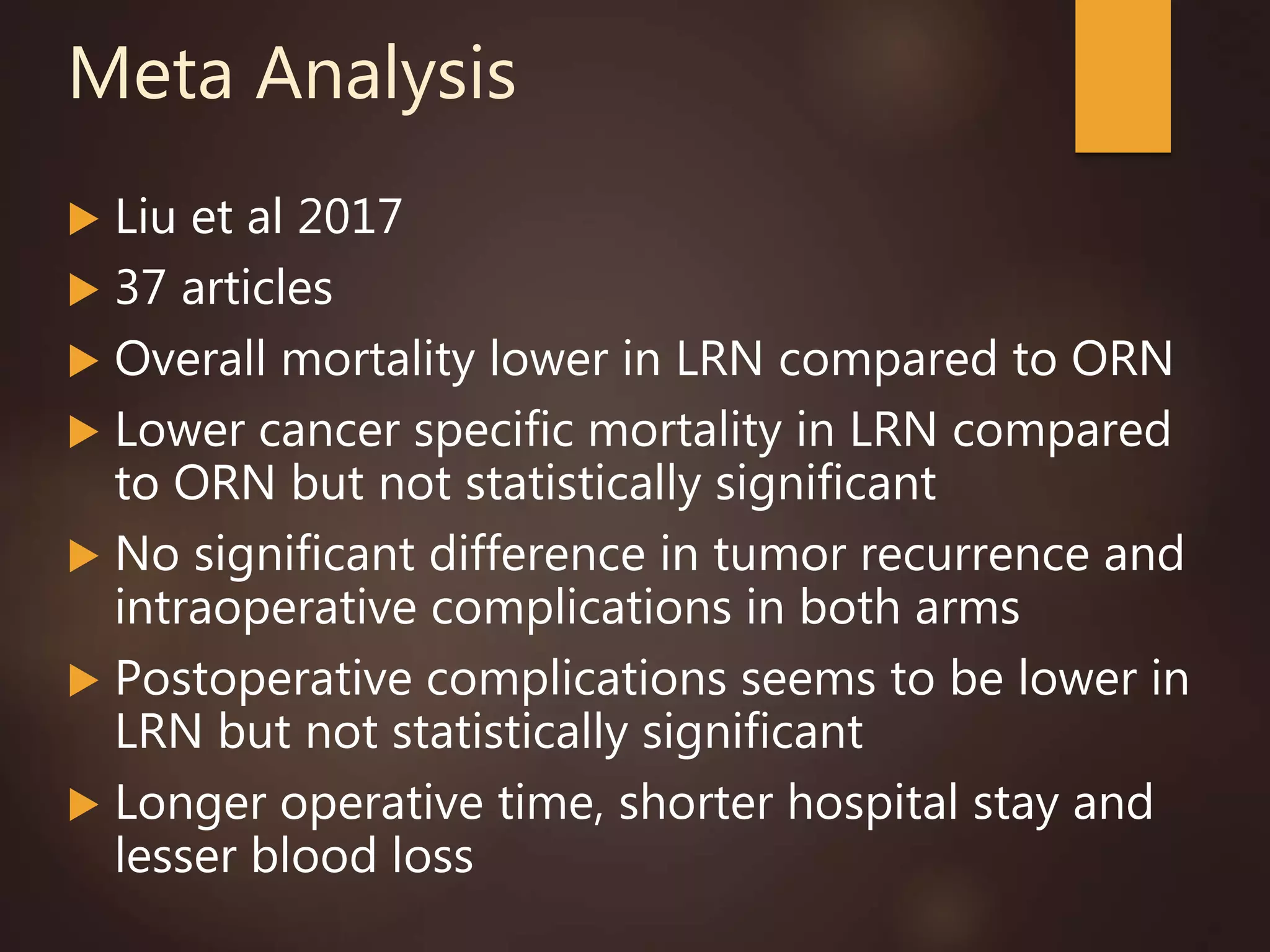
The document presents an overview of minimally invasive surgery techniques in oncology, highlighting significant trials and outcomes related to laparoscopic procedures for various cancers. Key findings indicate no substantial differences in overall survival and recurrence rates between laparoscopic and open surgeries, although laparoscopic methods generally offer advantages like reduced blood loss and shorter hospital stays. The data reinforces the ongoing support for minimally invasive approaches across different types of cancer treatments.