Embed presentation

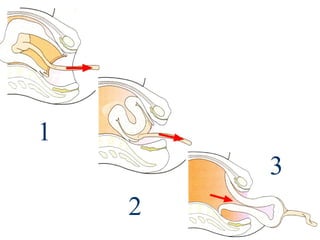
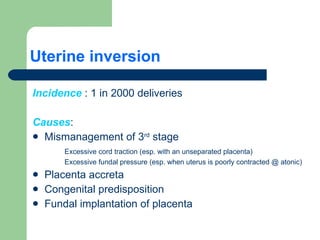
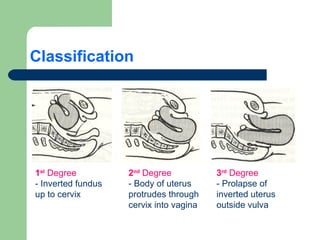
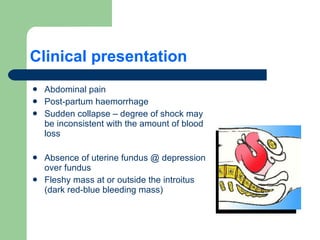
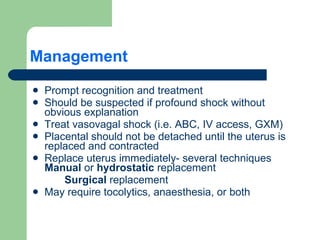

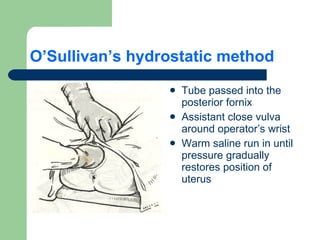
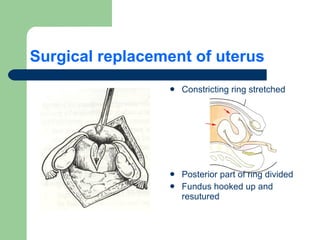
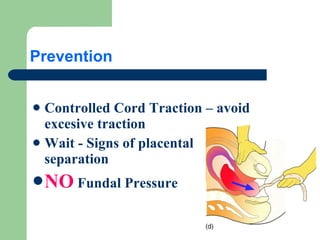
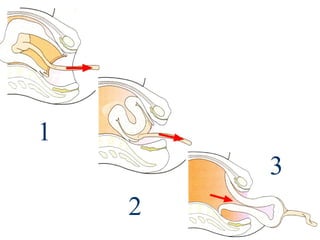
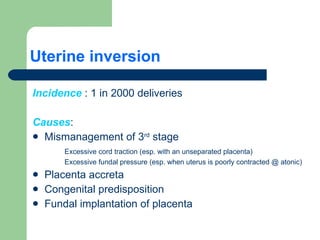
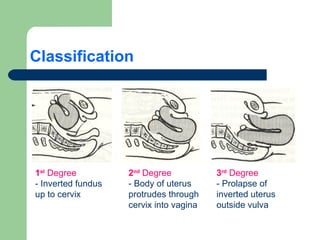
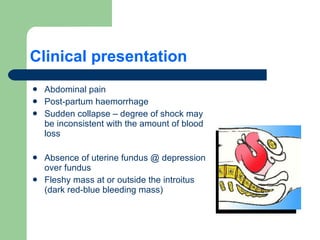
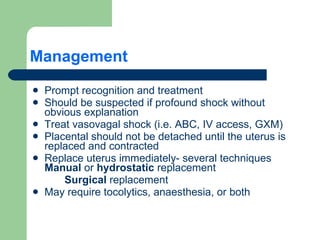
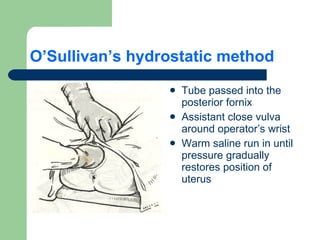
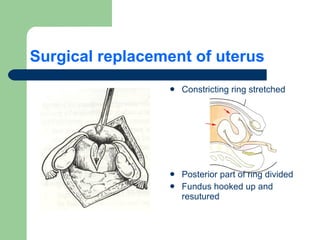
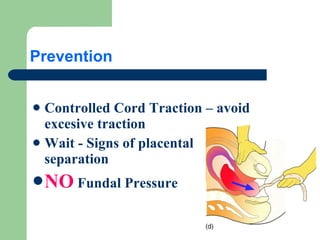
Uterine inversion occurs when the uterus turns inside out, most commonly during the third stage of labor. It has an incidence of 1 in 2000 deliveries. The main causes are mismanagement of the third stage through excessive cord traction or fundal pressure. Uterine inversion can be first, second, or third degree depending on how far the inversion has progressed. Clinical presentation includes abdominal pain, postpartum hemorrhage, and shock. Management involves prompt recognition and replacement of the inverted uterus manually or through hydrostatic replacement, with tocolytics as needed. Prevention focuses on controlled cord traction and avoiding fundal pressure before signs of placental separation.