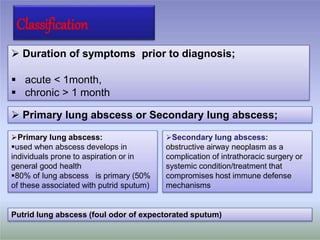
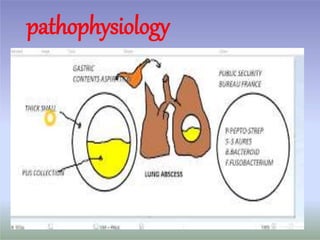
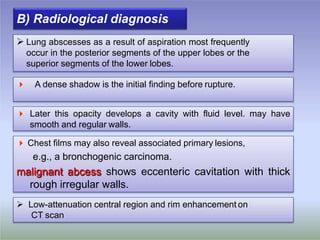
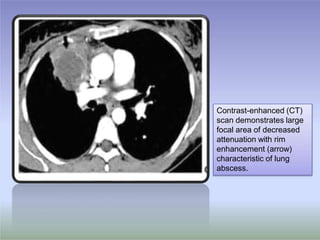
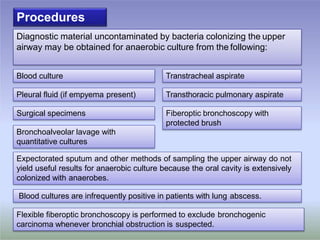
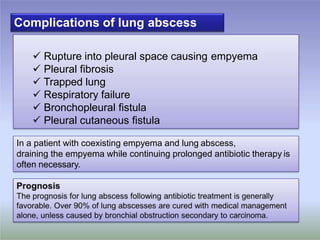
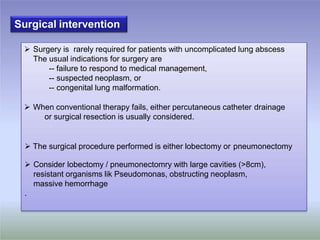
The document discusses lung abscess, including its definition, classification, microbiology, risk factors, pathophysiology, clinical features, diagnosis and treatment. A lung abscess is a microbial infection that causes necrosis of lung tissue, forming a cavity. It is usually caused by aspiration of oral anaerobic bacteria. Symptoms include cough, sputum production and fever. Diagnosis involves imaging showing a cavity with an air-fluid level. Treatment involves long-term antibiotics targeting the causative bacteria. Surgery is rarely needed except for failure of medical management or an underlying condition.