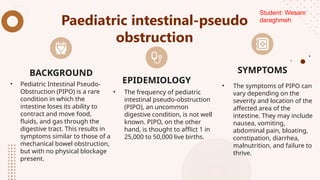
thi ppt disscuss points about Acute, chronic and paediatric intestinal-pseudo obstructions are rare disorders that occur when nerve or muscle problems slow or stop the movement of food, fluid, air, and waste.
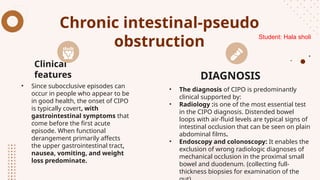
Symptoms of intestinal pseudo-obstruction include abdominal pain, bloating, and nausea and vomiting.
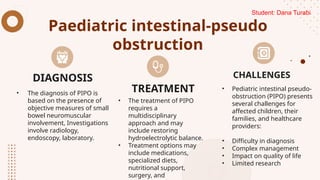
Diagnosis is based on clinical observation and radiography.
Treatment involves medications, specialized diets, nutritional support, surgery, and physical therapy.
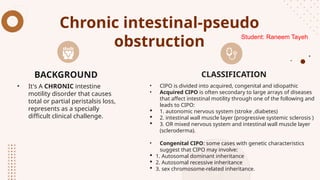
The pathophysiology of Chronic intestinal pseudo-obstruction is multifactorial and assigned to several theories, Theory of autonomic denervation, the Hormonal Theory and the Pharmacologic Theory