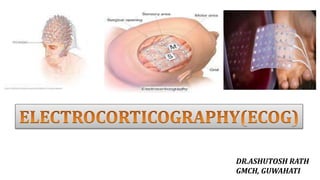
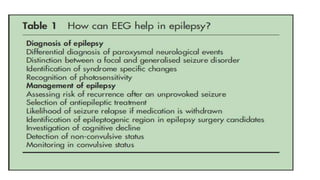
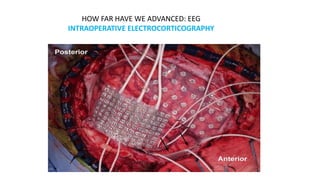
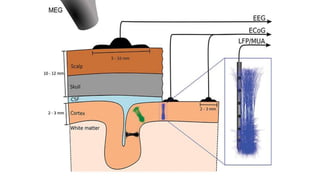
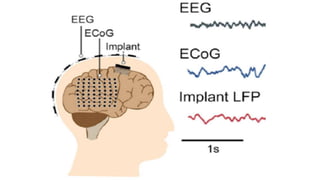
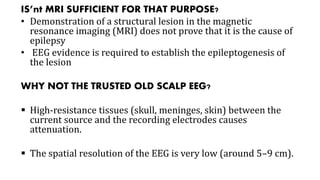
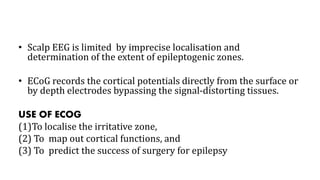
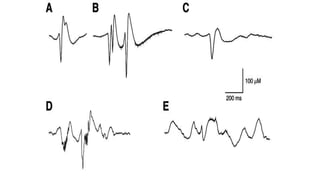
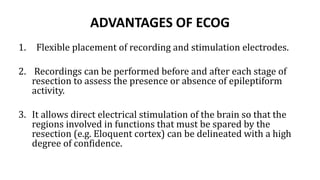
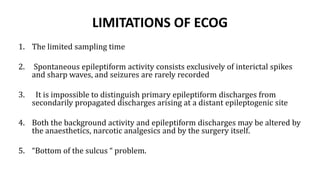
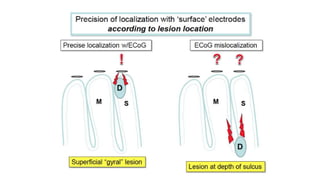
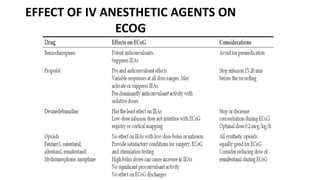
EEG has relatively low sensitivity (25–56%) for diagnosing epilepsy but high specificity (78–98%). Epileptiform discharges are seen in 0.5% of healthy adults on routine EEG but 10-30% in those with brain pathologies. Factors like the location of the epileptogenic zone, seizure frequency, and timing of the EEG affect whether a patient shows interictal epileptiform discharges. Intraoperative electrocorticography directly records cortical potentials during epilepsy surgery to localize the irritative zone, map brain functions, and predict surgical outcomes. It has higher spatial resolution than scalp EEG but recordings are limited by anesthesia effects and duration.