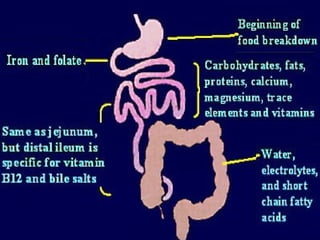
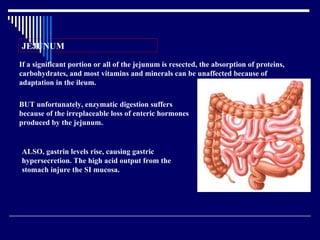
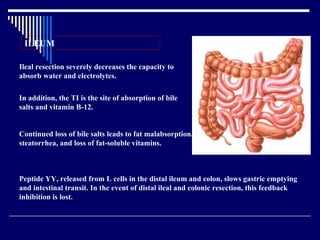
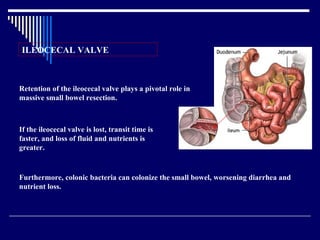
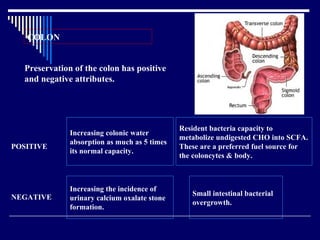
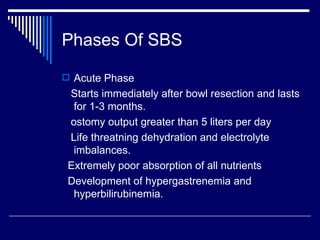
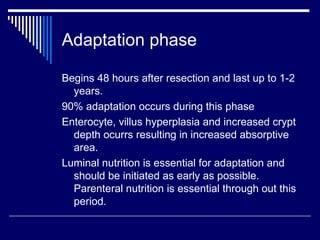
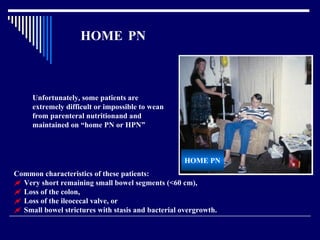
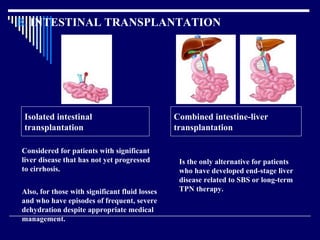
Short bowel syndrome is defined as having less than 200cm of residual small bowel. It results in malabsorption, diarrhea, and nutritional deficiencies due to the loss of absorptive capacity. Management involves fluid/electrolyte replacement, nutritional support including parenteral nutrition, and medications. While some patients can be weaned off parenteral nutrition, others require long-term home parenteral nutrition support. Surgeries like bowel lengthening procedures and serial transverse enteroplasty aim to improve absorption, but transplantation is the only alternative for those with end-stage complications.