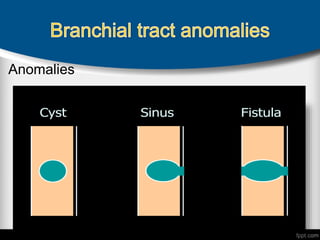
Branchial anomalies result from improper development of the branchial apparatus during embryogenesis. They present as cysts, sinuses, or fistulas in the neck region due to failure of branchial clefts or pouches to regress normally. The definitive treatment is complete surgical excision to prevent recurrent infections while protecting important nerves like the spinal accessory and recurrent laryngeal. Second branchial cleft cysts are the most common type and manifest as neck masses anterior to the sternocleidomastoid muscle.