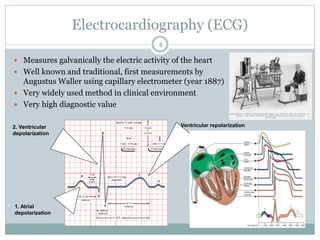
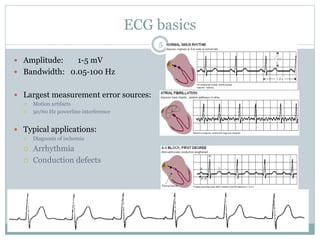
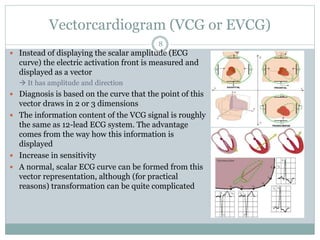
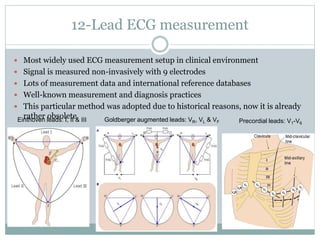
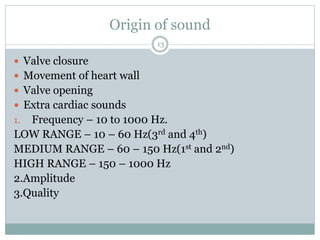
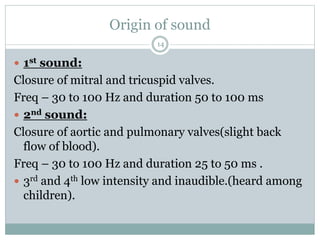
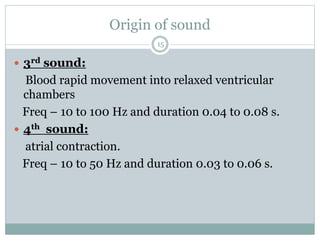
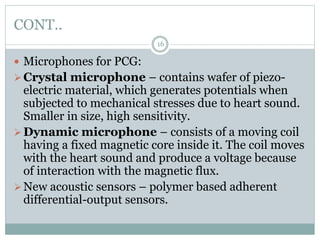
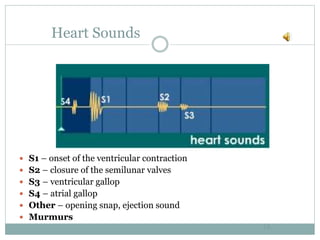
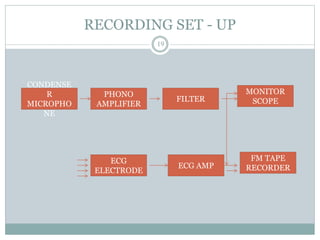
This document discusses various biomedical recorders used to measure electrical signals from the body. It focuses on electrocardiography (ECG) which measures the heart's electrical activity, and phonocardiography (PCG) which records heart sounds. For ECG, it describes the typical waveform, applications in diagnosis, and 12-lead measurement setup. For PCG, it explains the different heart sounds recorded, microphones used, writing methods, medical applications in detecting murmurs and valvular lesions, and special applications including fetal and esophageal PCG.