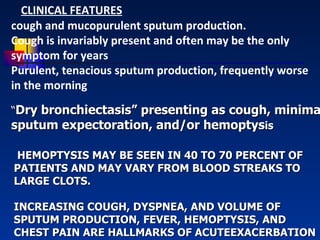
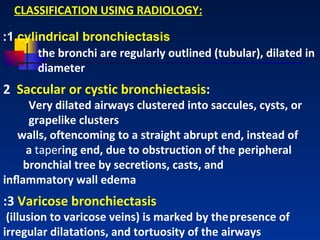
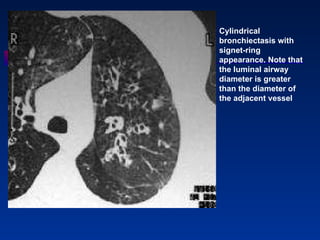
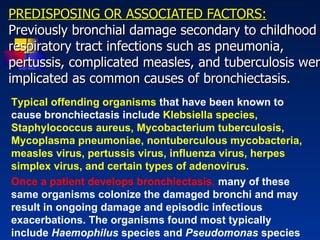
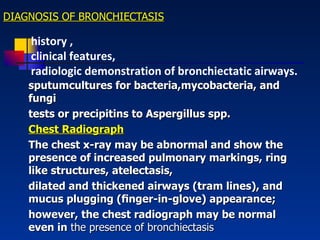
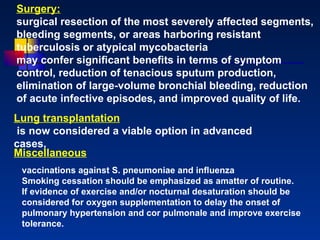
Bronchiectasis is a lung condition characterized by abnormal dilation of the bronchi. It is usually caused by damage to the airways from childhood infections. Symptoms include chronic cough and mucus production. Diagnosis involves chest imaging like CT scans to view the dilated airways. Treatment focuses on controlling infections with antibiotics, reducing inflammation, and improving lung cleansing through airway clearance techniques. In more severe cases, surgery may be used to remove diseased portions of the lung.