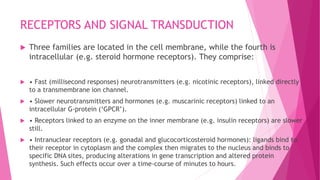
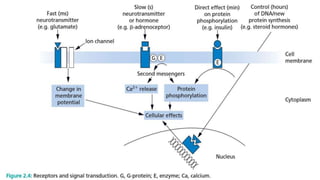
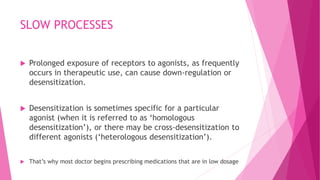
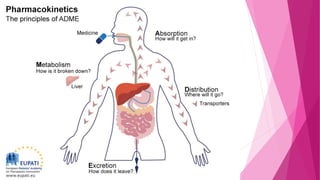
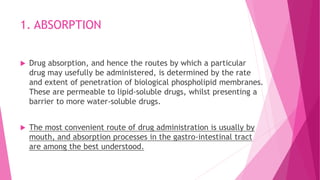
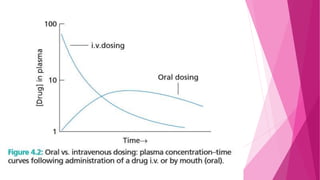
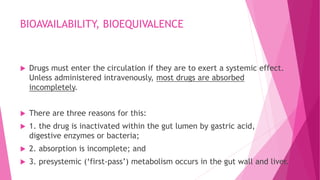
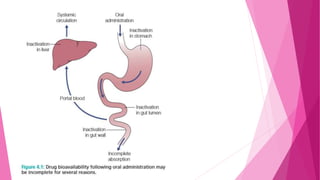
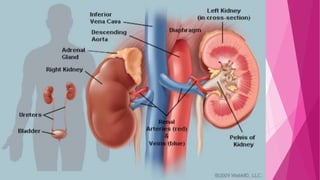
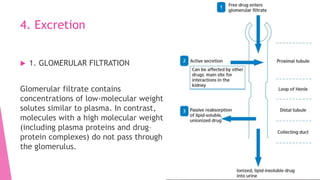
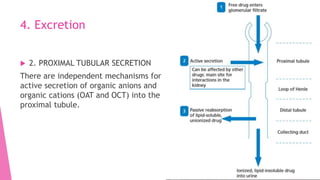
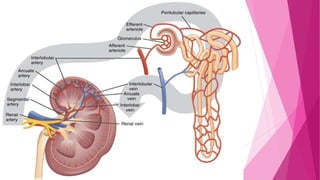
This document discusses pharmacodynamics and pharmacokinetics. Pharmacodynamics is the mechanism of drug action and the relationship between drug concentration and the body's response. Most drugs act by binding to receptors on cells. Pharmacokinetics involves the absorption, distribution, metabolism and excretion of drugs in the body. Drugs can be administered through various routes including oral, intravenous, intramuscular and others. Factors like age, liver and kidney function impact how drugs are processed in the body.
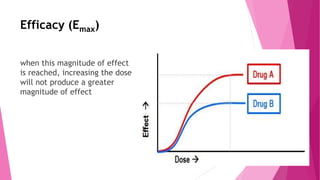
![Potency
"[Potency is] an expression of the activity of a drug, in
terms of the concentration or amount needed to produce
a defined effect."](https://image.slidesharecdn.com/2-190310064152/85/2-pharmacodynamics-and-kinetics-10-320.jpg)












![References:
• Audrey Berman . . . [et al.]. – 9th
ed. (2012) KOZIER & ERB’S
Fundamentals of NURSING
Concepts, Process, and Practice.
• James M Ritter, L.Lewis, T. Mant
and A.Ferro. 5th ed. (2008) A
Textbook of Clinical
Pharmacology and Therapeutics](https://image.slidesharecdn.com/2-190310064152/85/2-pharmacodynamics-and-kinetics-74-320.jpg)