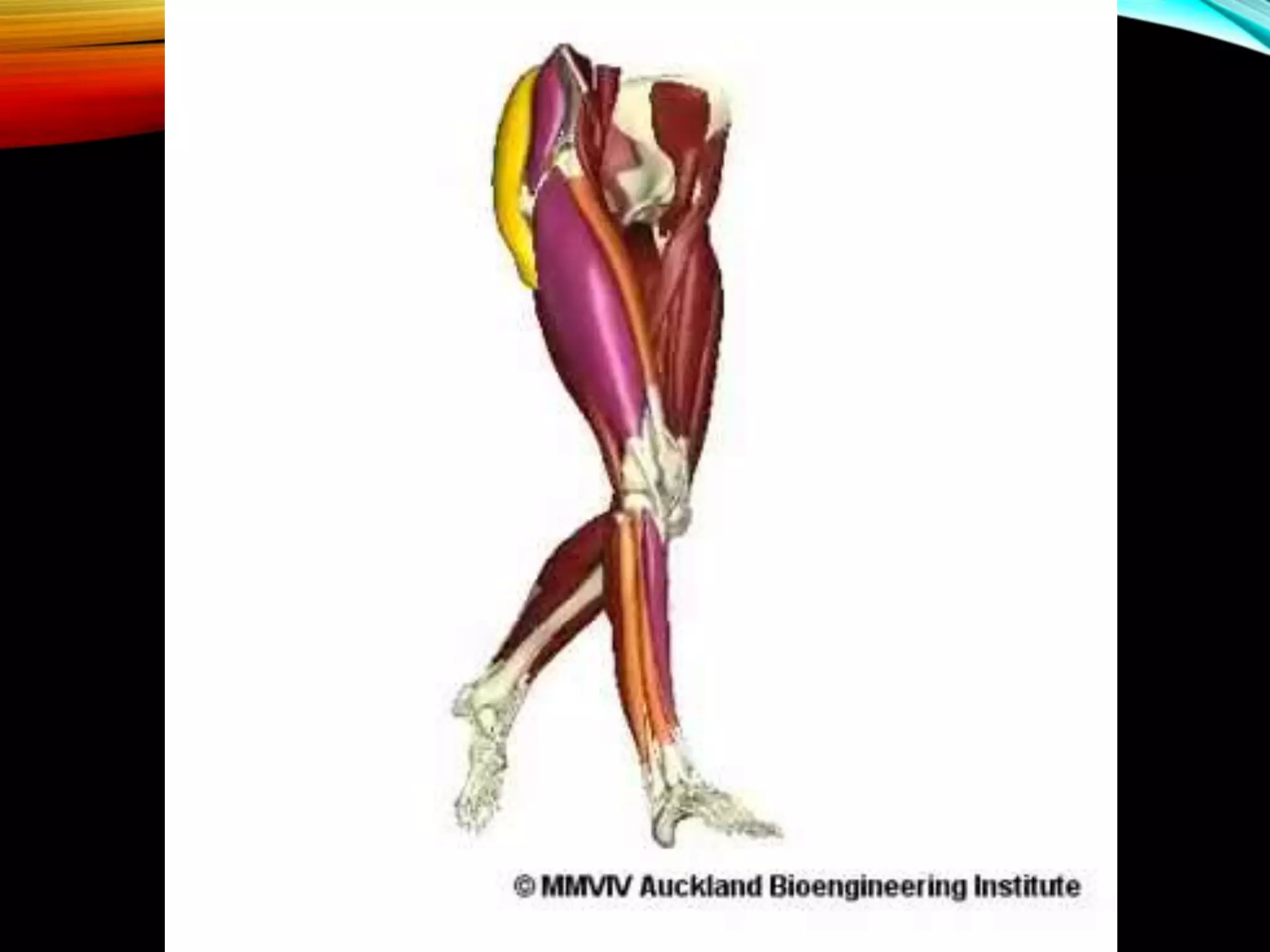
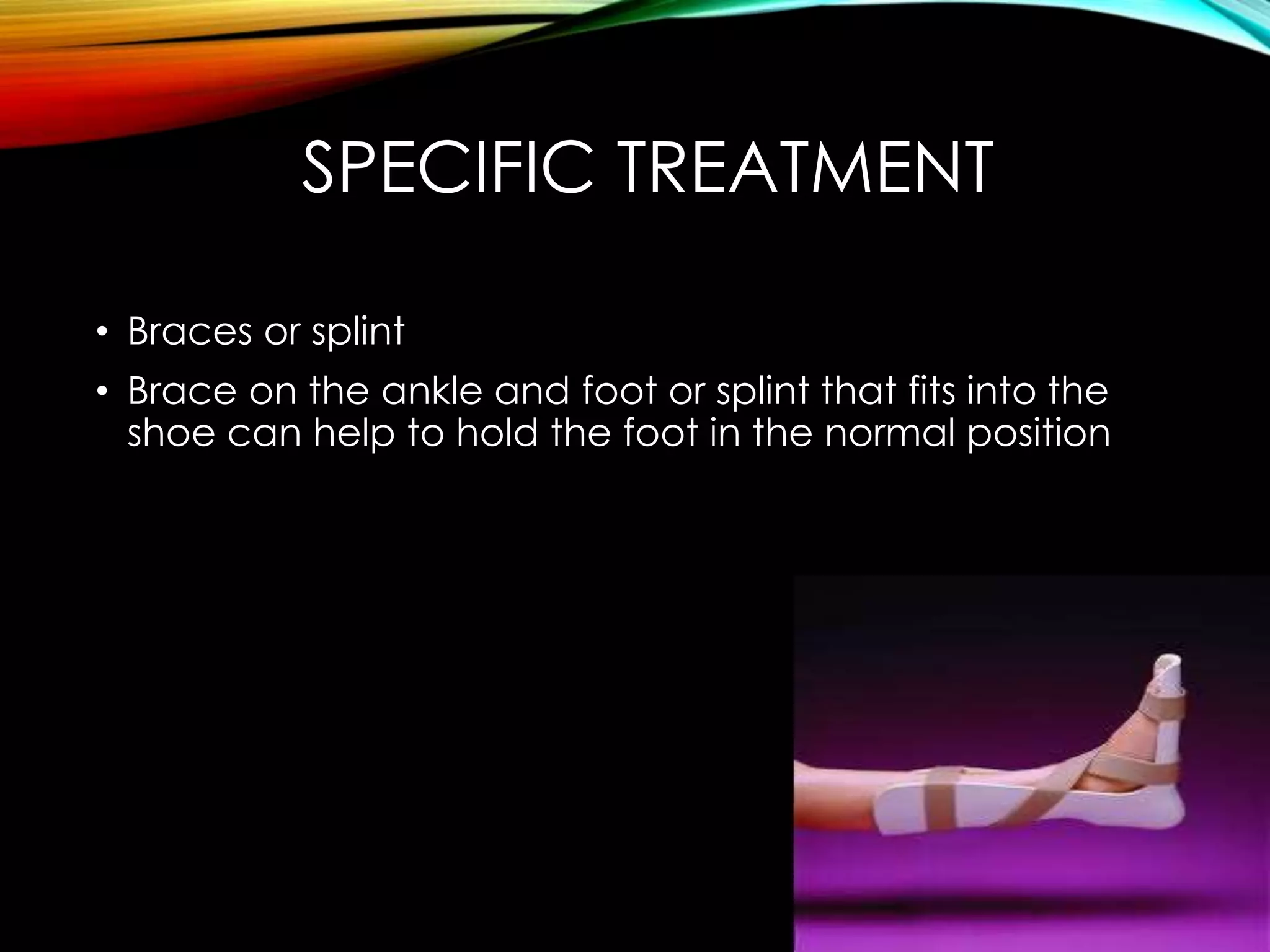
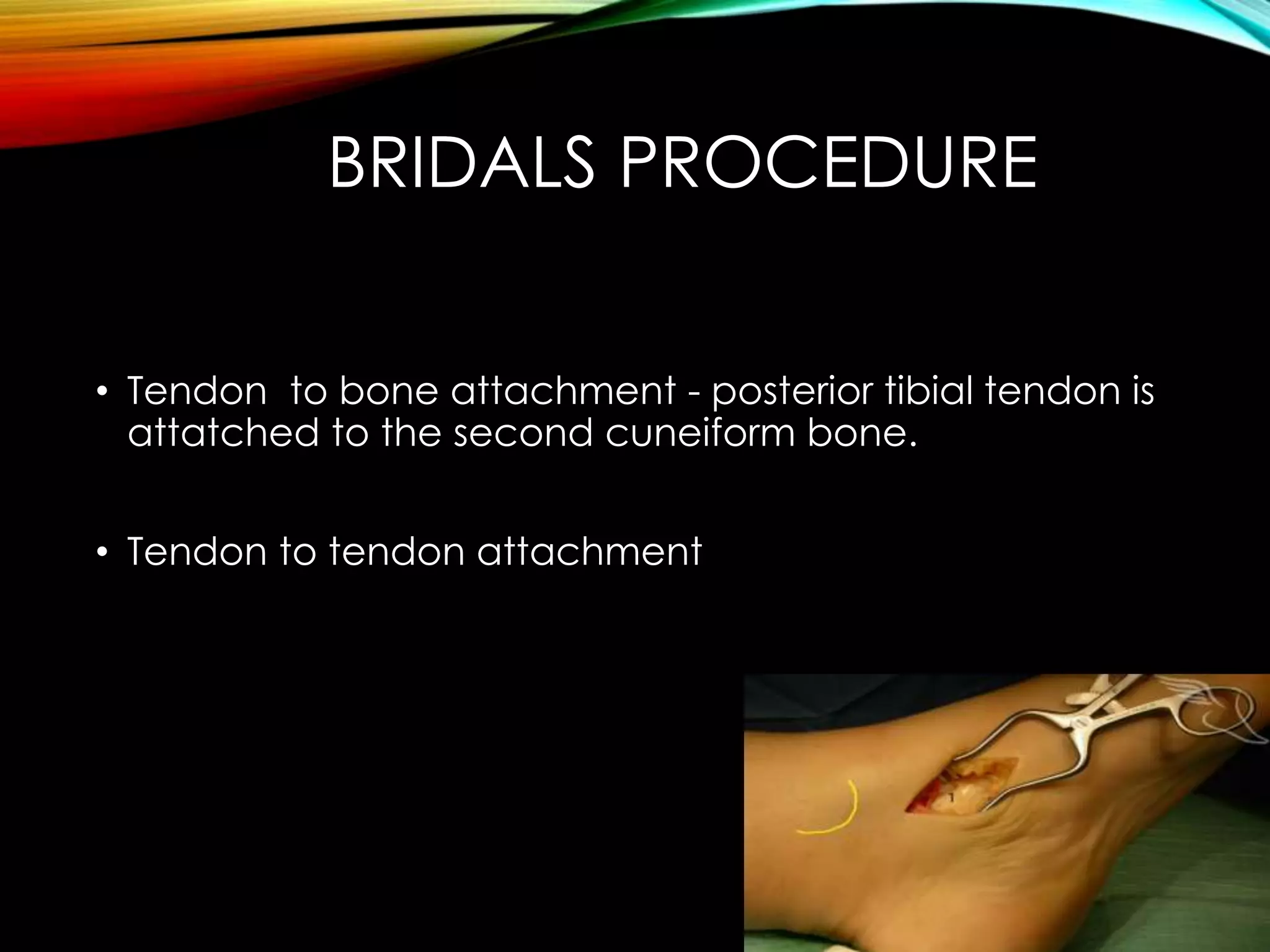
This document discusses foot drop, which is the inability to lift the front part of the foot. It can be caused by nerve injuries, neurological conditions, muscle weakness, or injuries. Symptoms include difficulty lifting the foot and dragging it when walking. Treatment depends on the underlying cause but may include bracing, physical therapy, nerve stimulation, or surgery to repair nerves or transfer tendons.