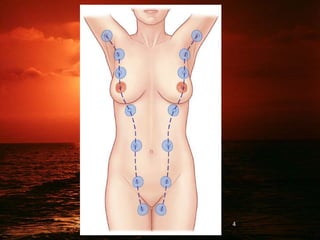
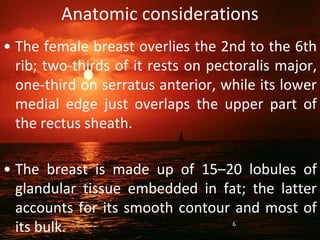
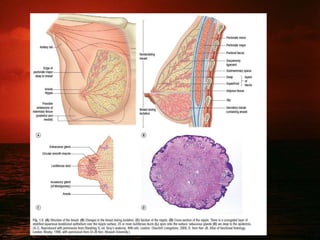
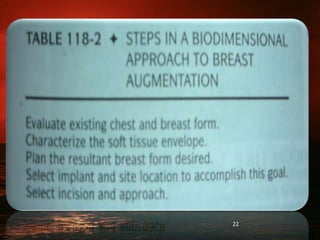
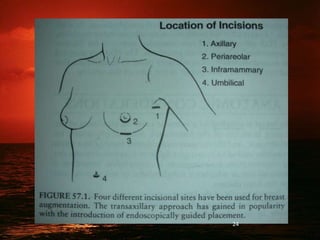
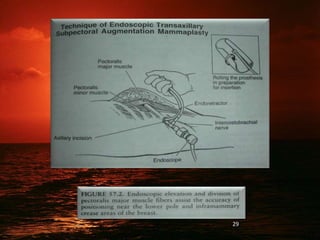
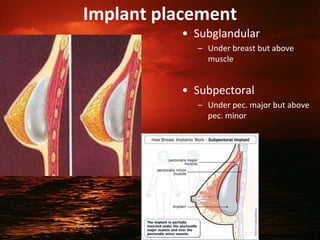
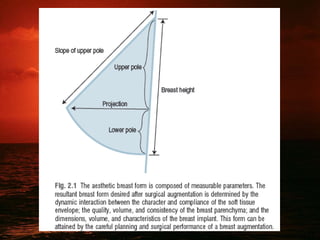
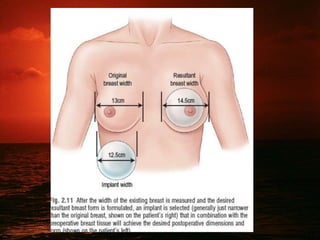
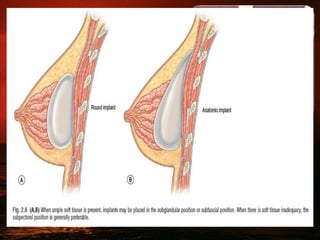
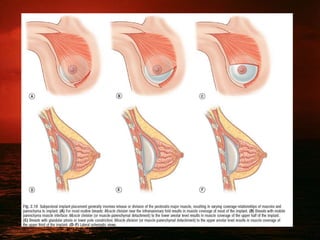
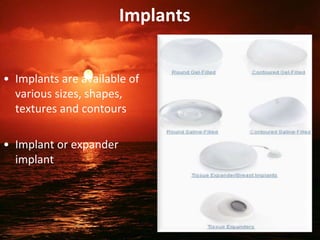
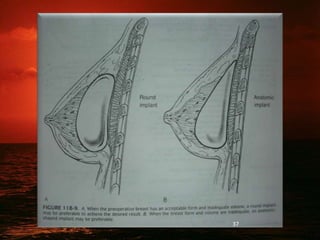
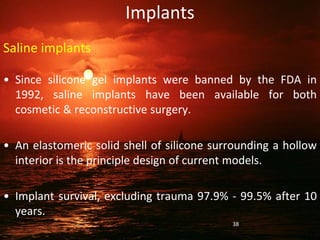
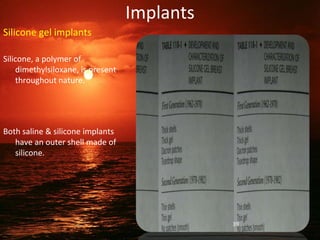
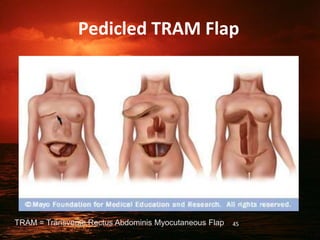
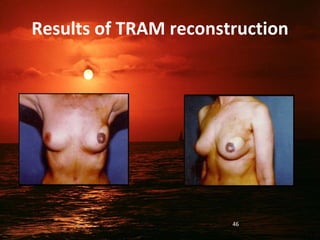
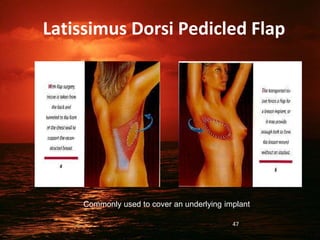
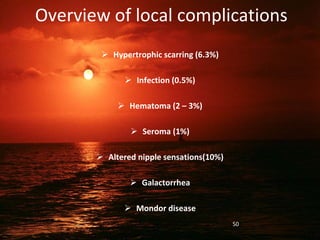
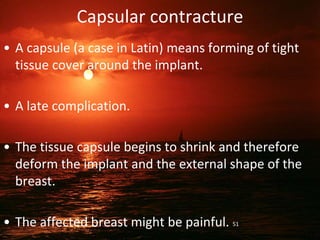
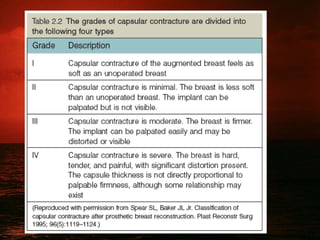
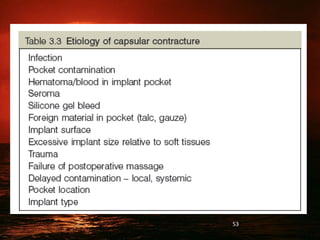
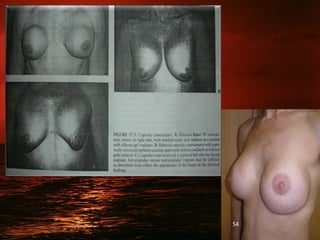
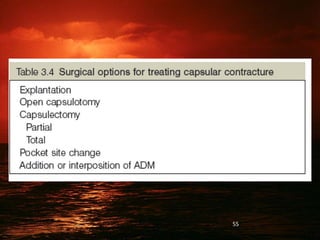
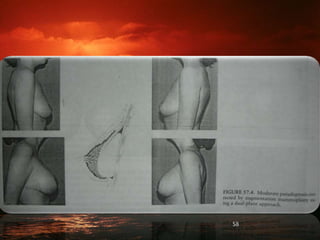
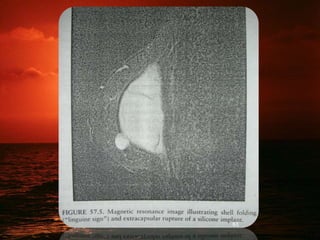
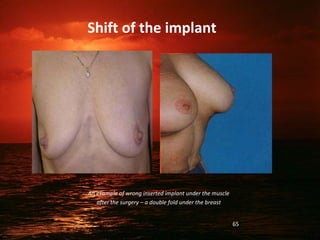
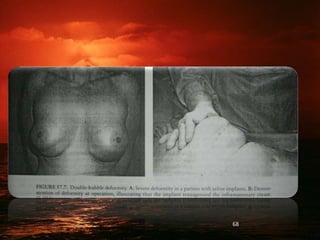
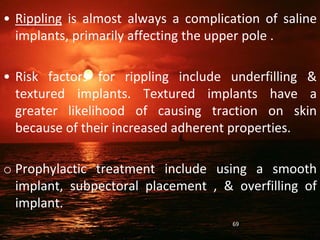
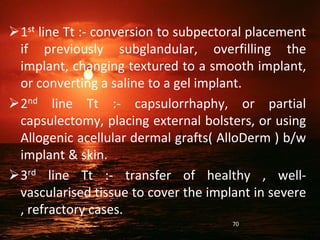
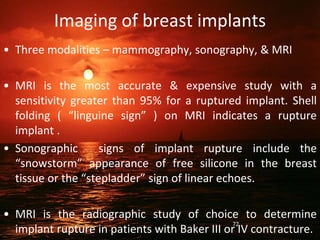
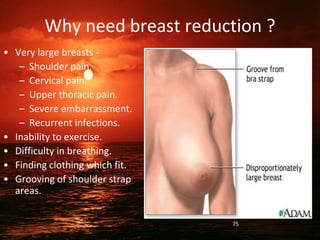
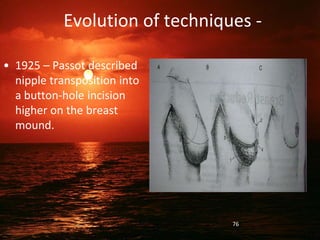
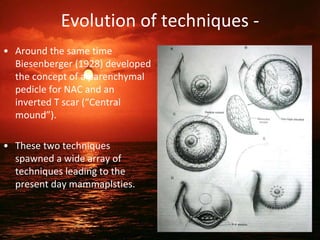
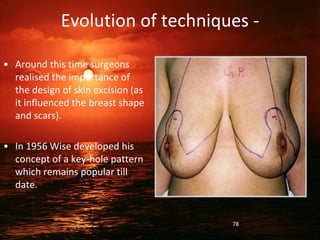
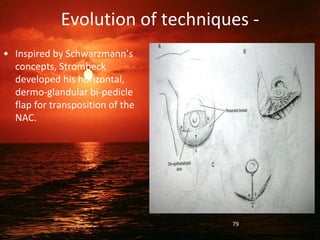
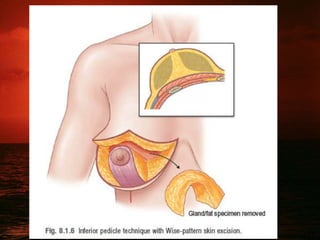
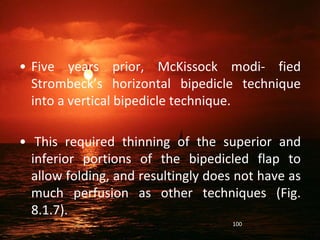
This document discusses breast augmentation (mammoplasty) surgery. It covers breast anatomy, the surgical techniques for augmentation including different incision sites and implant placement locations. It describes the types of implants available including saline and silicone gel implants. The document discusses complications like capsular contracture and their treatment. It also addresses psychological, imaging and long term safety issues regarding breast implants.