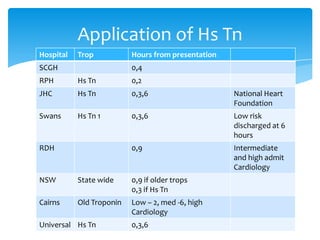
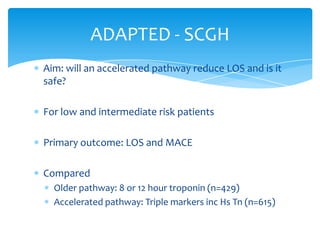
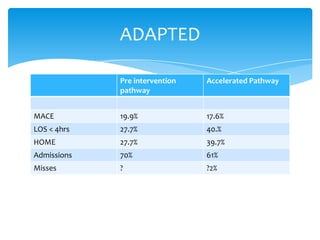
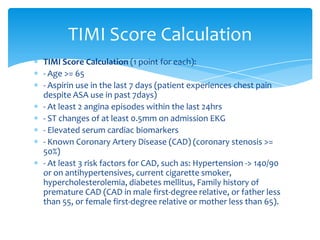
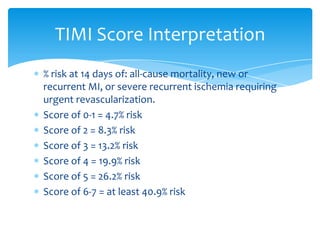
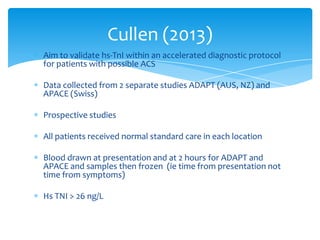
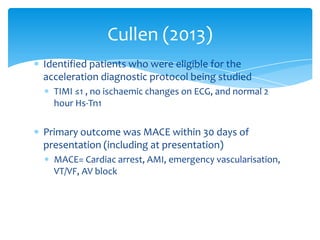
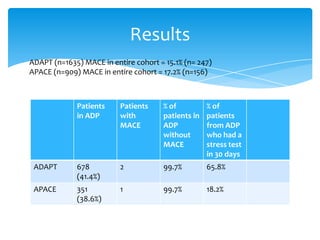
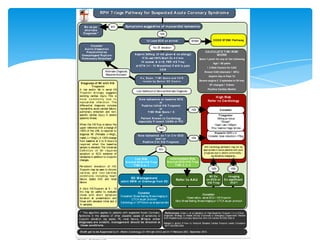
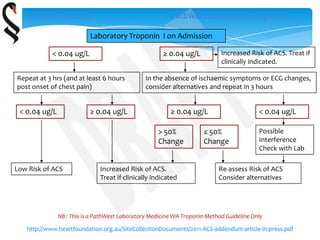
Ultra high sensitivity troponins can detect troponin in healthy individuals and allow for earlier diagnosis of myocardial infarction. However, they have reduced specificity and may lead to overdiagnosis. Using troponins along with risk stratification tools like the TIMI score and serial measurements can help manage this. Studies show accelerated diagnostic pathways using high sensitivity troponins and risk scores safely reduce length of stays and admissions for approximately 40% of low-risk suspected acute coronary syndrome patients. Ongoing issues include safely managing intermediate-risk patients and addressing reduced specificity.