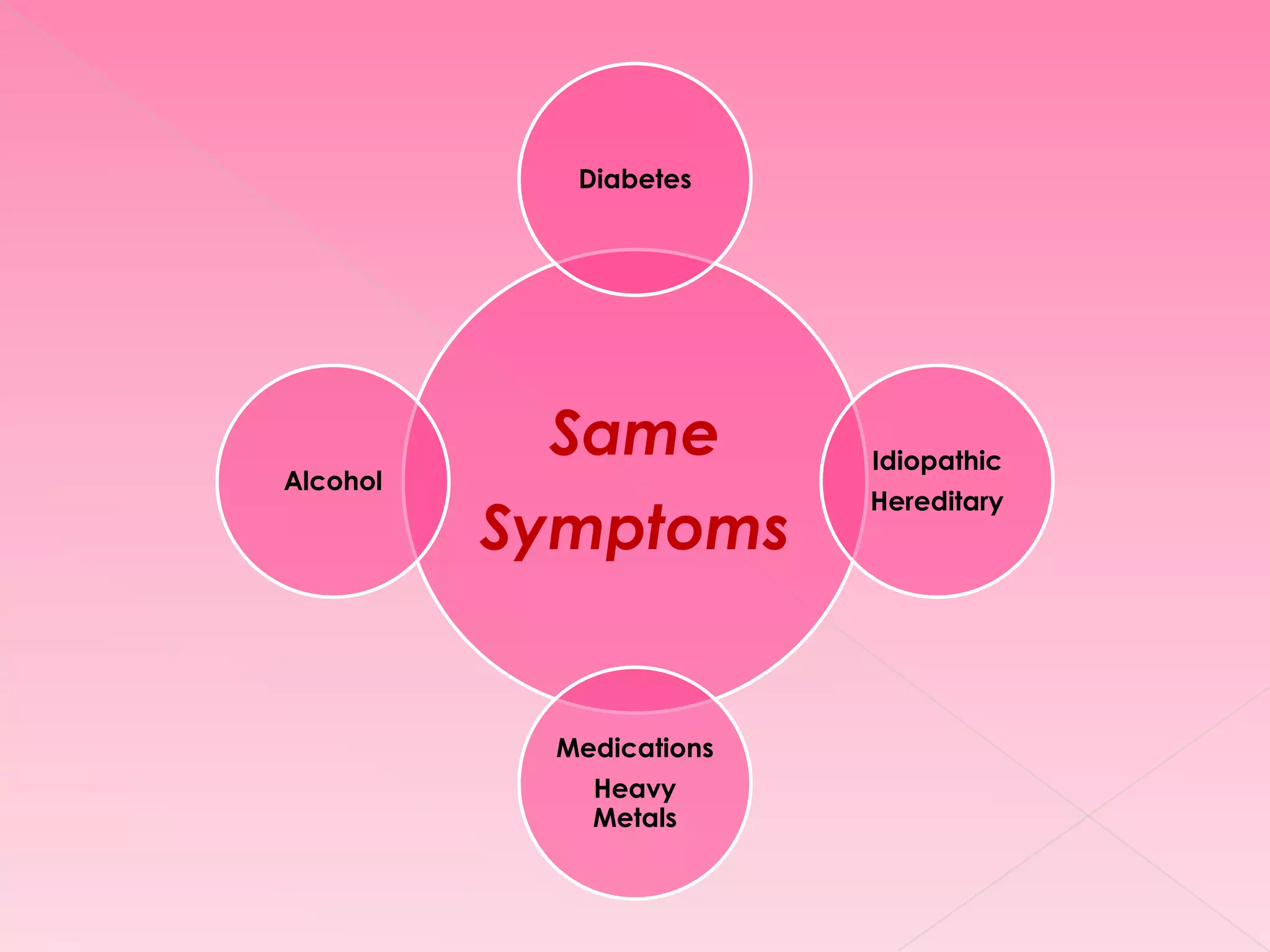
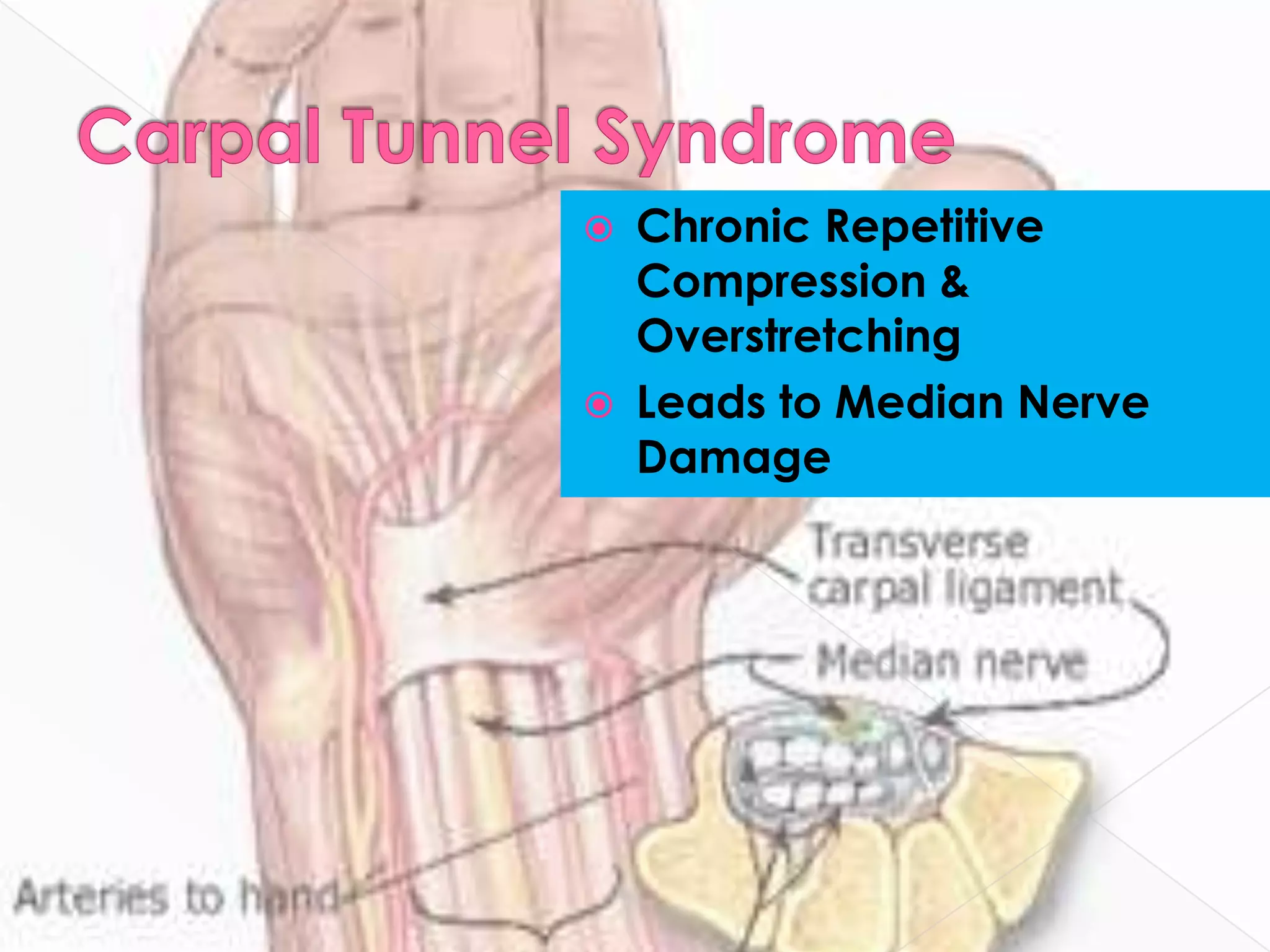
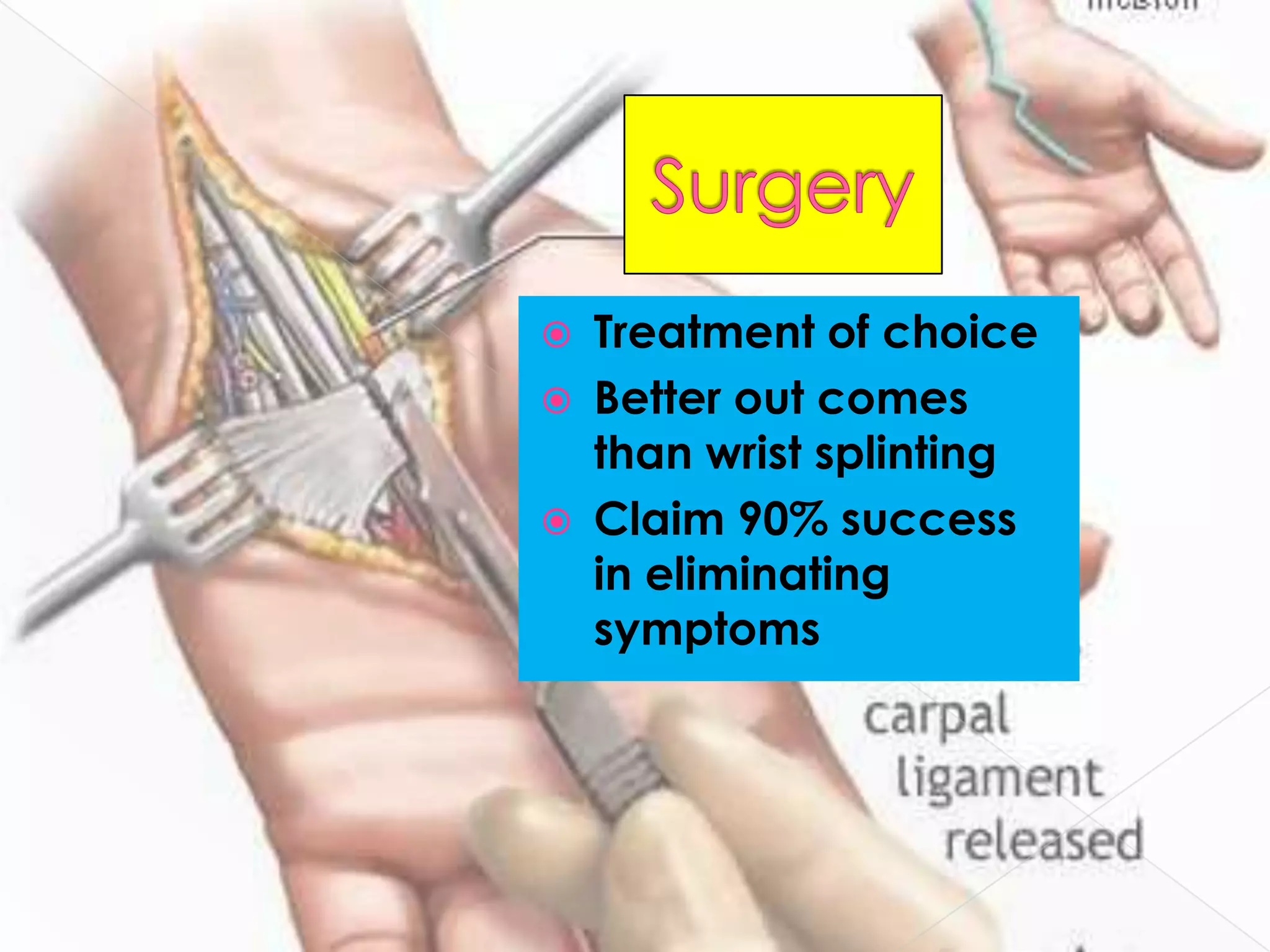
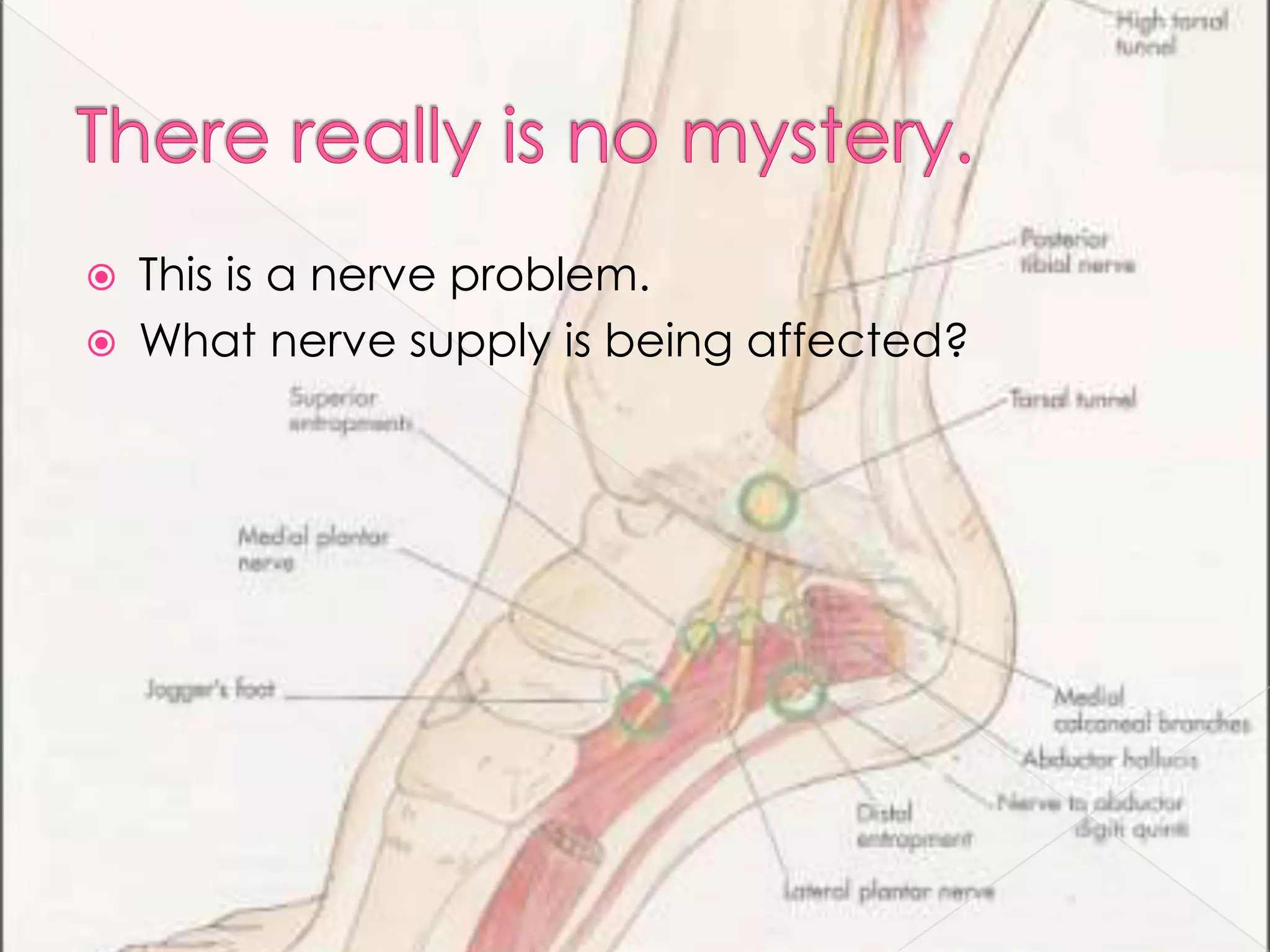
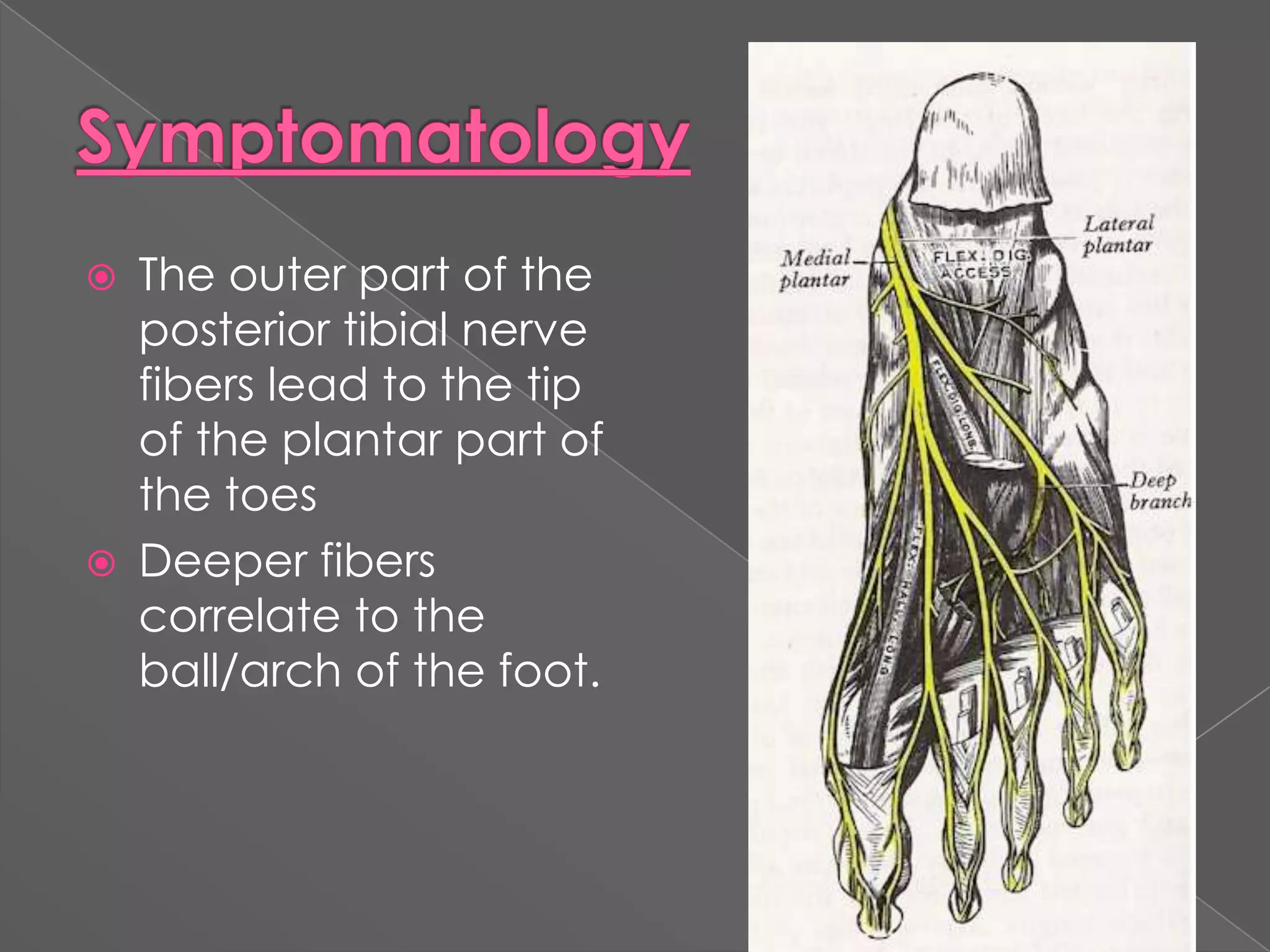
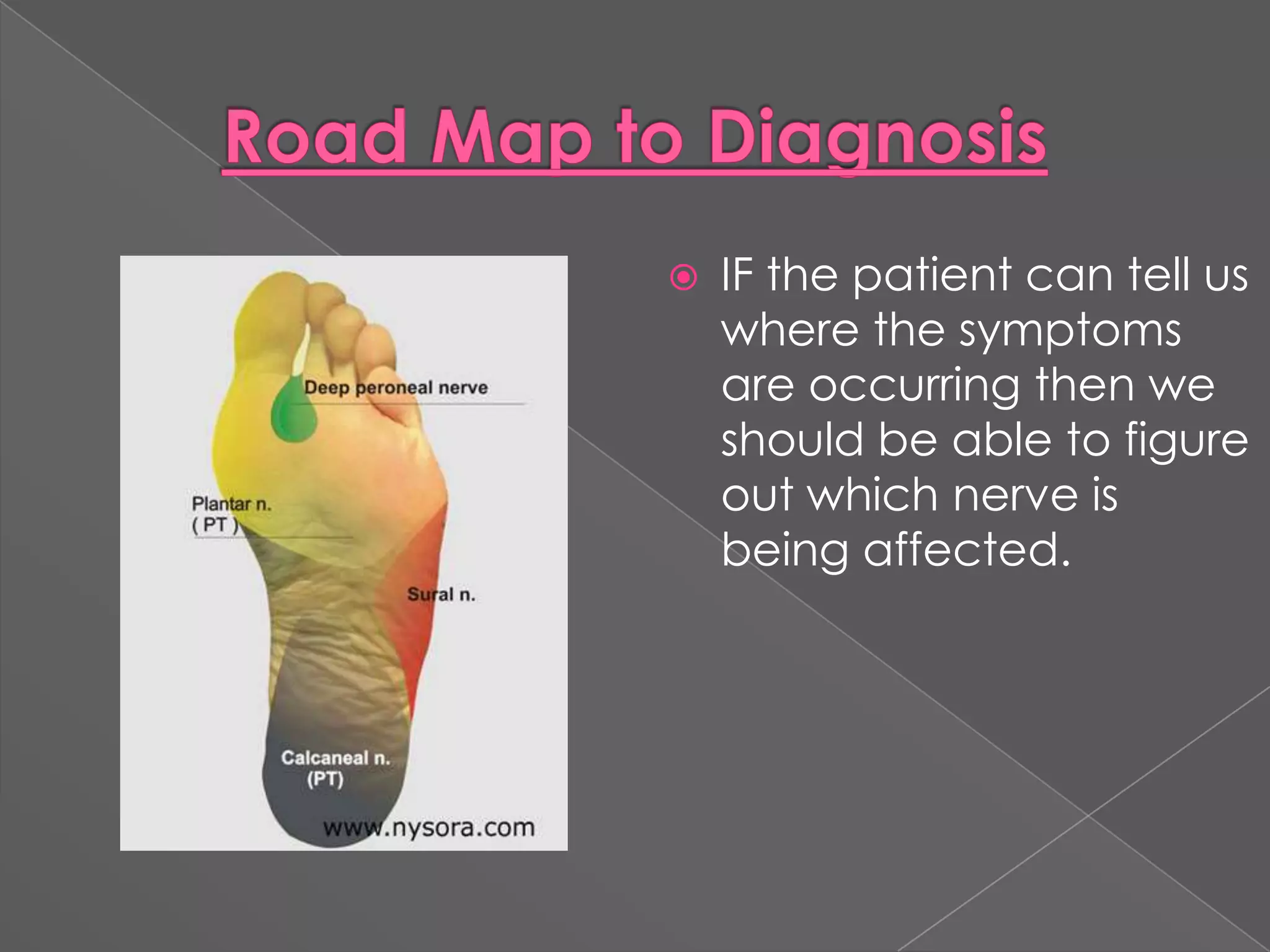
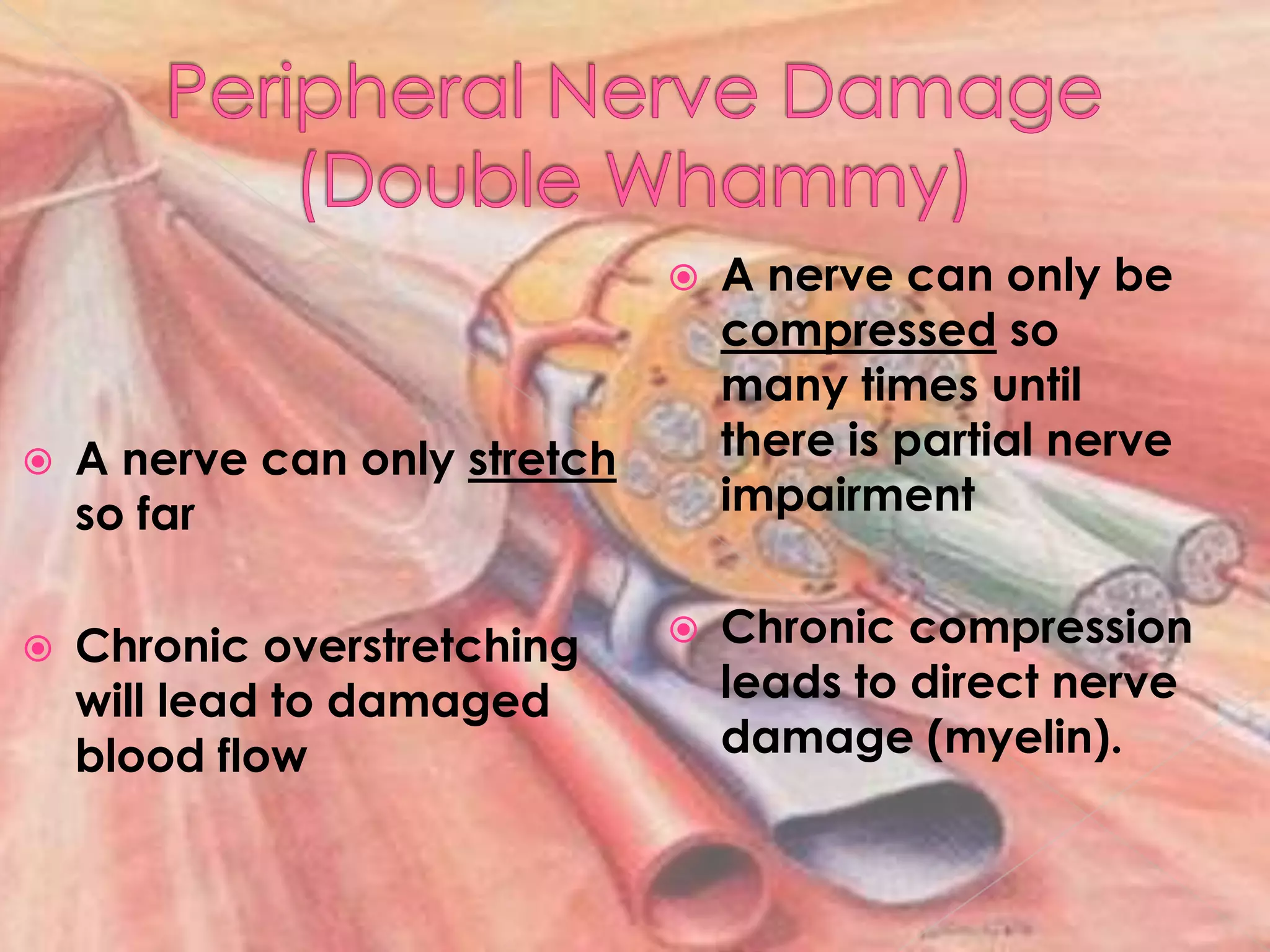
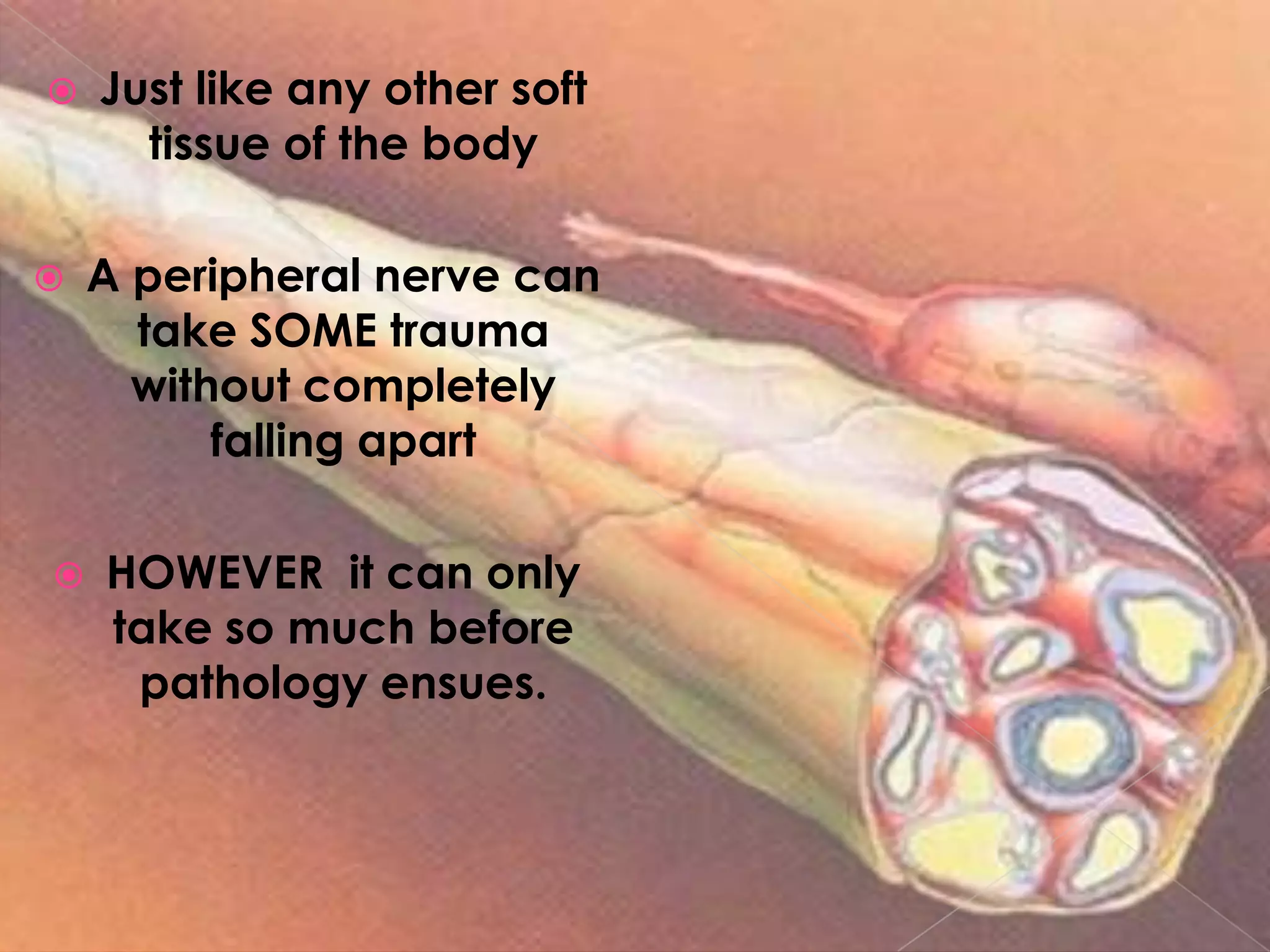
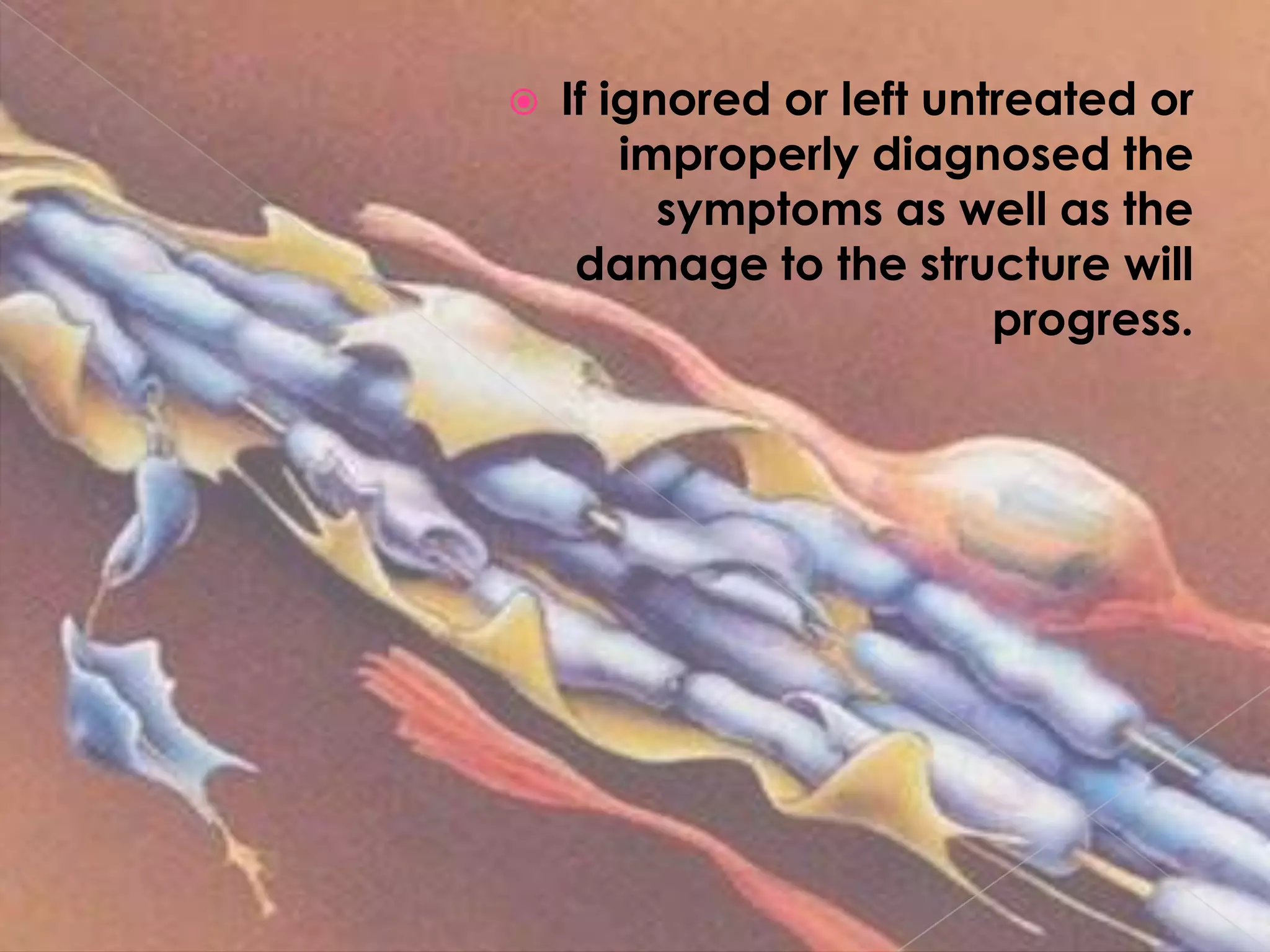
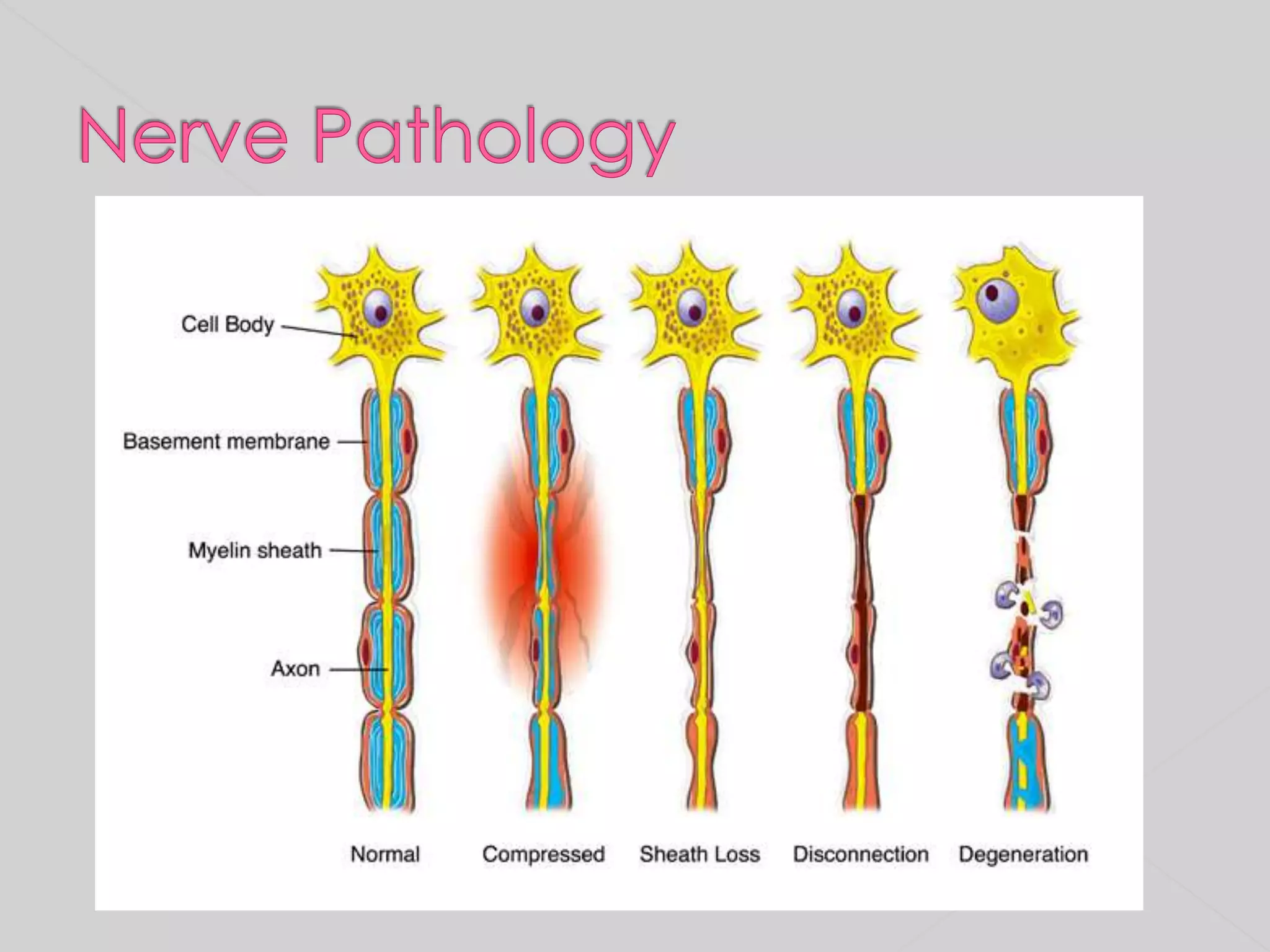
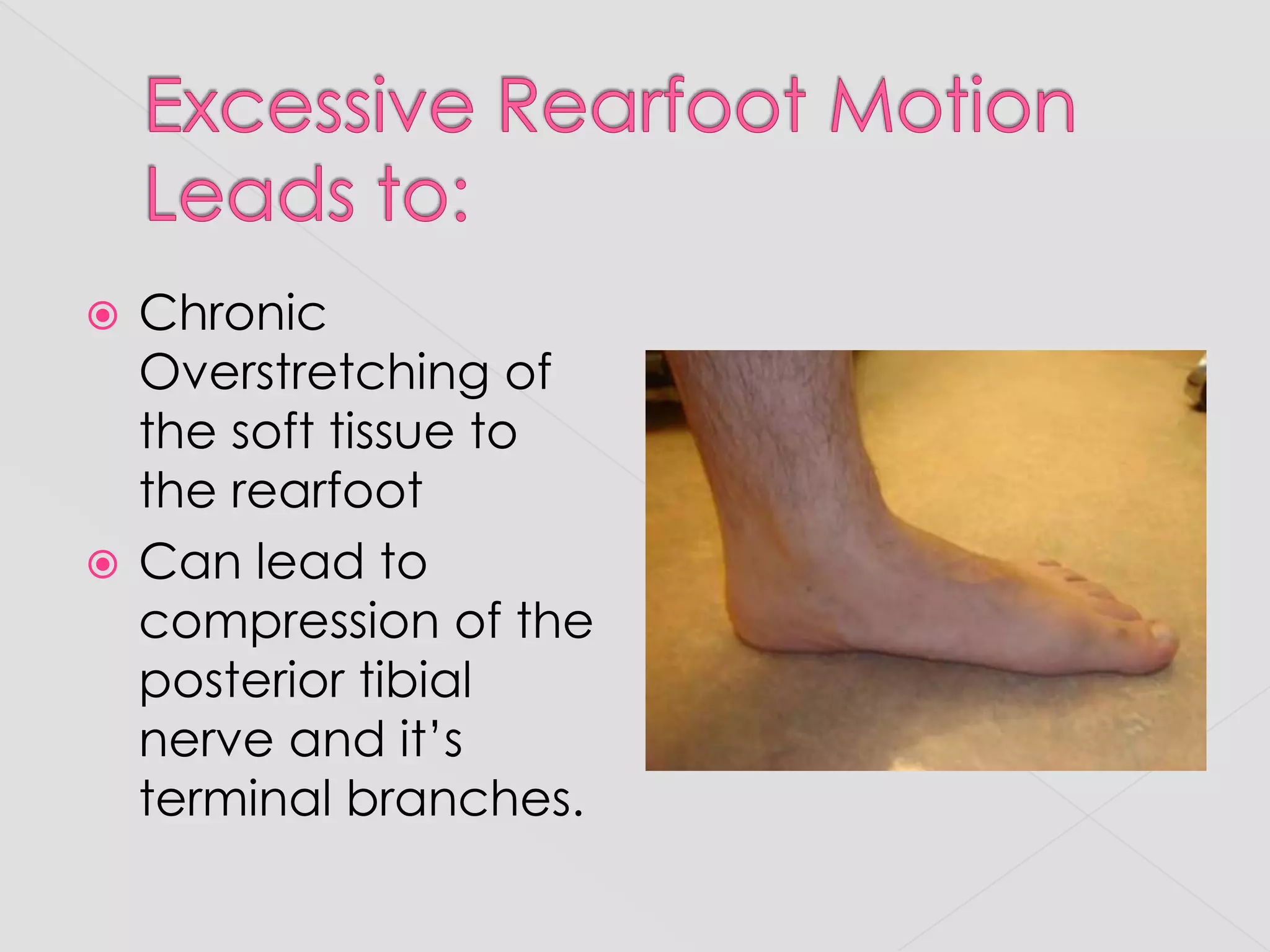
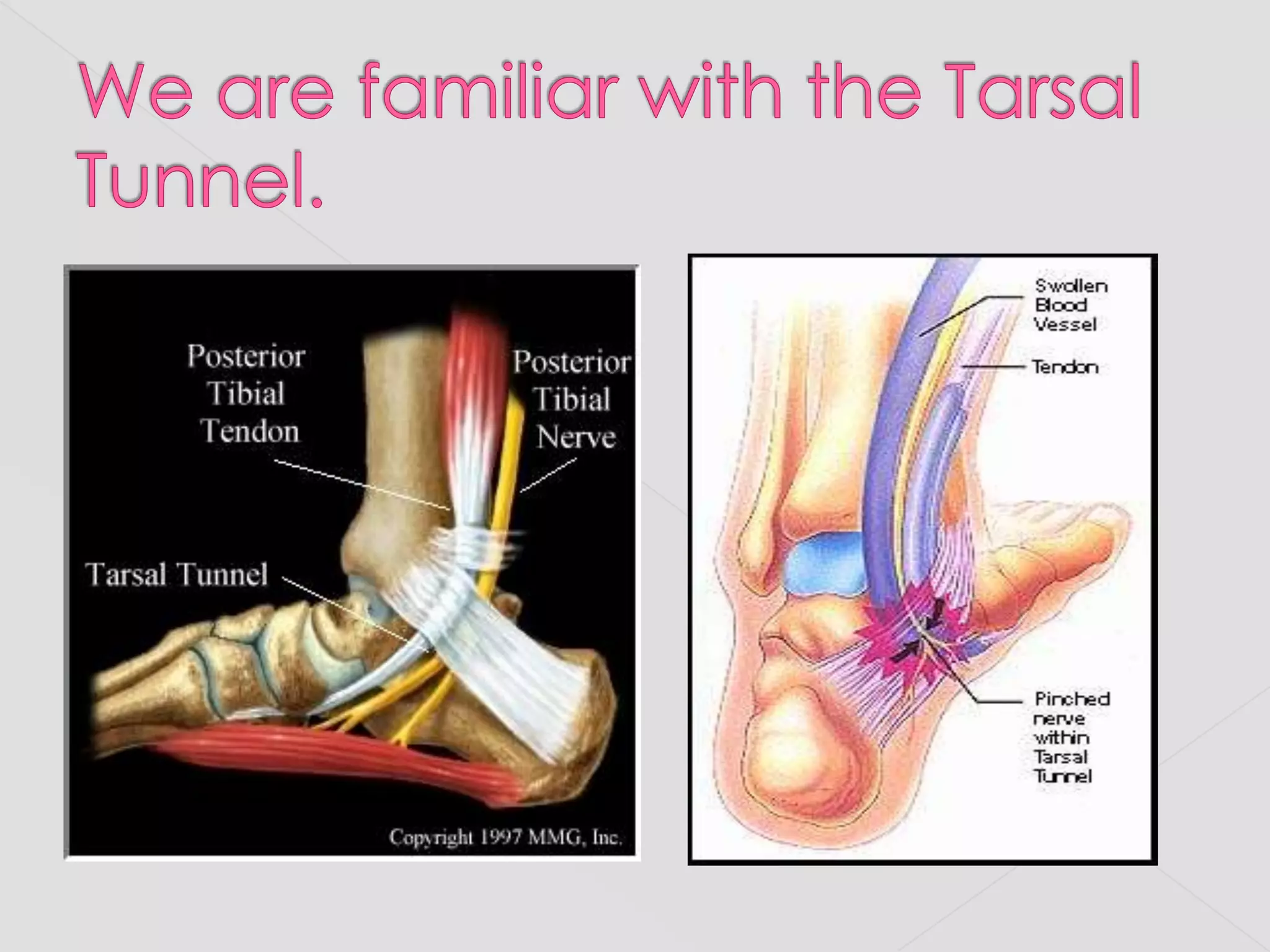
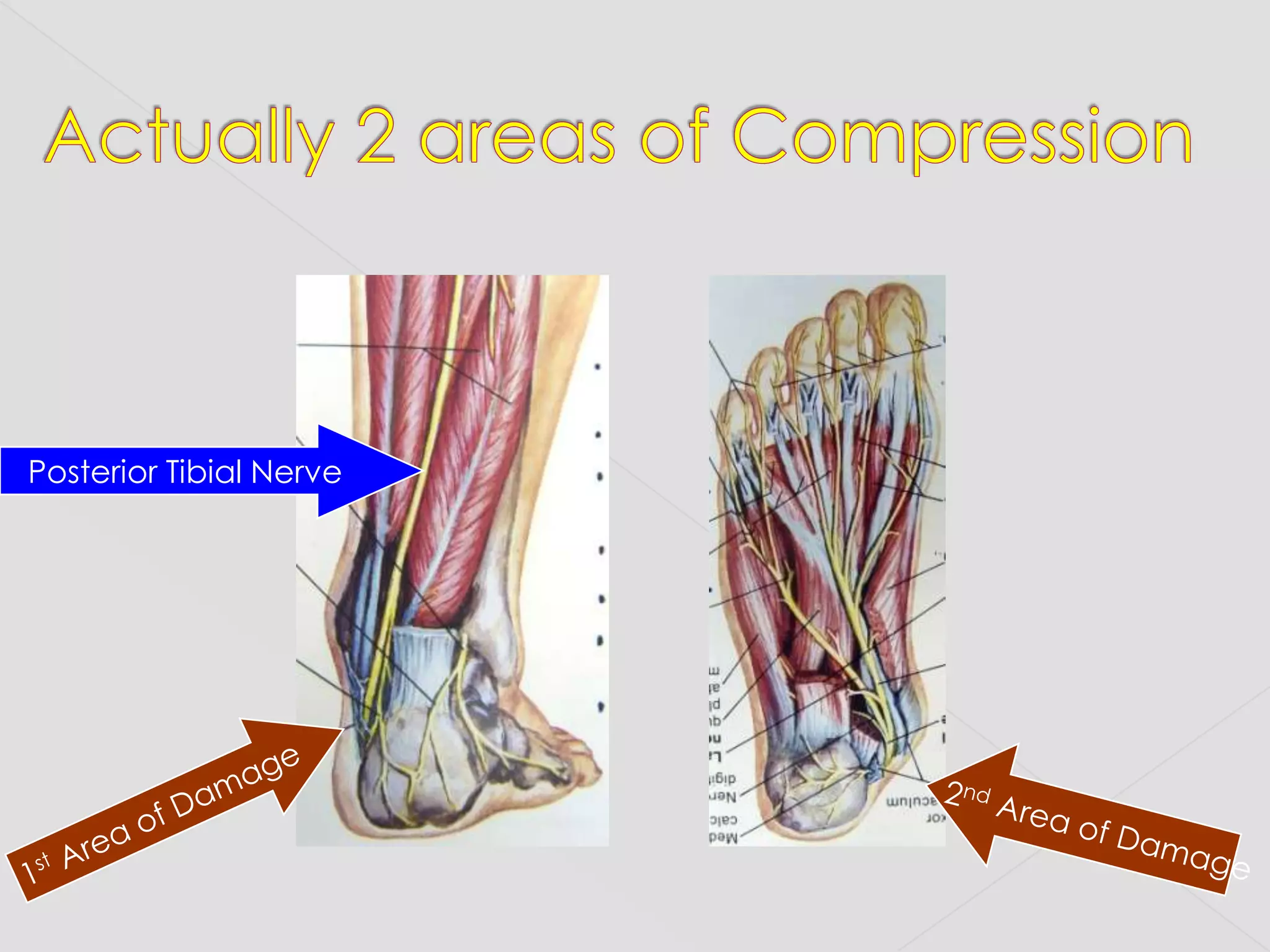
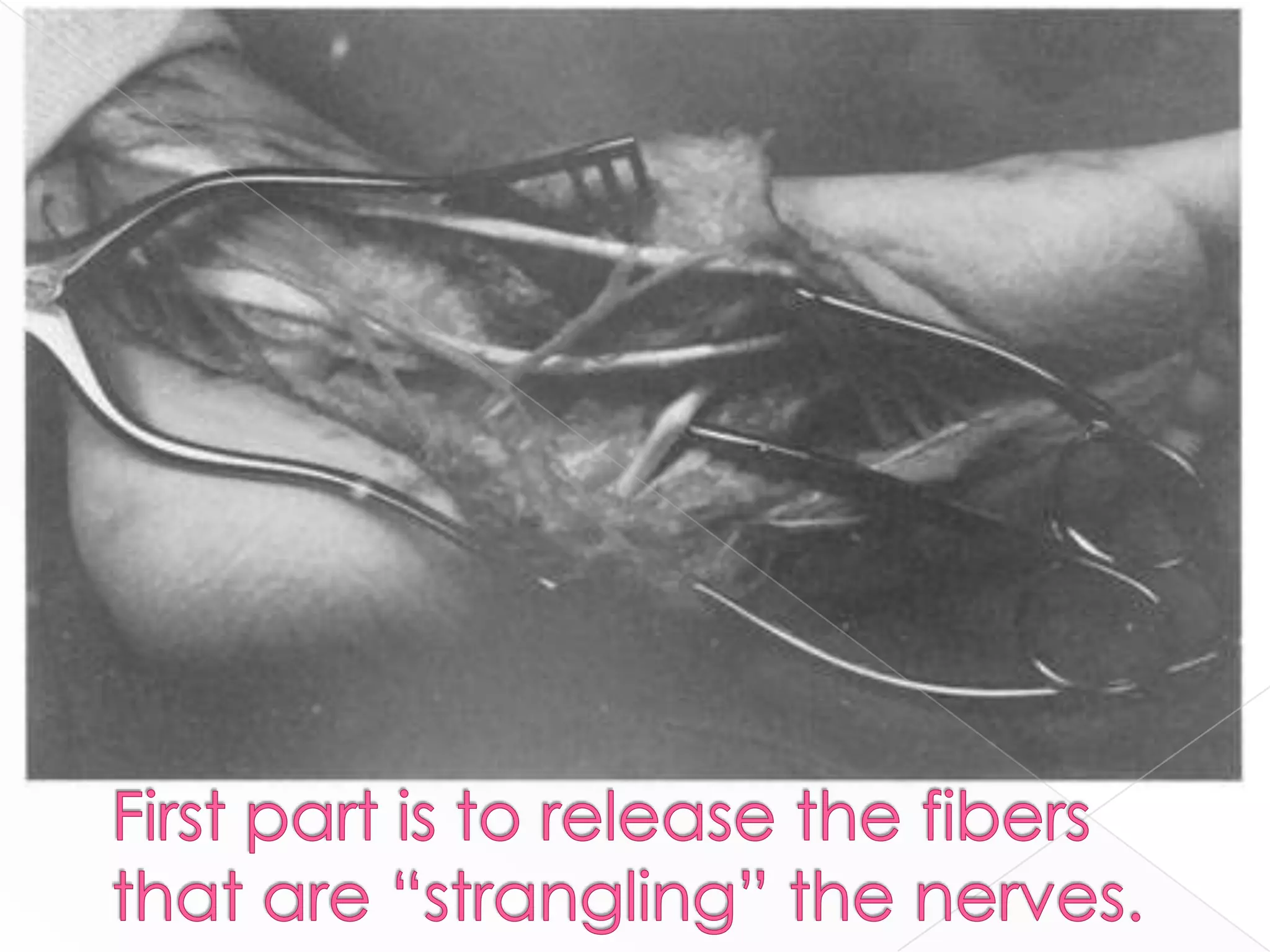
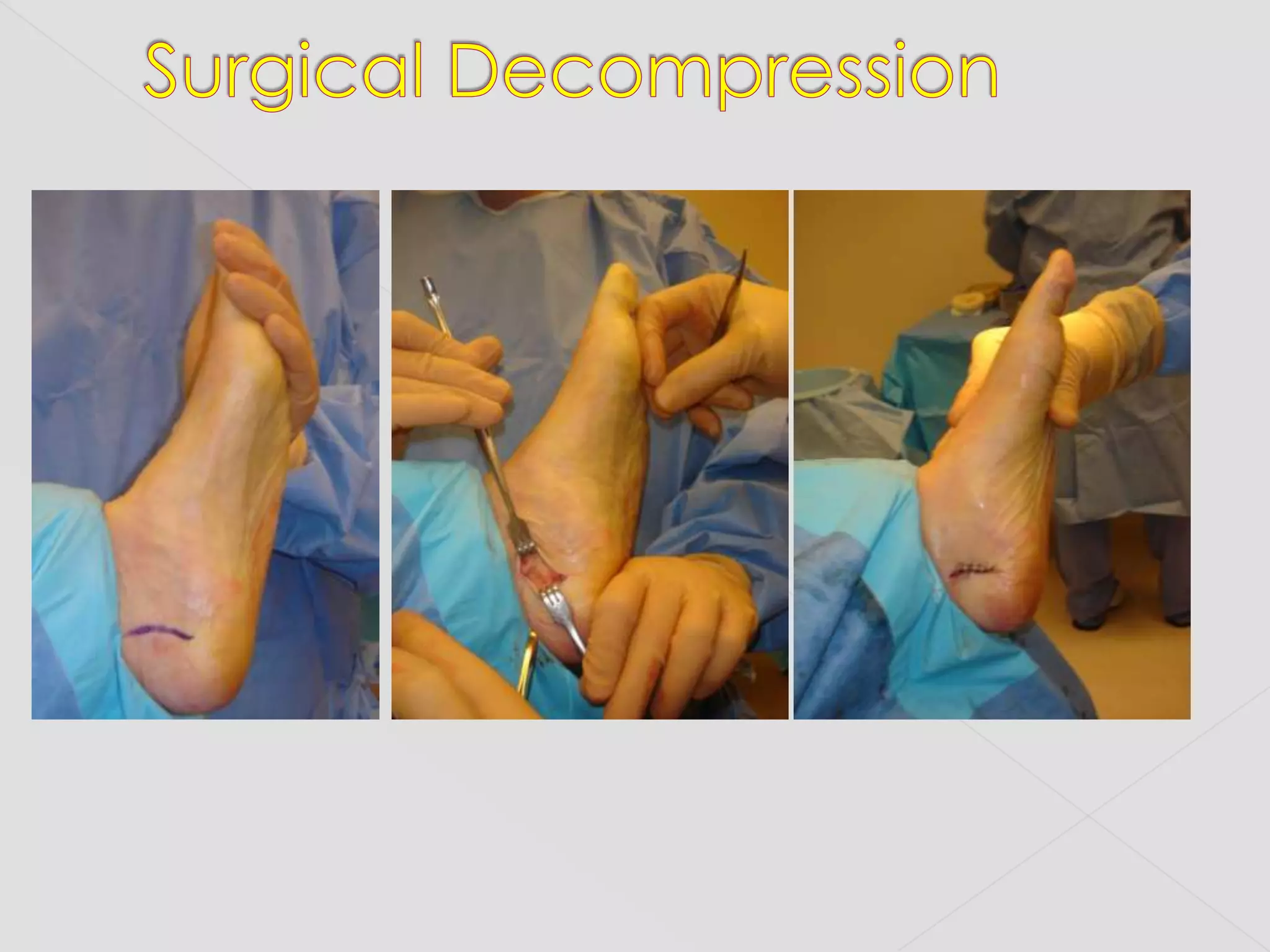
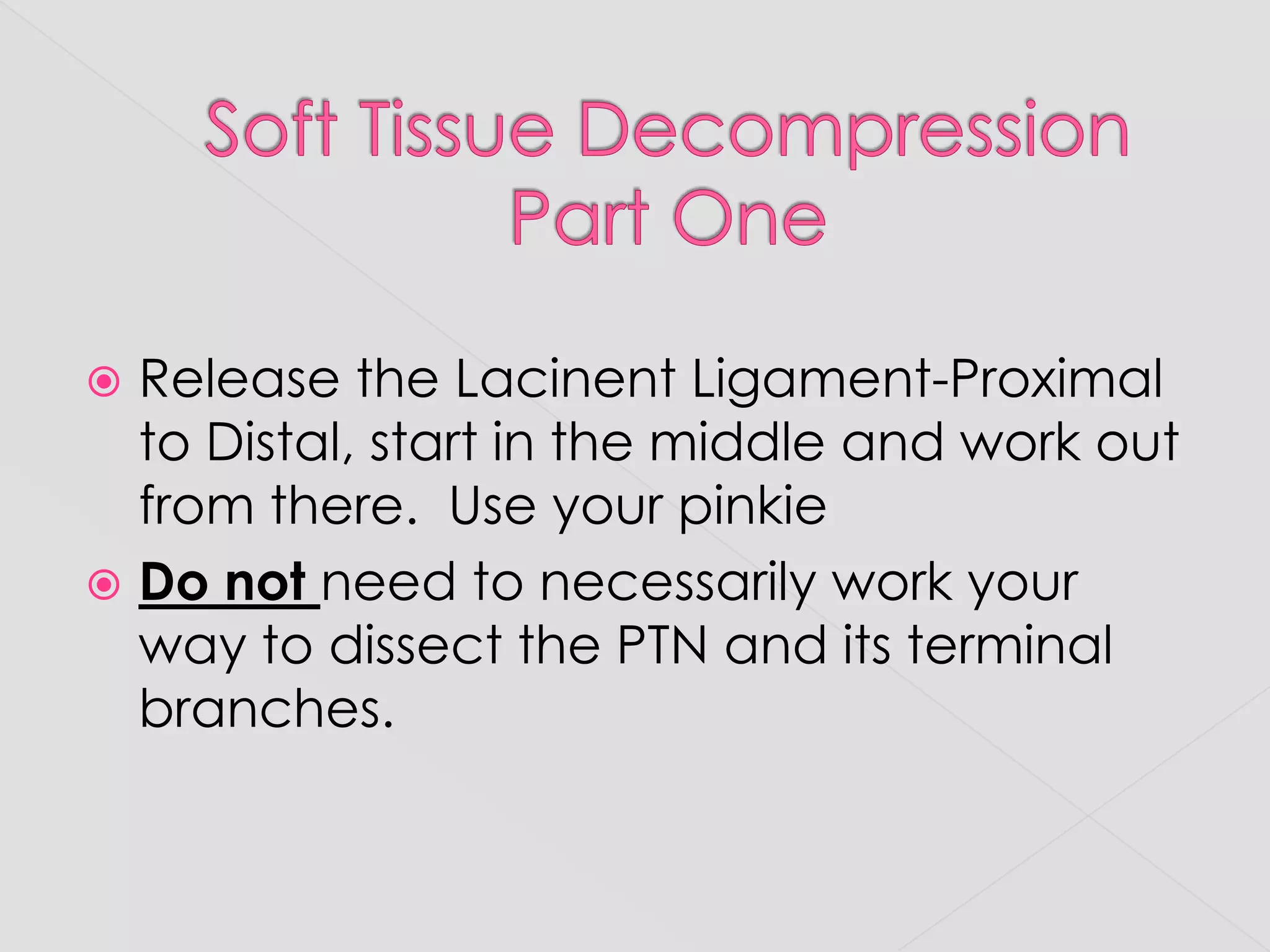
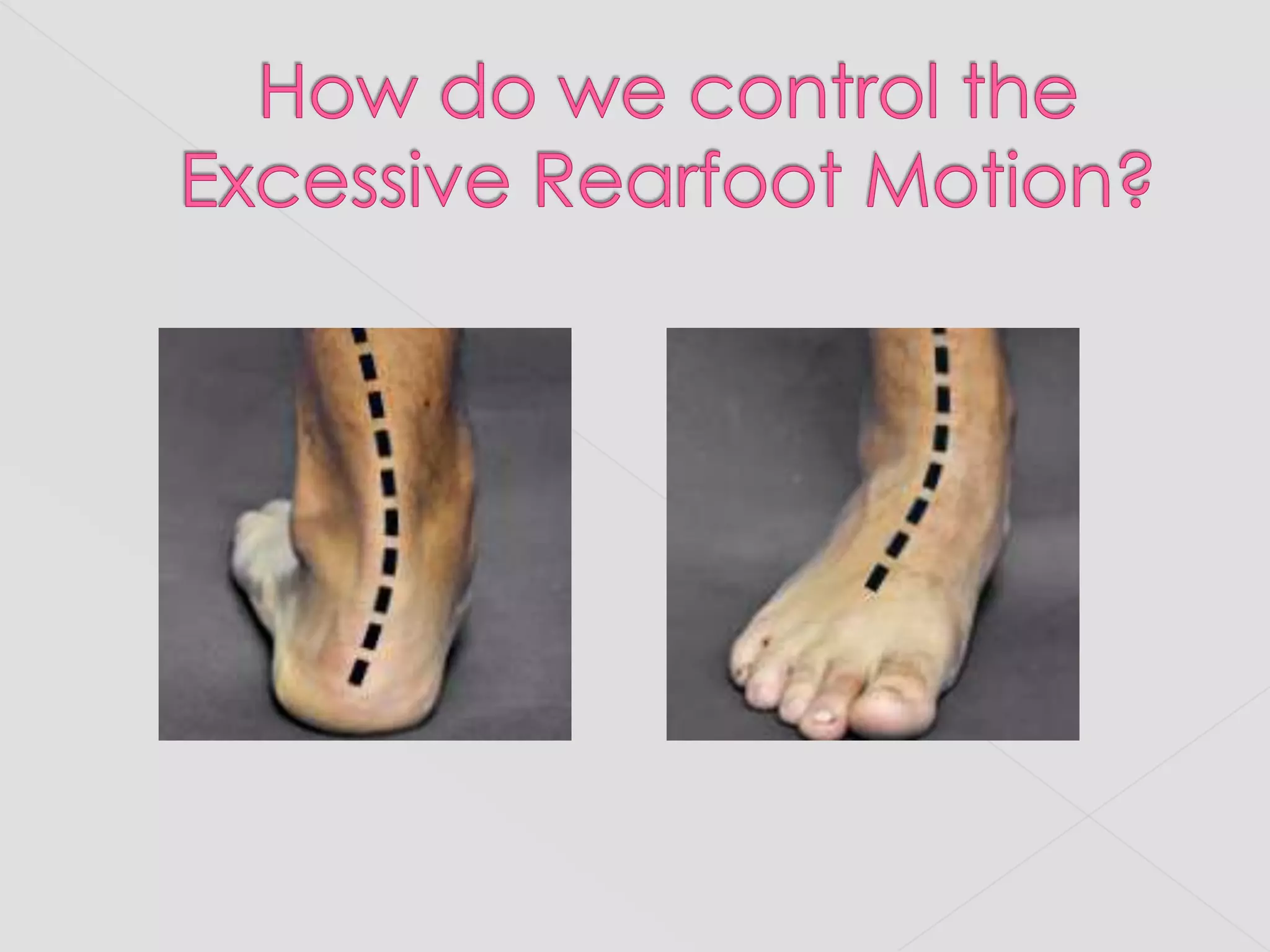
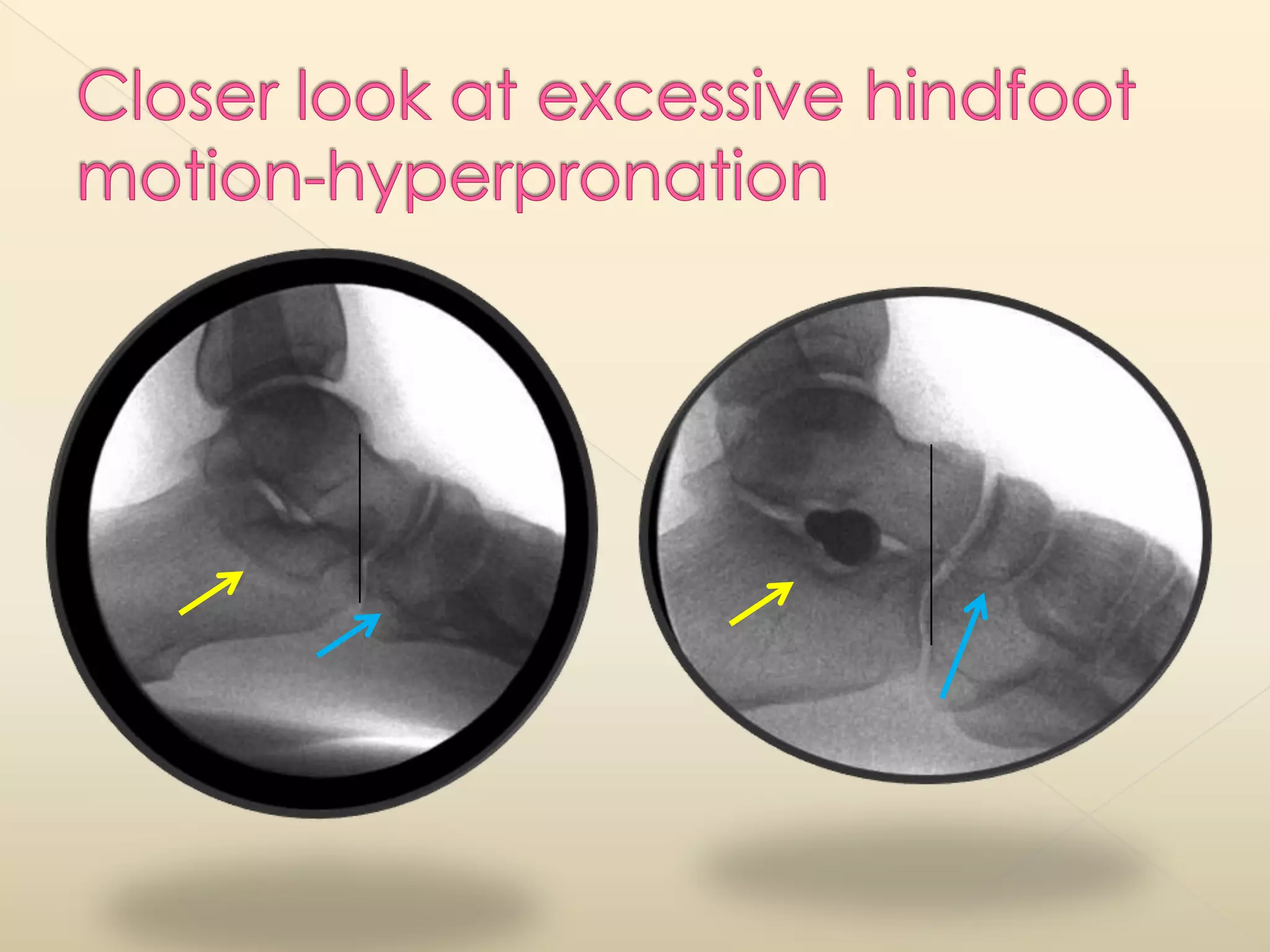
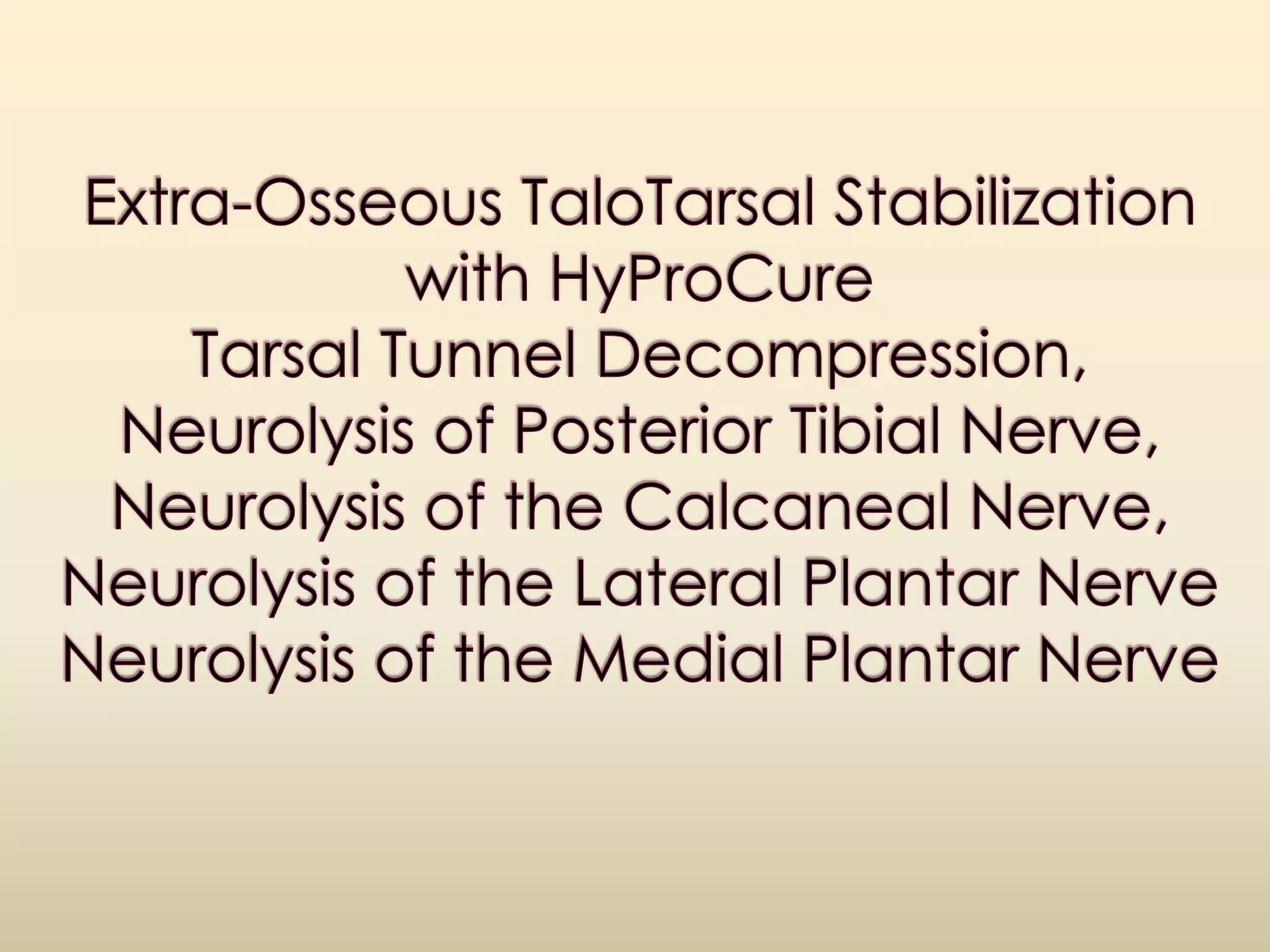
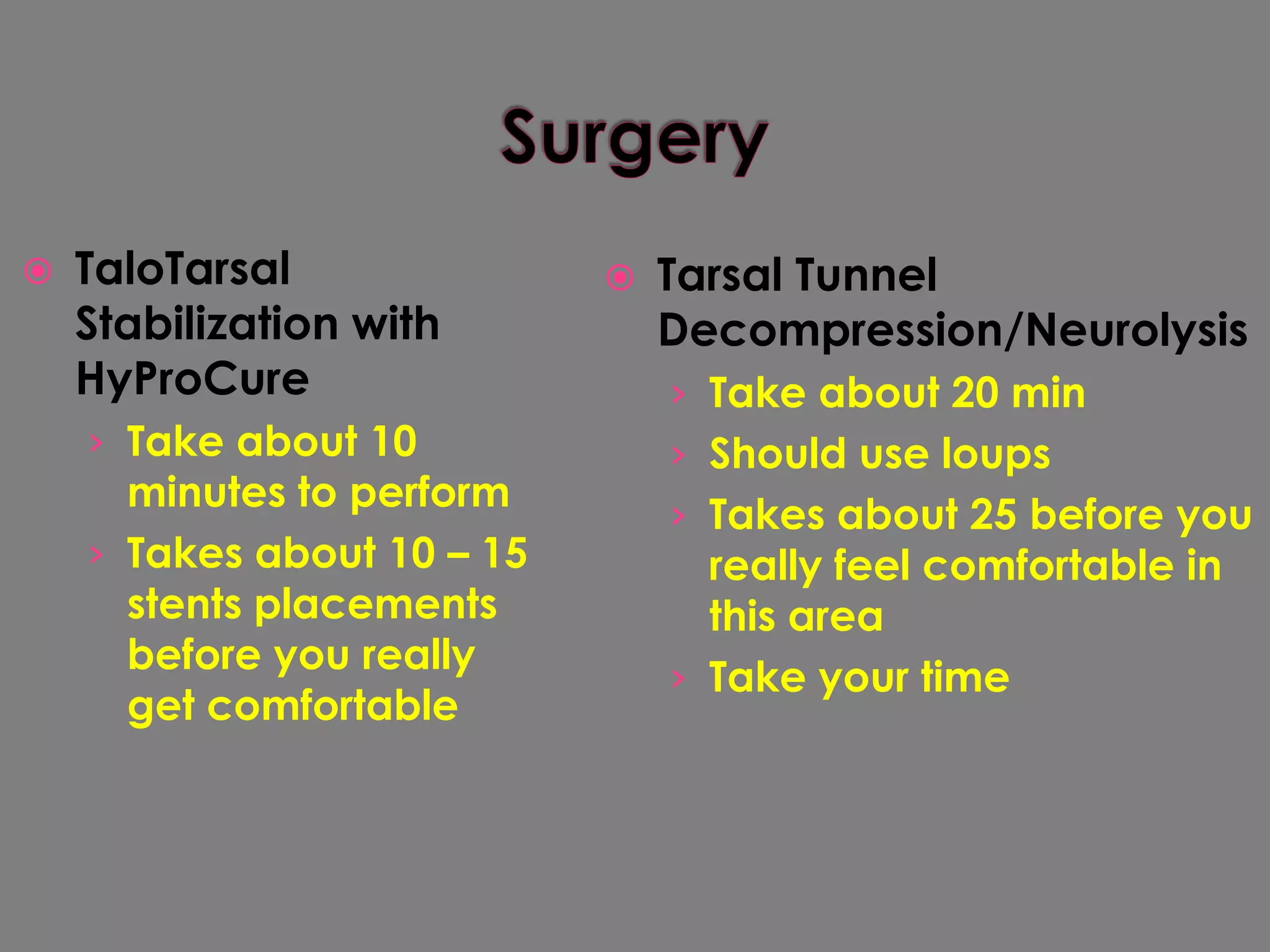
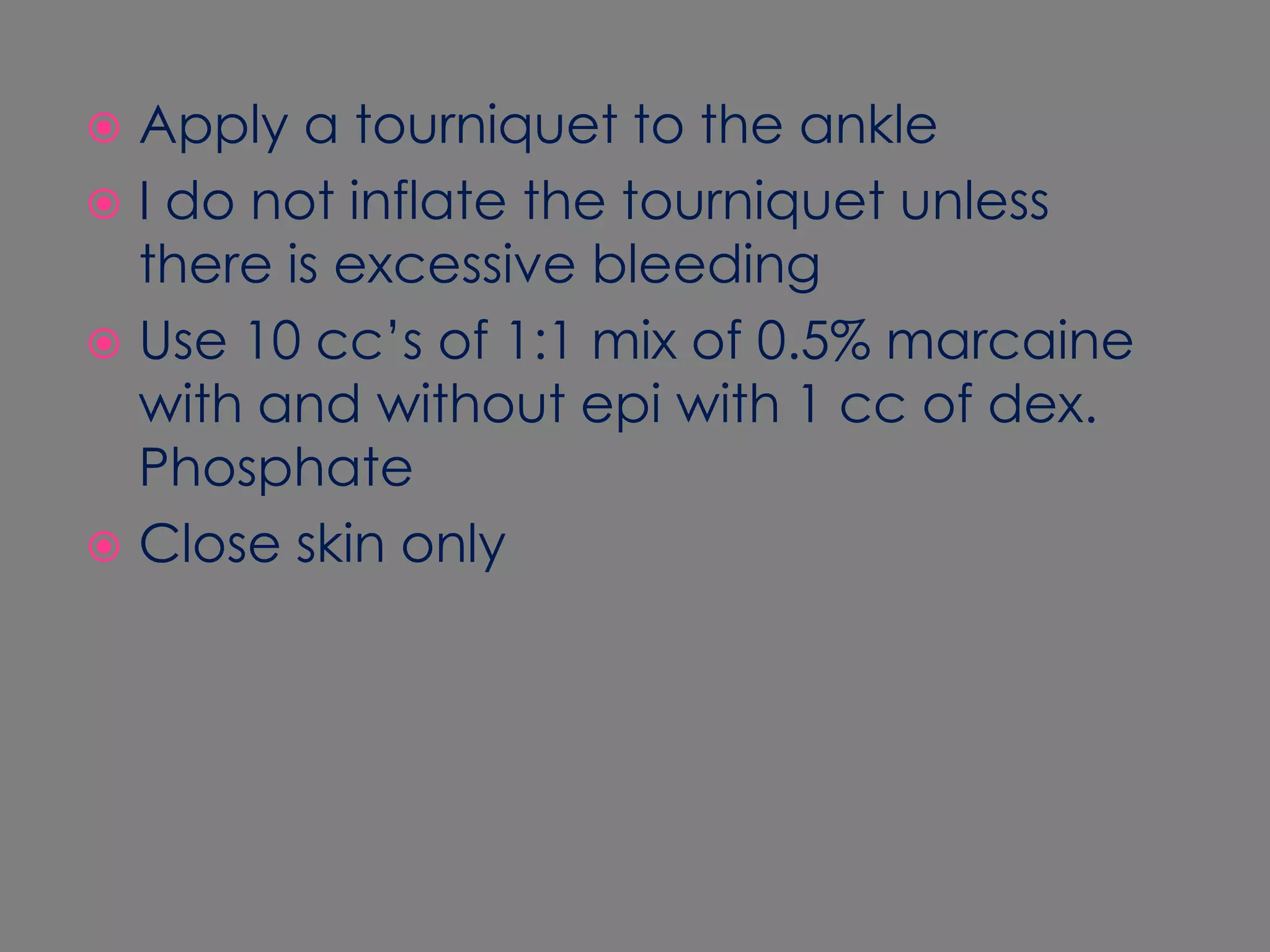
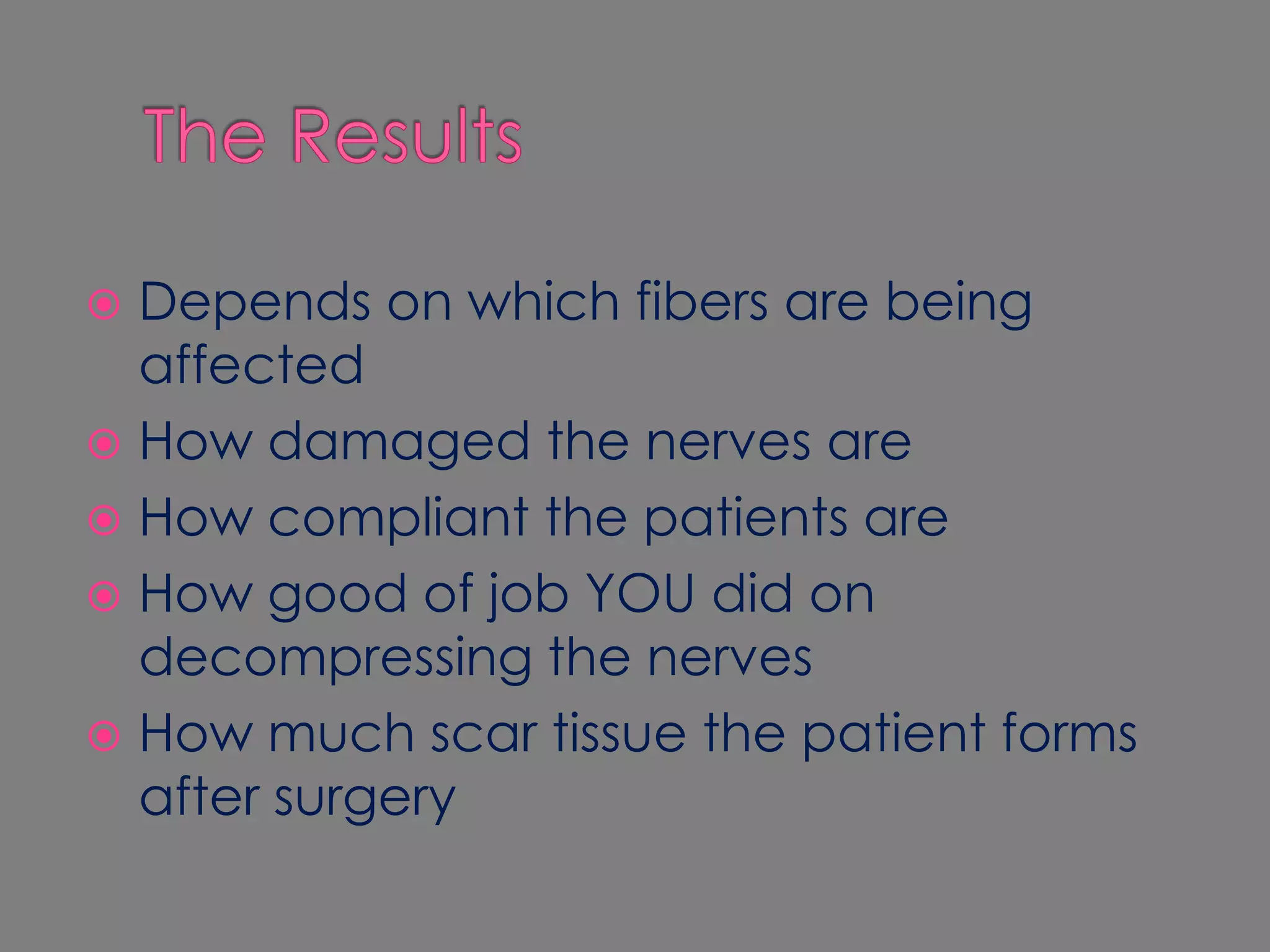
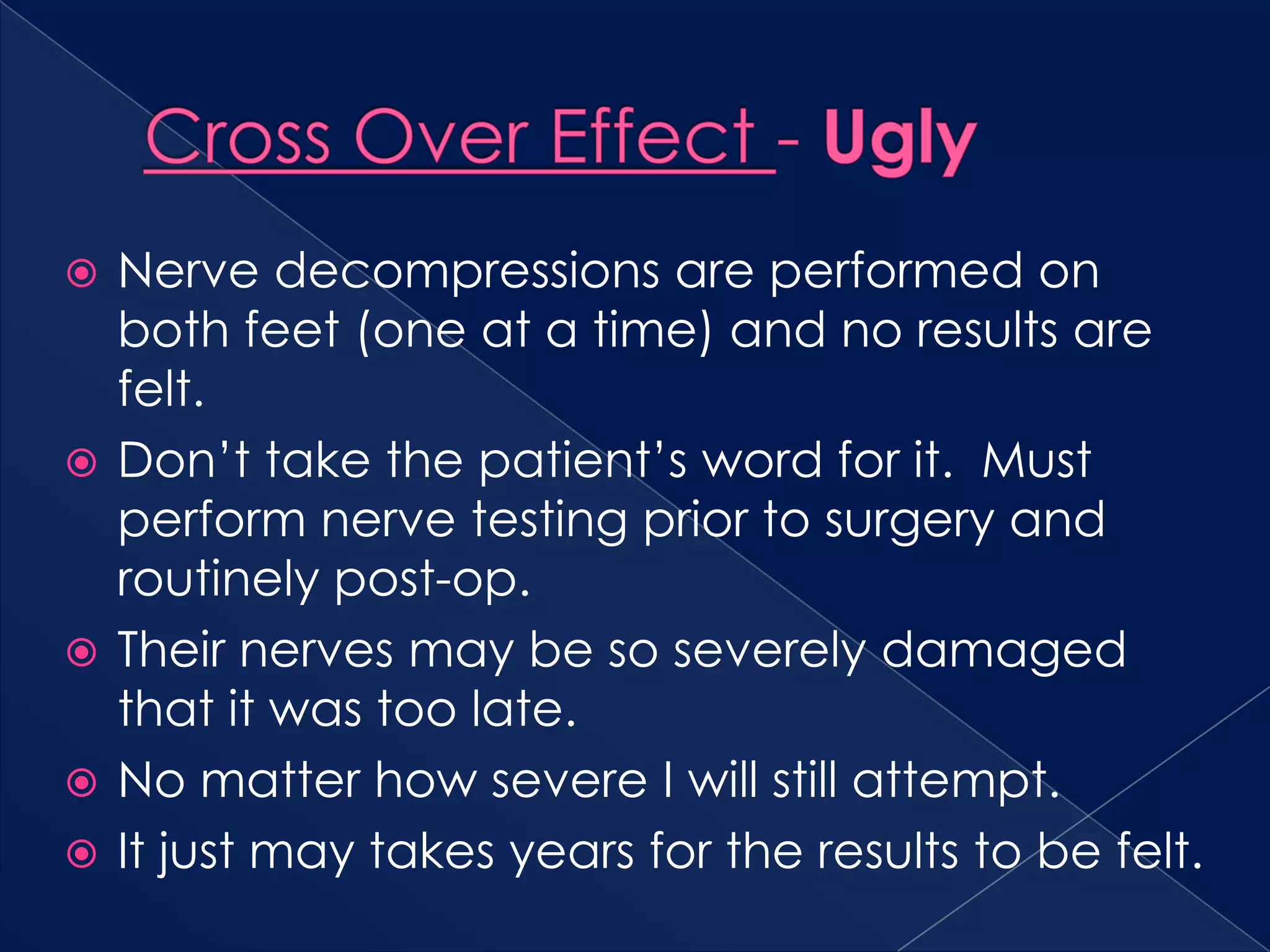
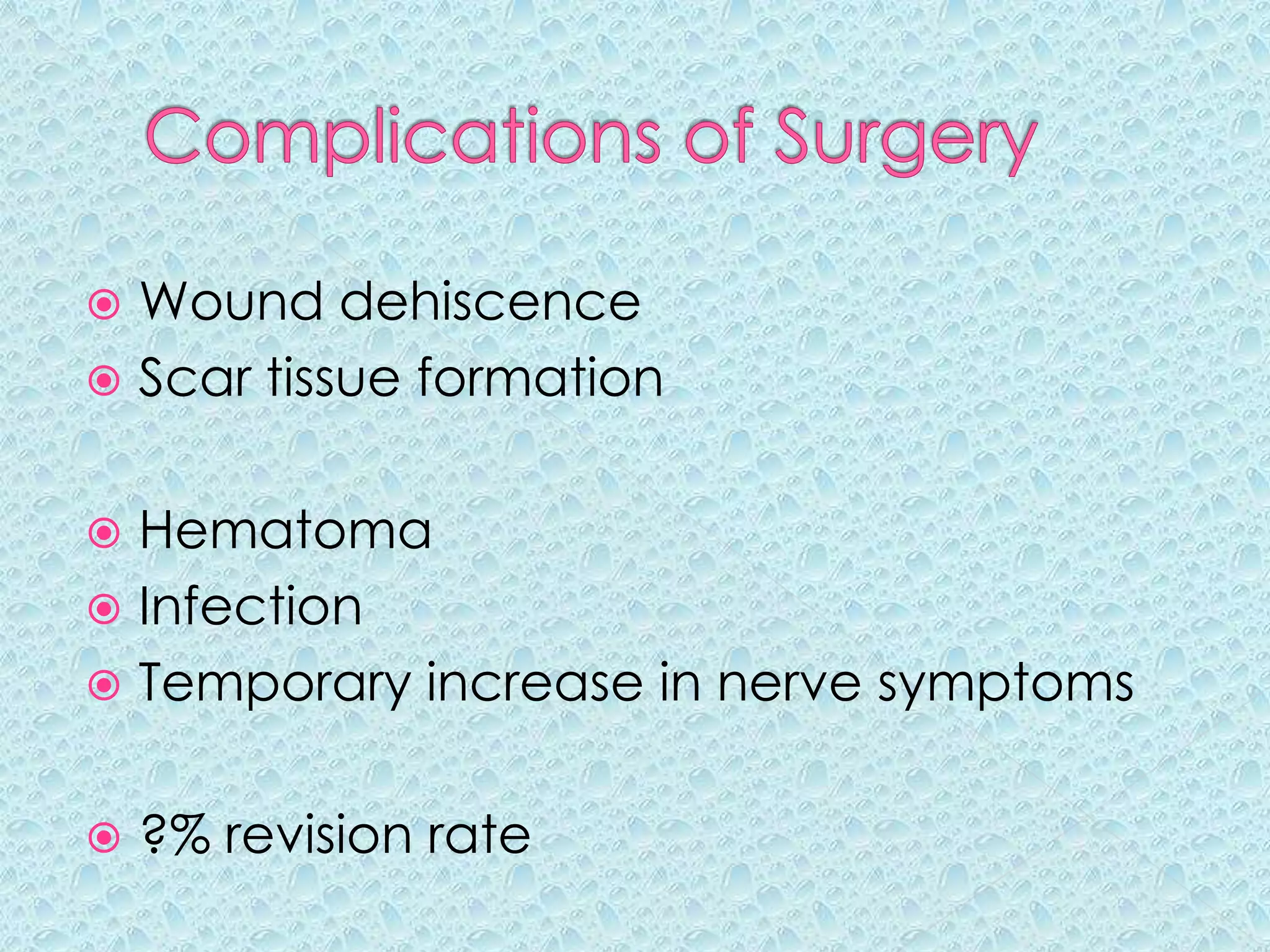
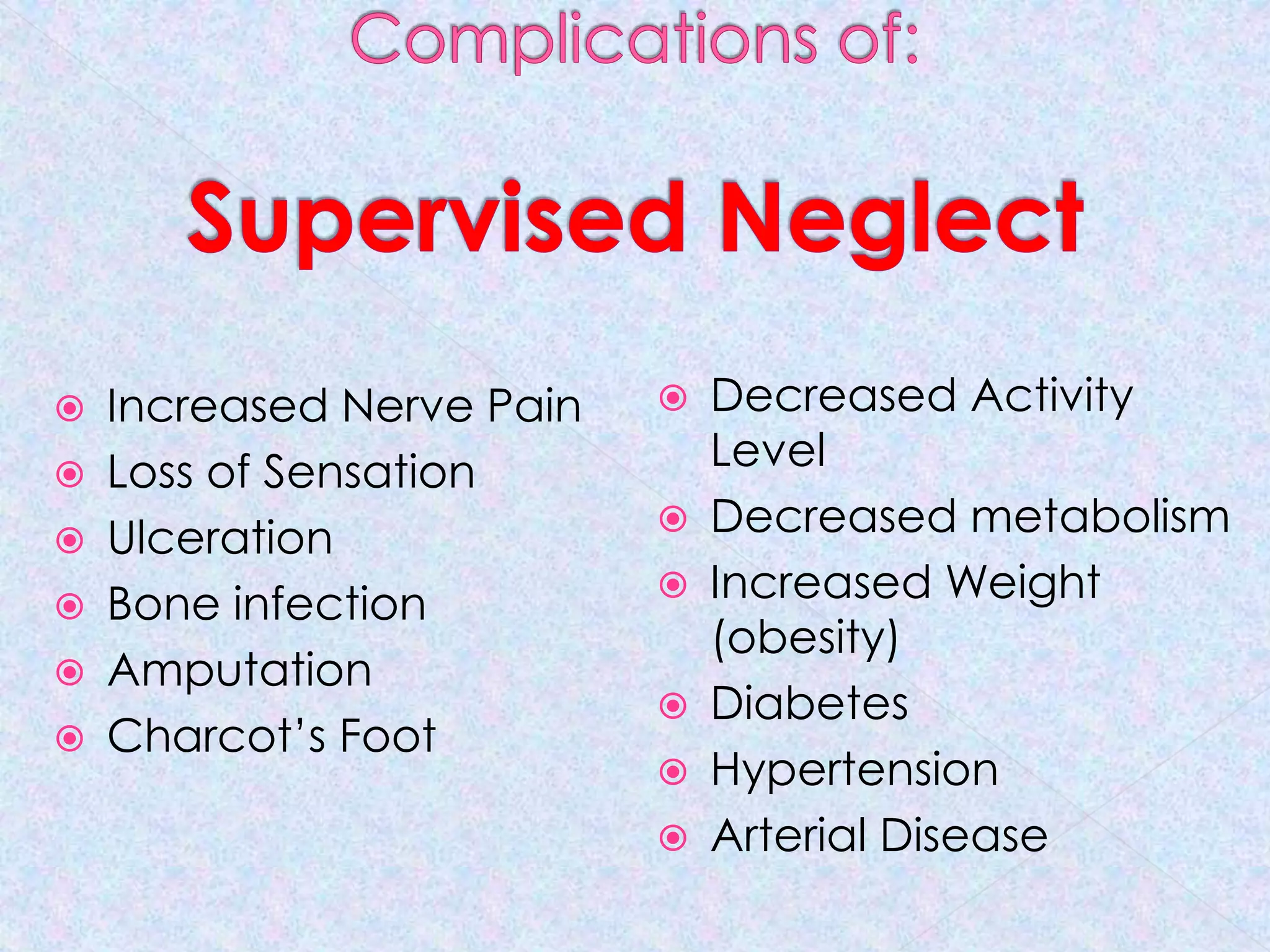
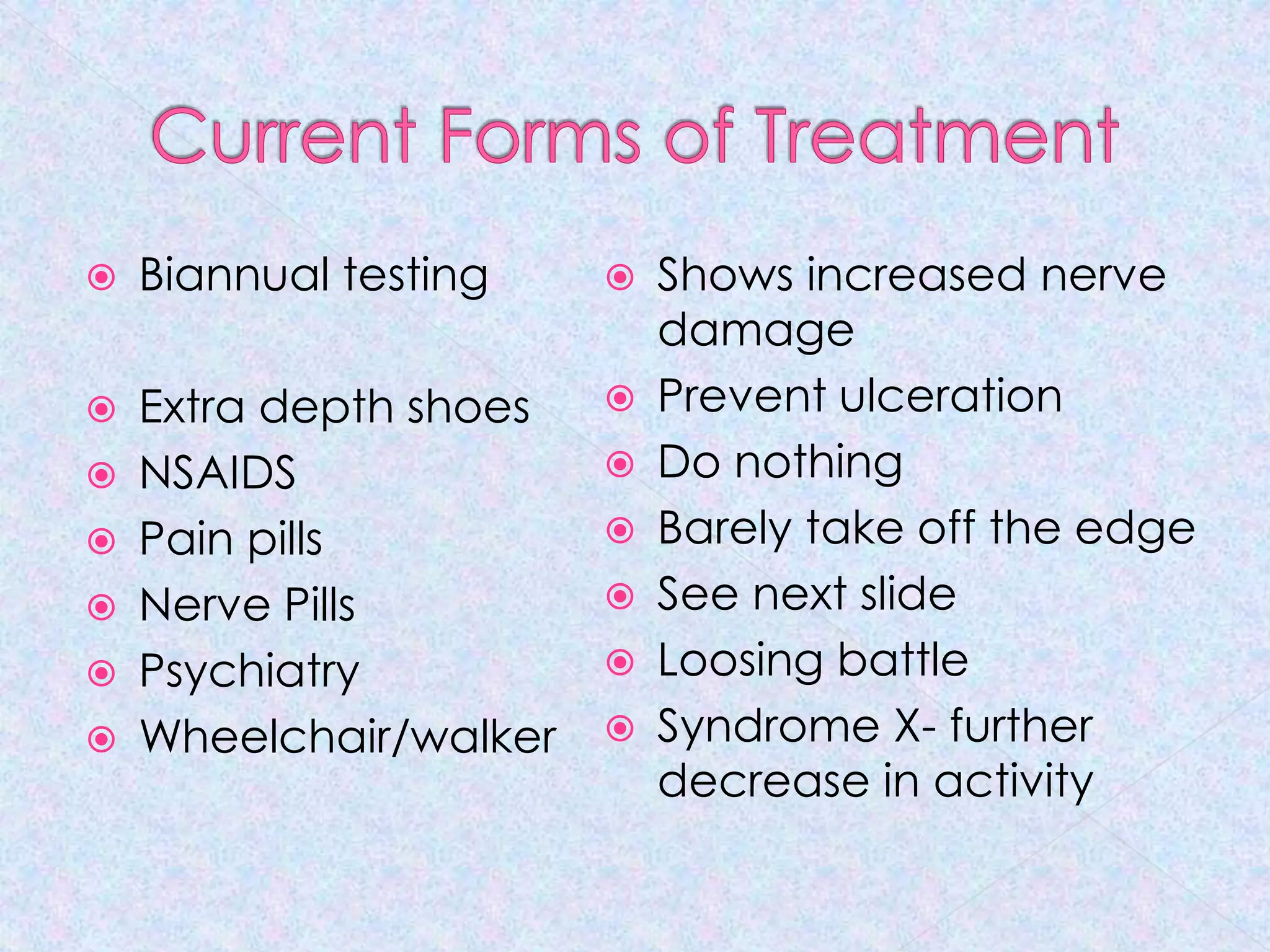
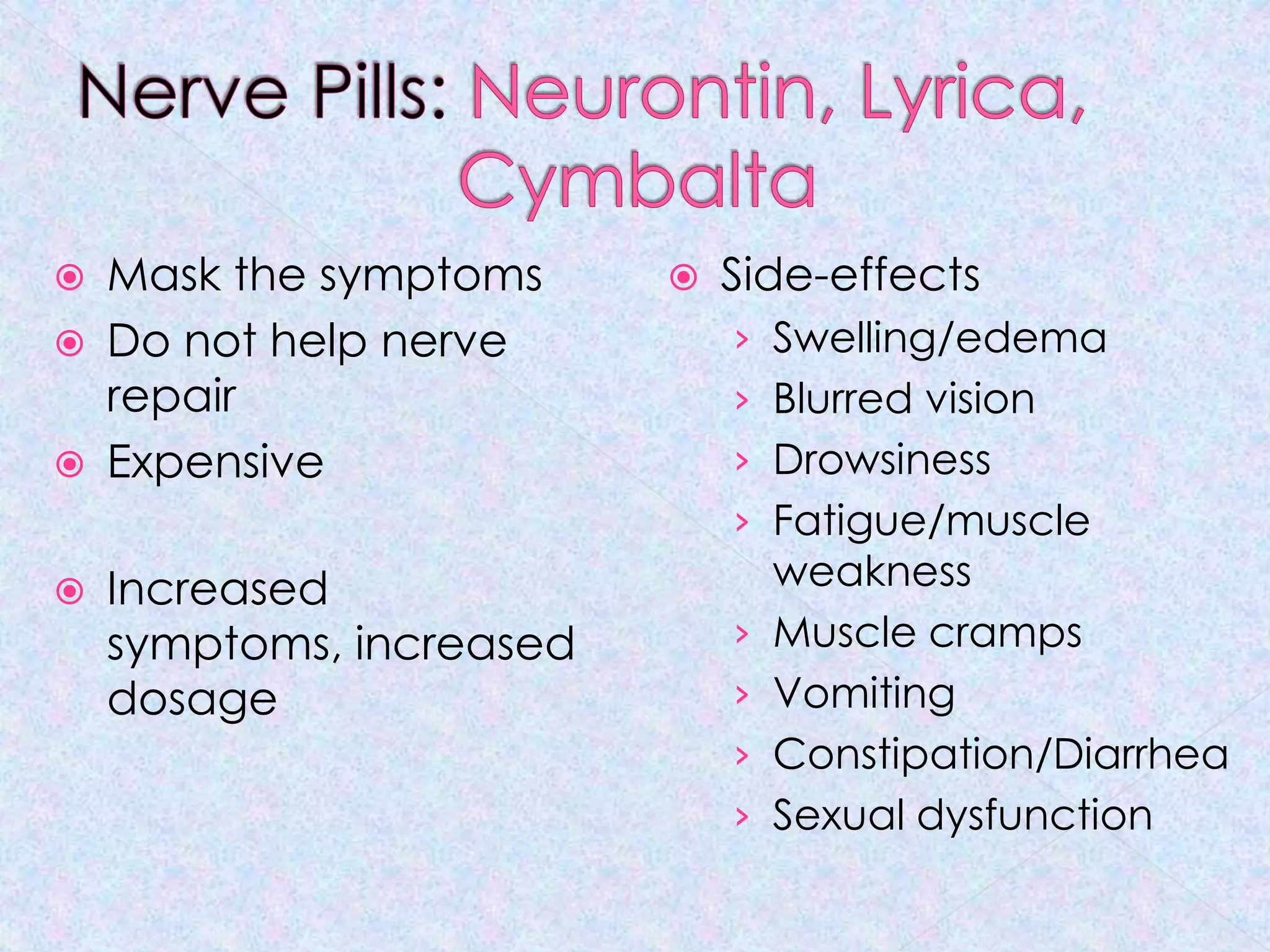
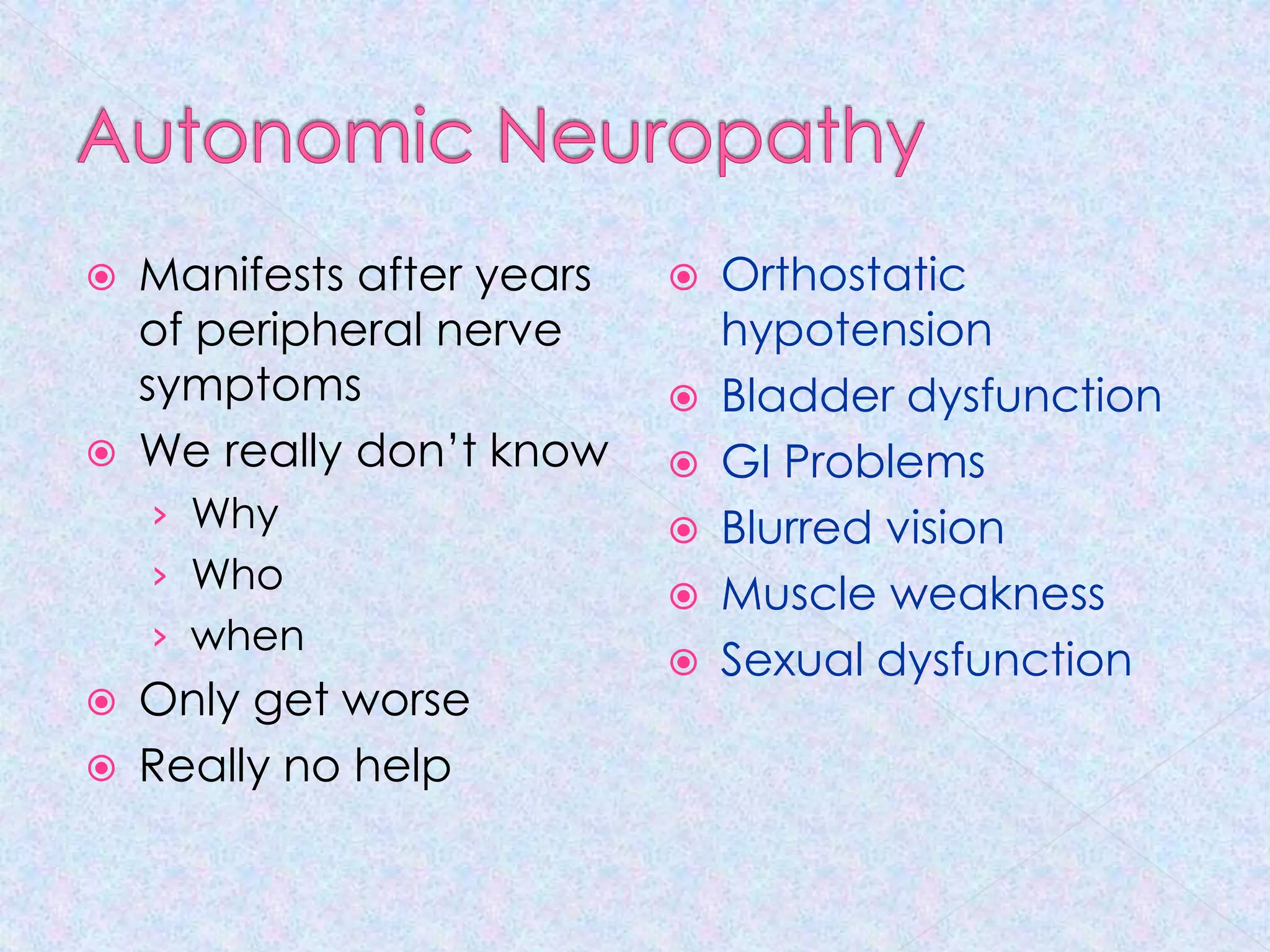
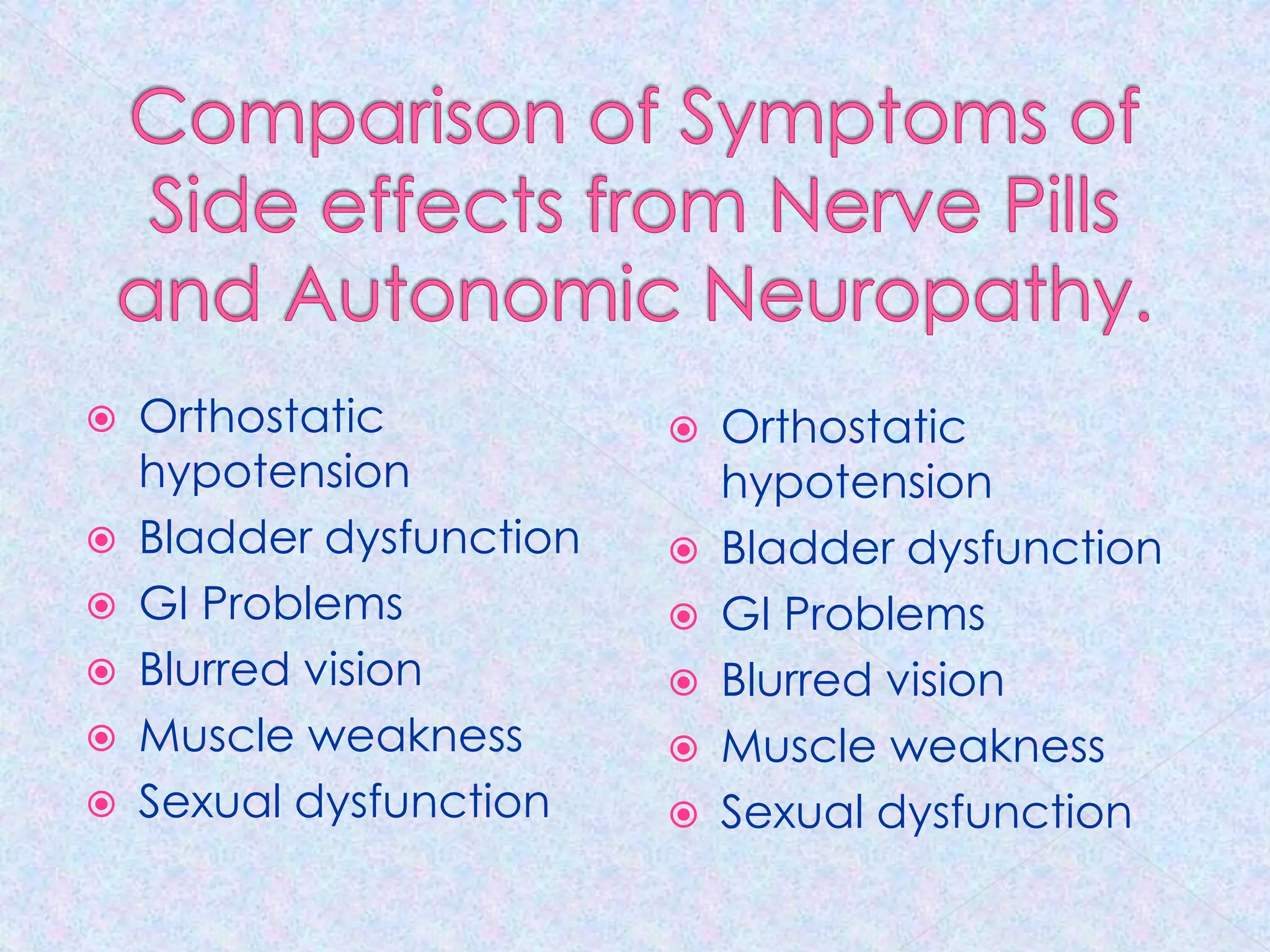
The document discusses various forms of neuropathy, particularly focusing on diabetic peripheral neuropathy and peripheral nerve compression syndrome, highlighting their symptoms, causes, and treatment methods. It emphasizes the complexity of nerve-related disorders and advocates for a change in perception towards treatment options, including surgical decompression as a viable method for relief. The author argues that timely intervention can prevent the progression of nerve damage and improve patient outcomes.