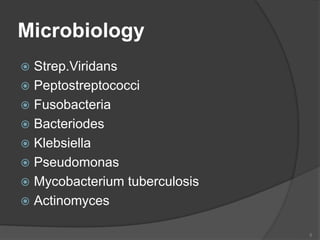
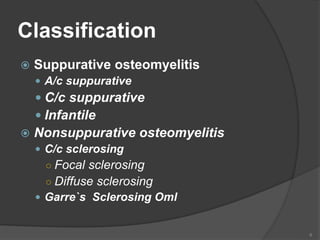
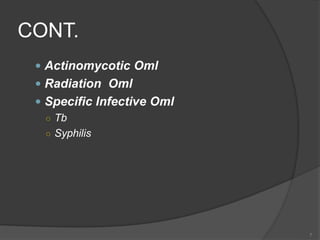
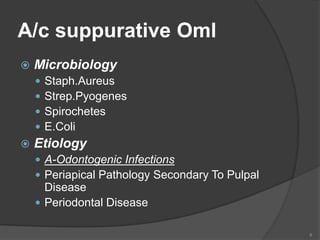
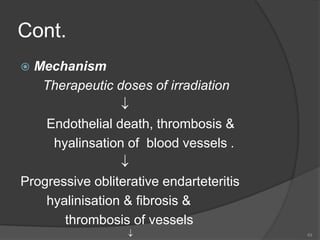
This document discusses osteomyelitis of the jaw, including its definition, etiology, classification, clinical features, microbiology, and management. It defines osteomyelitis as an inflammatory bone infection that begins in the medullary spaces and spreads to involve the periosteum. Common causes include odontogenic infections, trauma, infections of nearby regions, and hematogenous spread. The document classifies osteomyelitis and describes the features of acute suppurative, chronic suppurative, nonsuppurative, infantile, and other specific types. Treatment involves antibiotics, surgical drainage and debridement, hyperbaric oxygen therapy, and reconstruction in severe cases. Complications like necrosis and pathological fractures are also mentioned