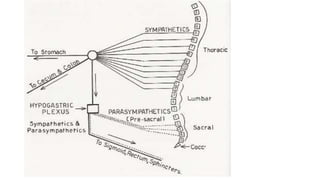
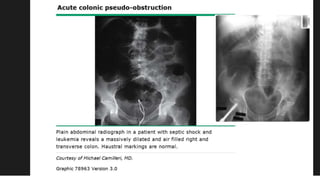
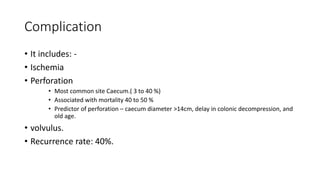
Ogilvie's syndrome, also known as acute colonic pseudo-obstruction, is characterized by dilation of the cecum and right colon without mechanical obstruction. It was first described in 1948 and is caused by an imbalance in the autonomic nervous system regulating colonic motility. Symptoms include abdominal distension and pain. Diagnosis involves abdominal x-rays showing colon dilation. Treatment aims to decompress the colon initially with nasogastric tubes, enemas, or neostigmine injections, with surgery considered if decompression fails or complications like perforation occur. Risks include ischemia, perforation and high mortality with perforation.