This document provides an overview of common gynecological surgical procedures and includes the following key points:
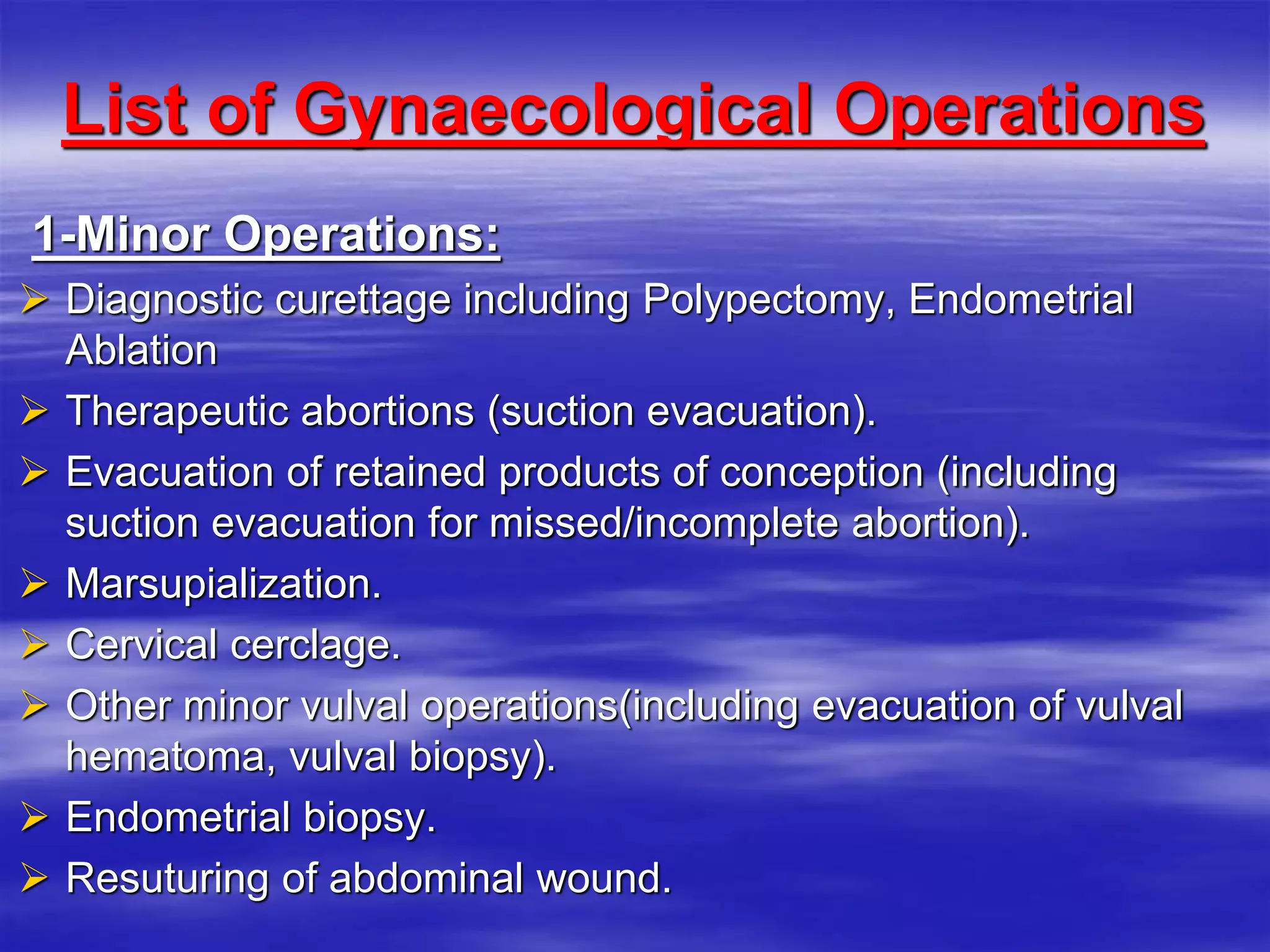
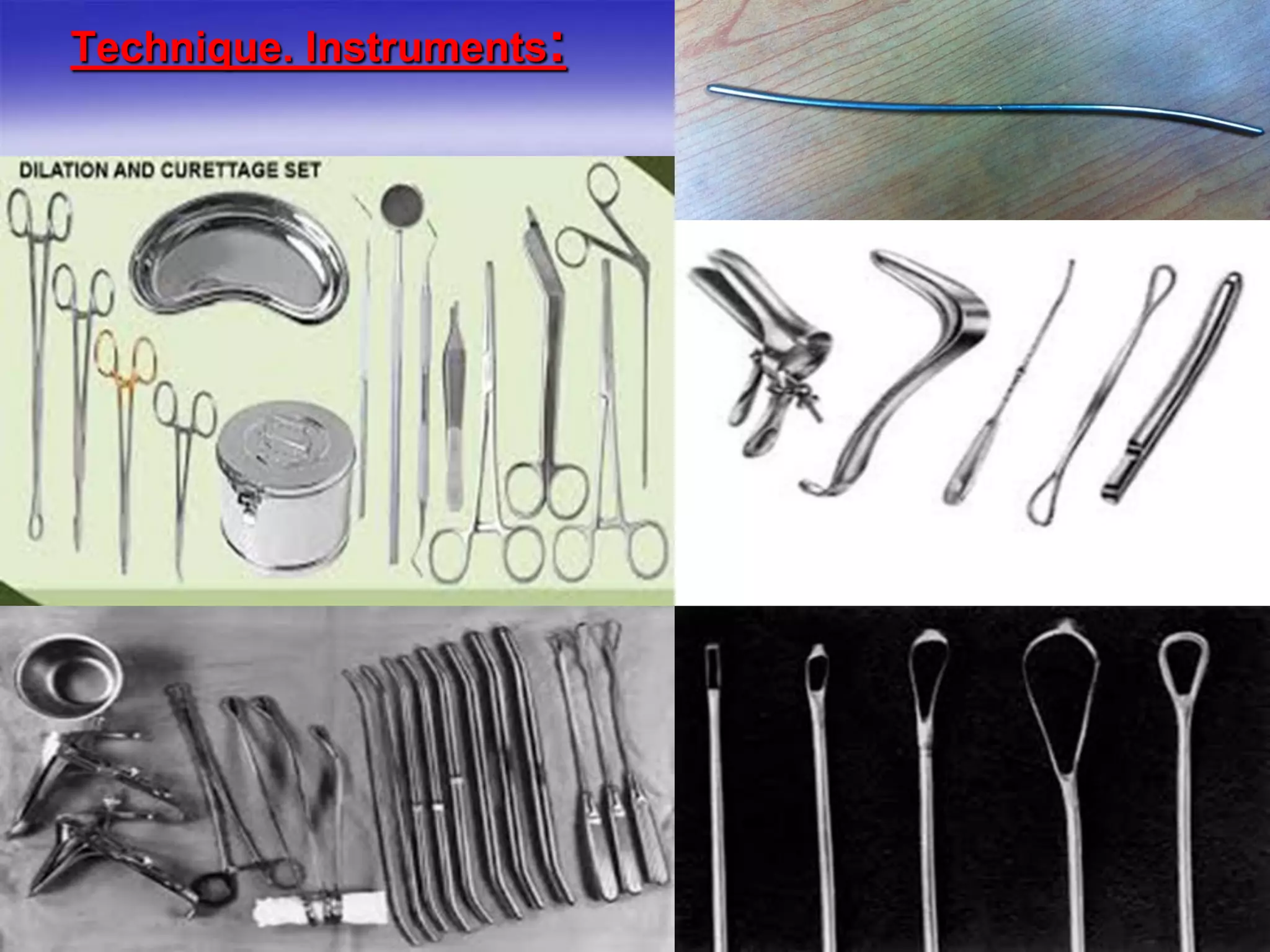
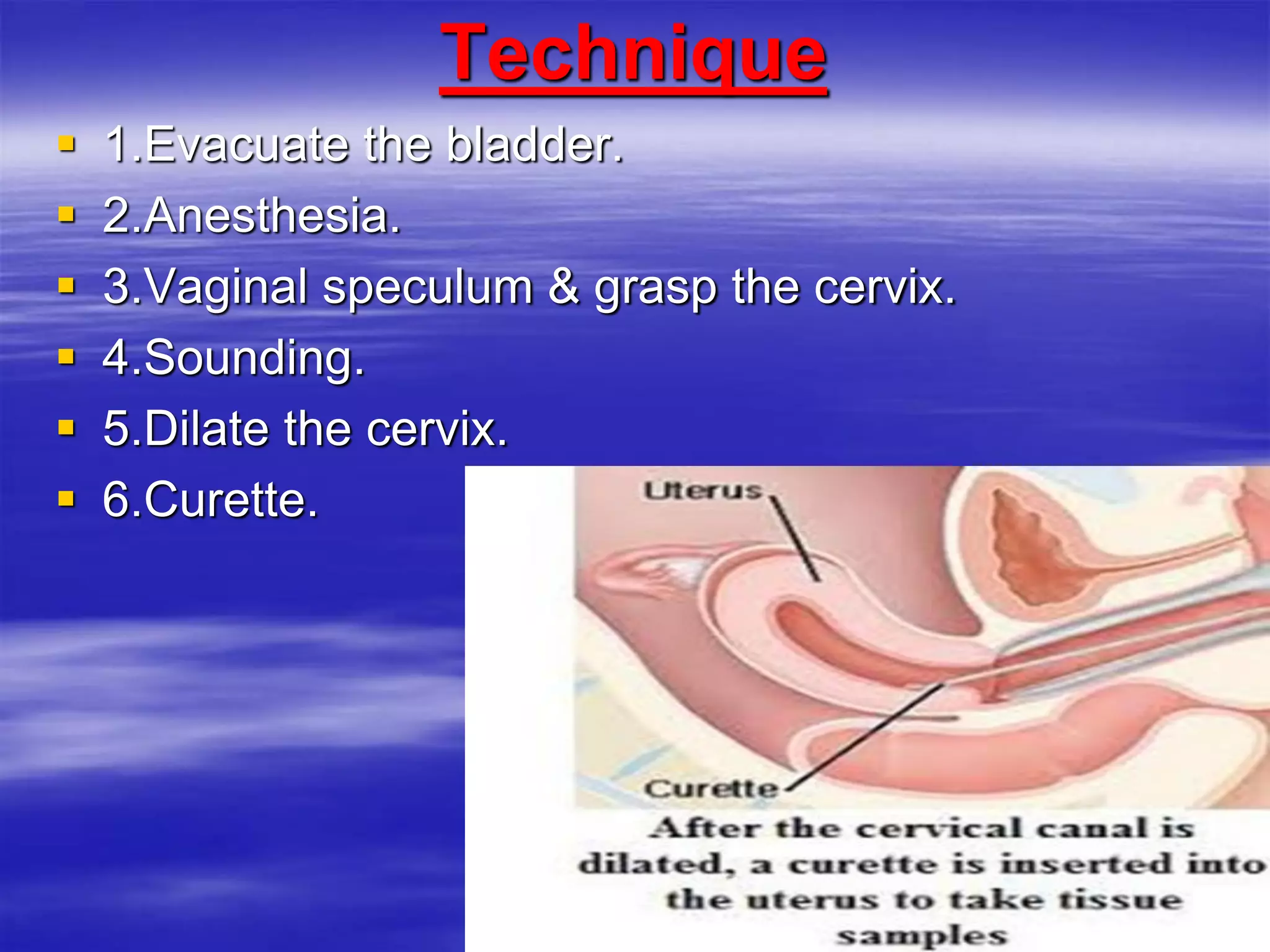
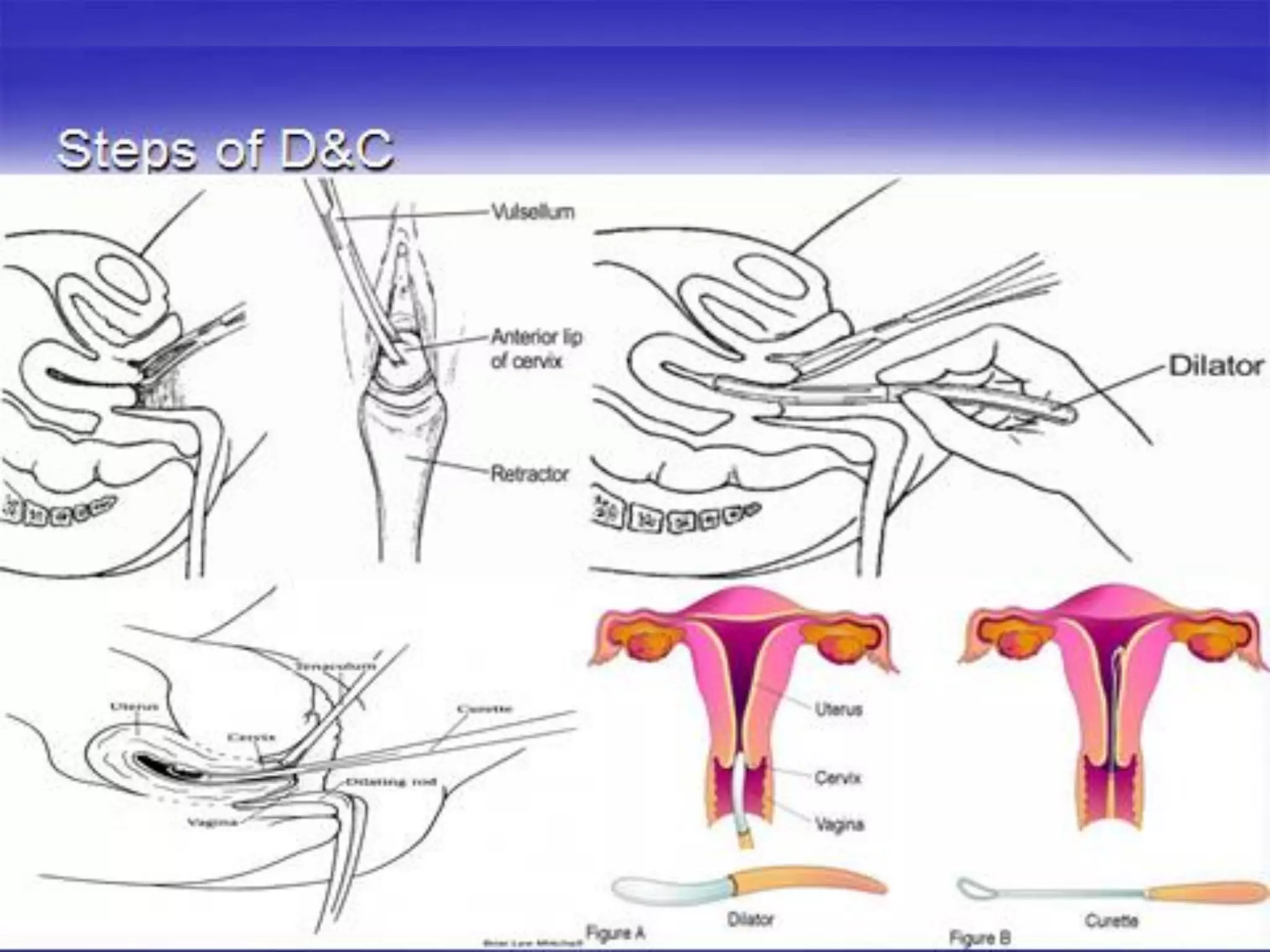
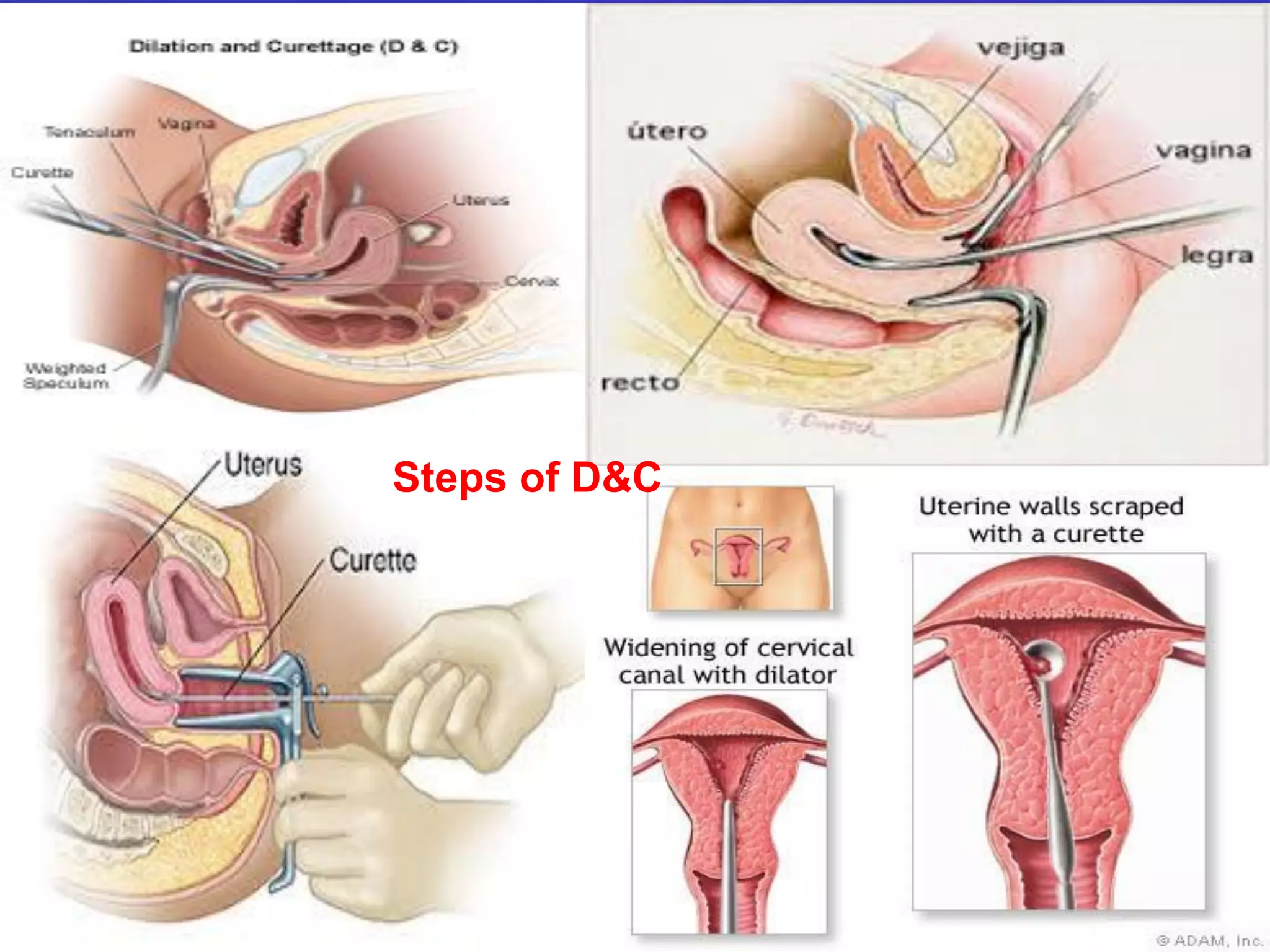
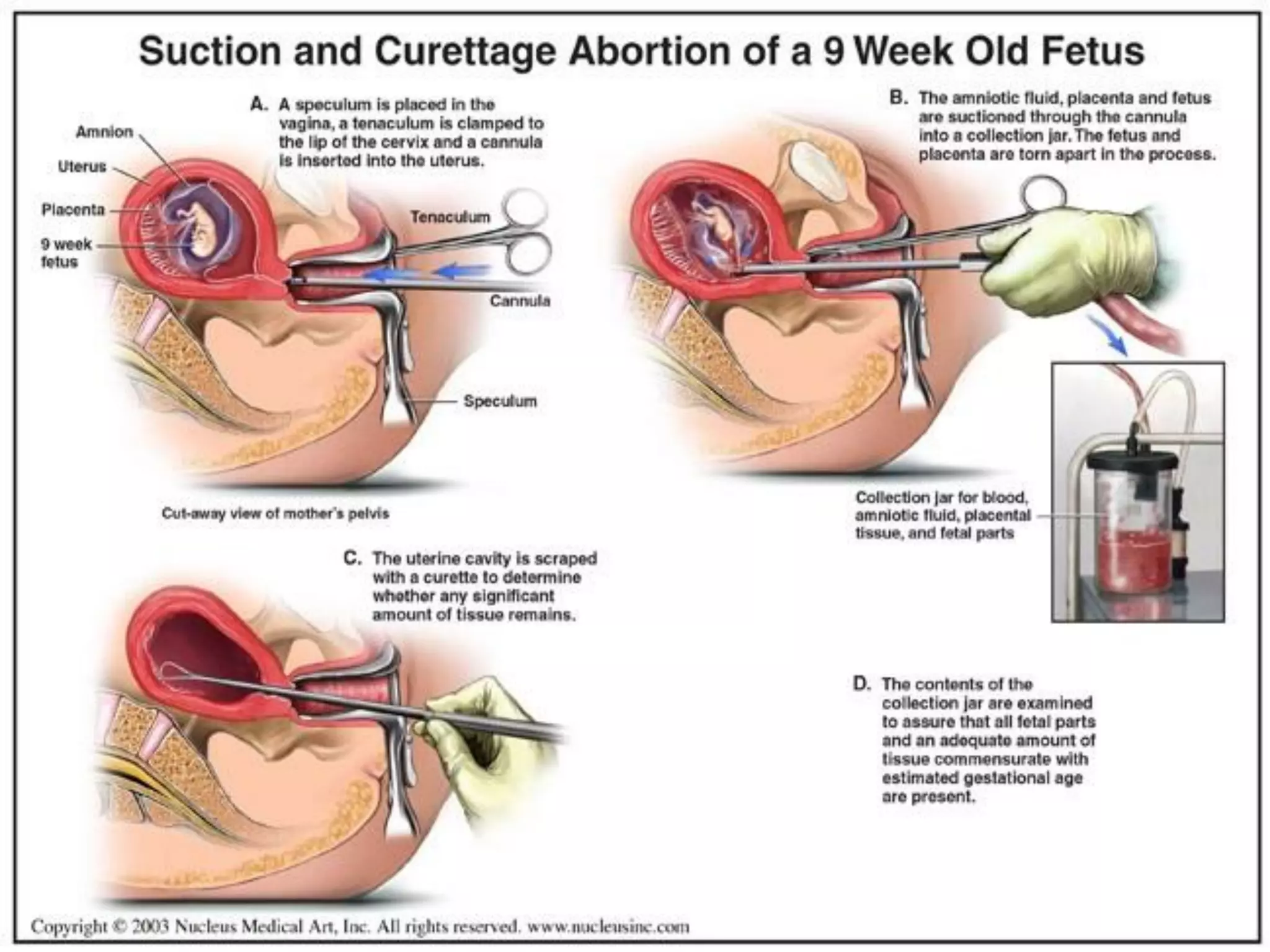
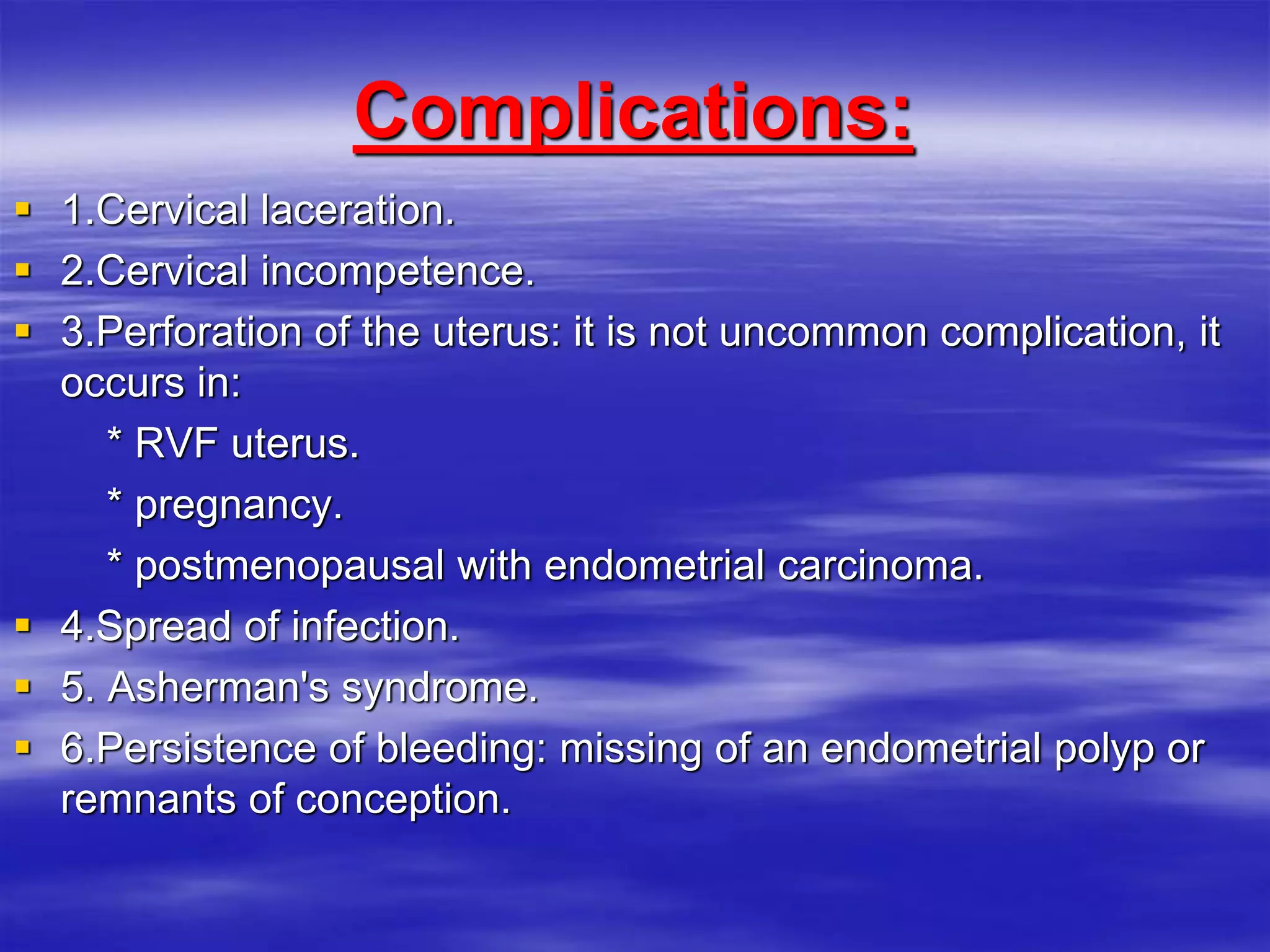
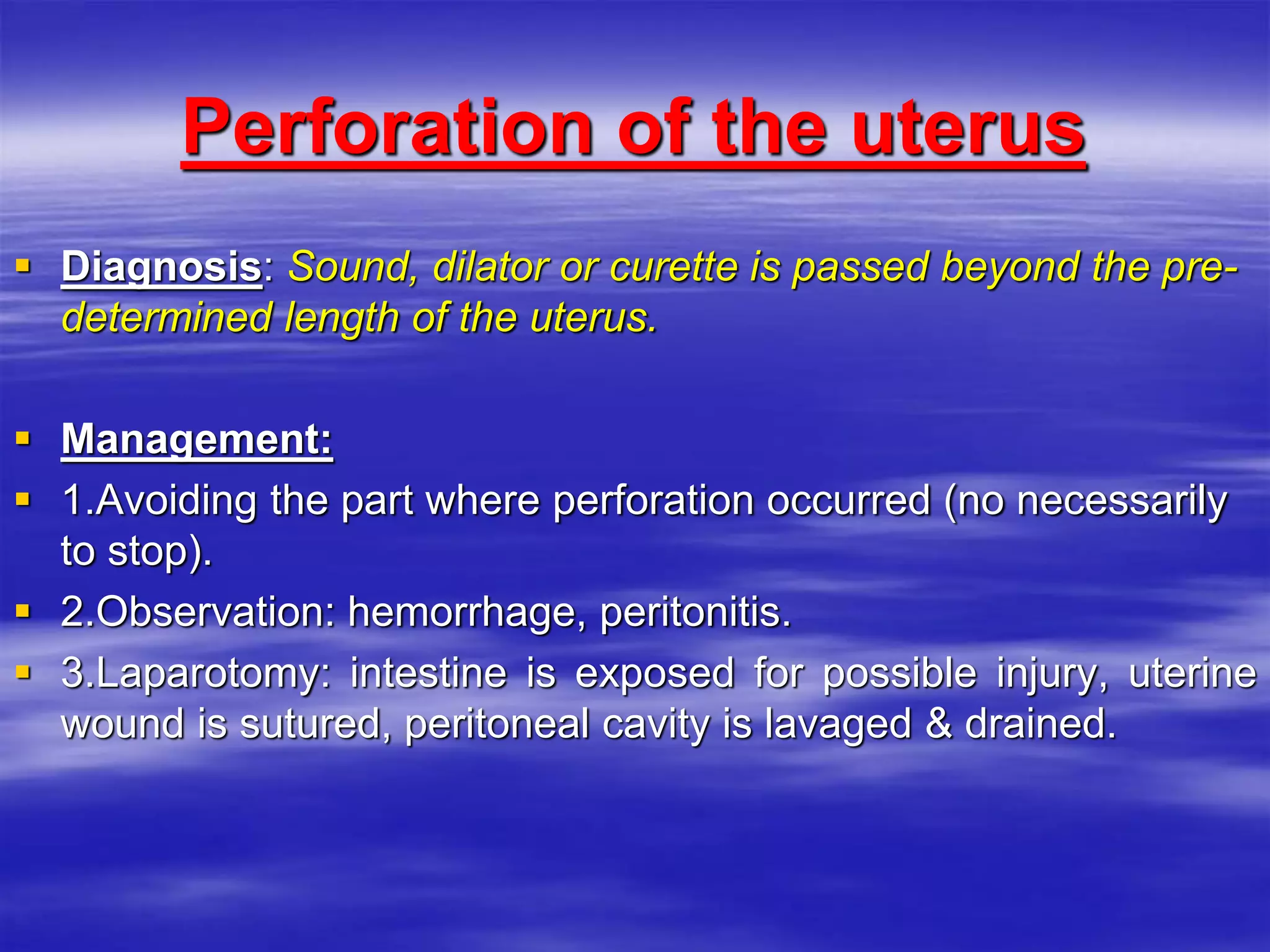
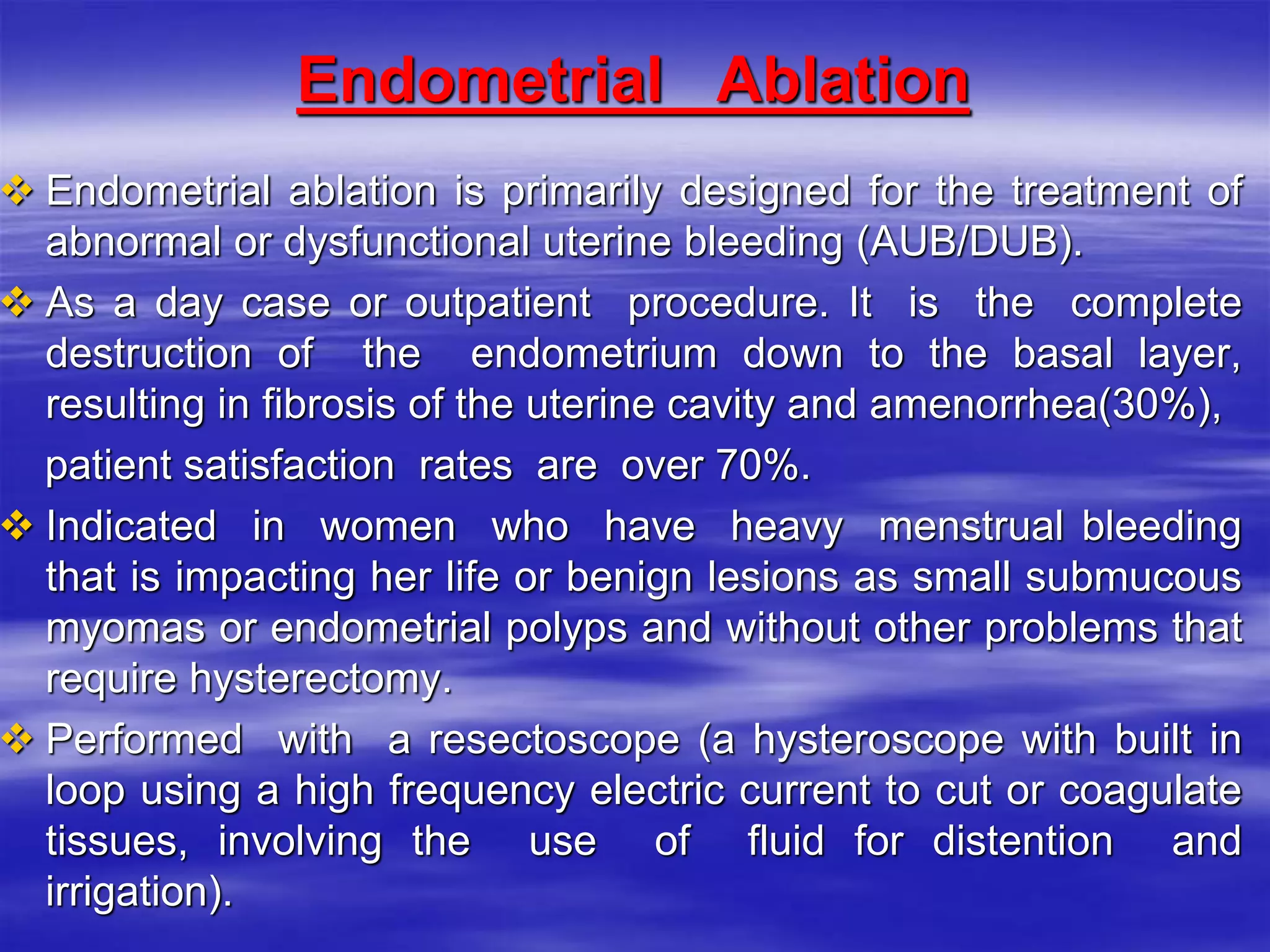
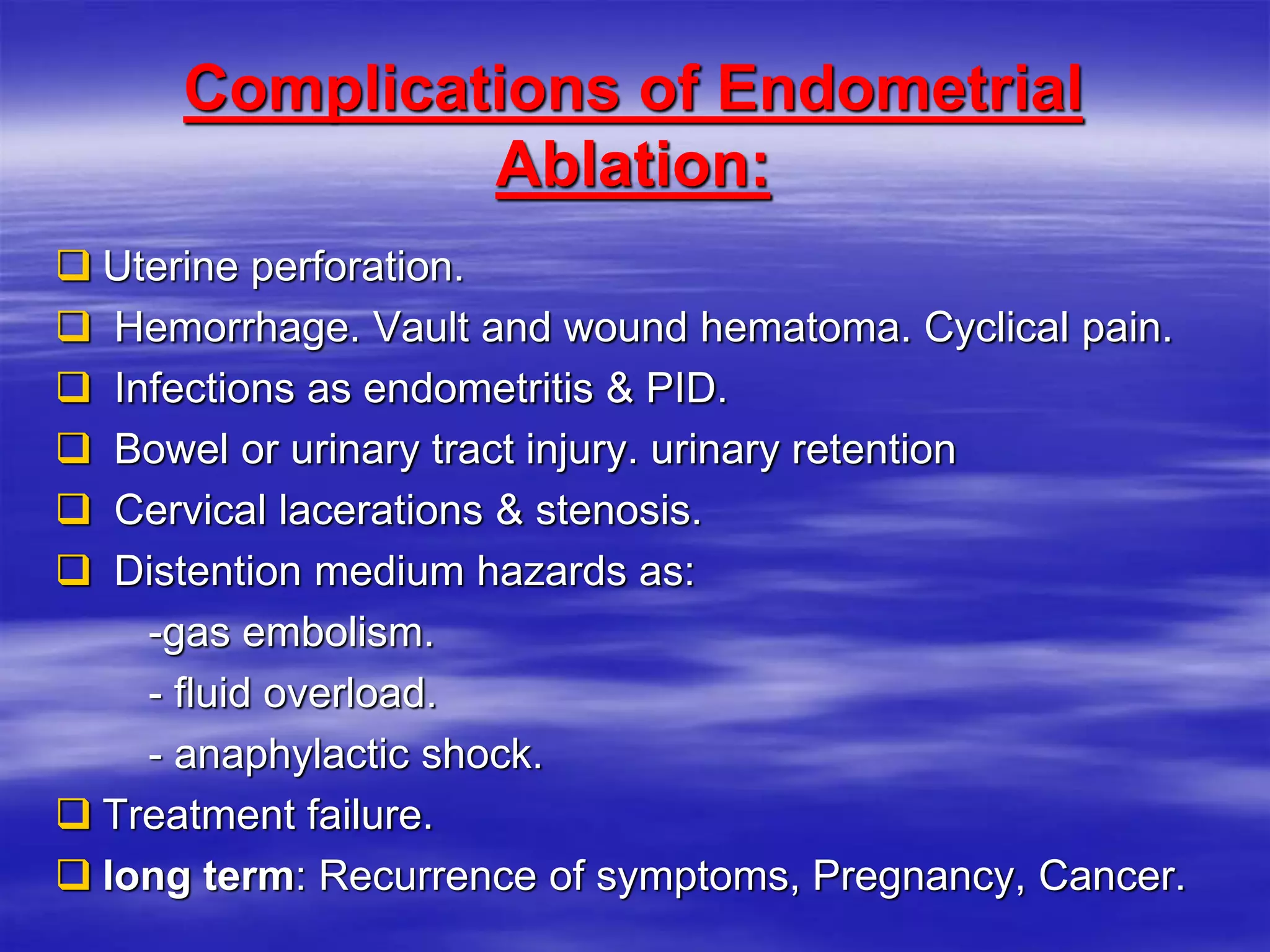
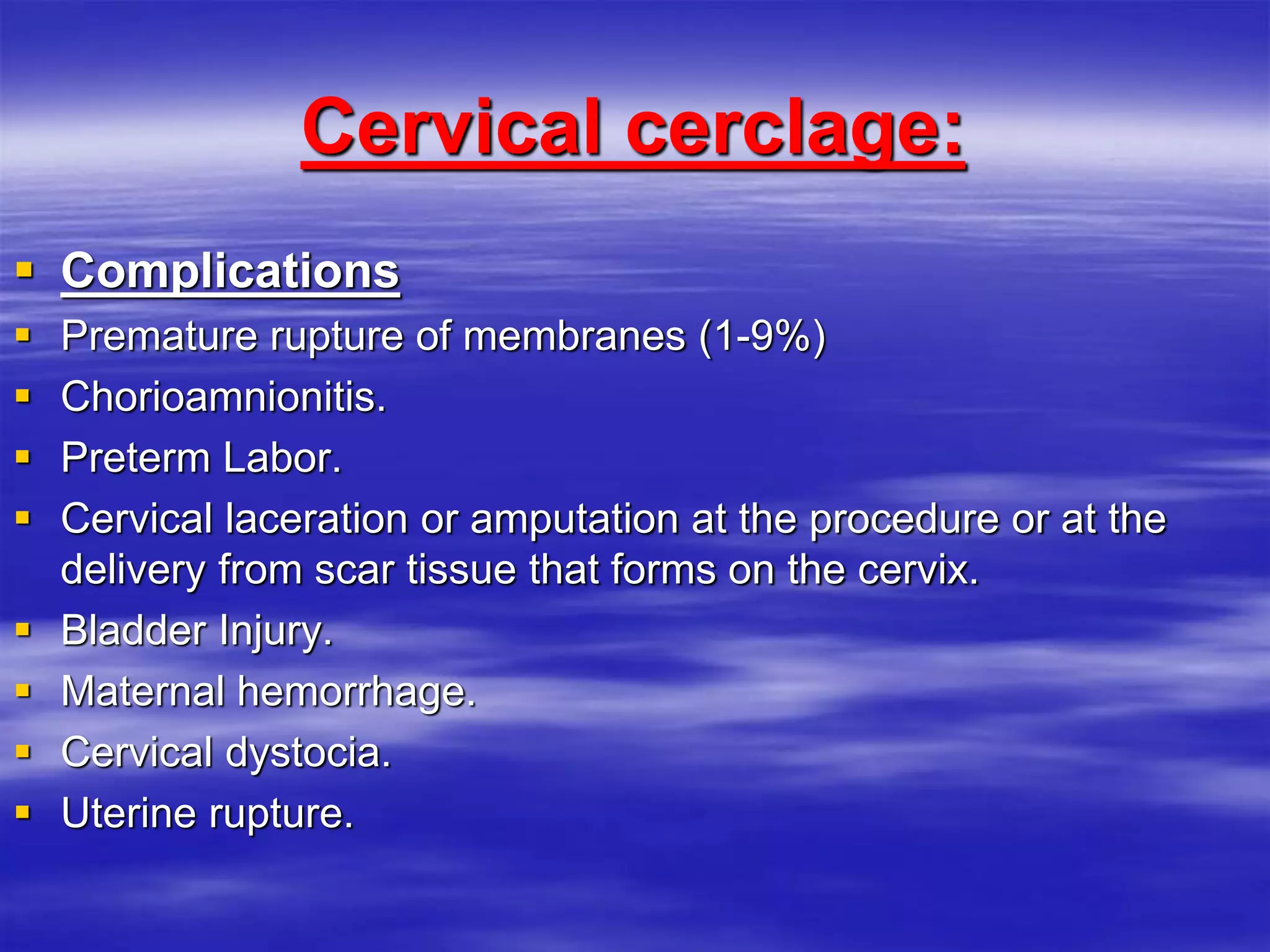
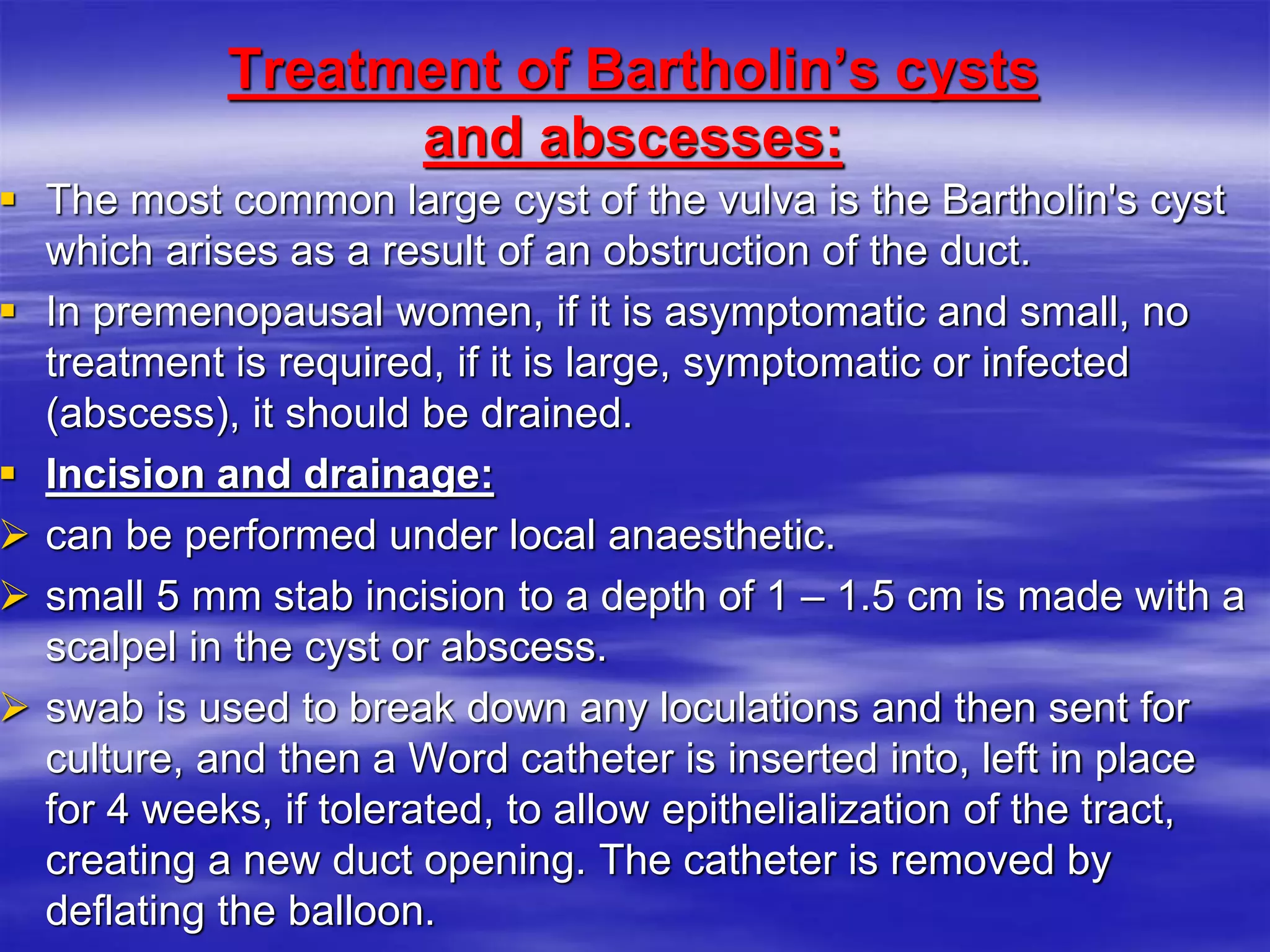
1. It describes procedures like dilation and curettage (D&C), endometrial ablation, and cervical cerclage - outlining their indications, techniques, and potential complications.
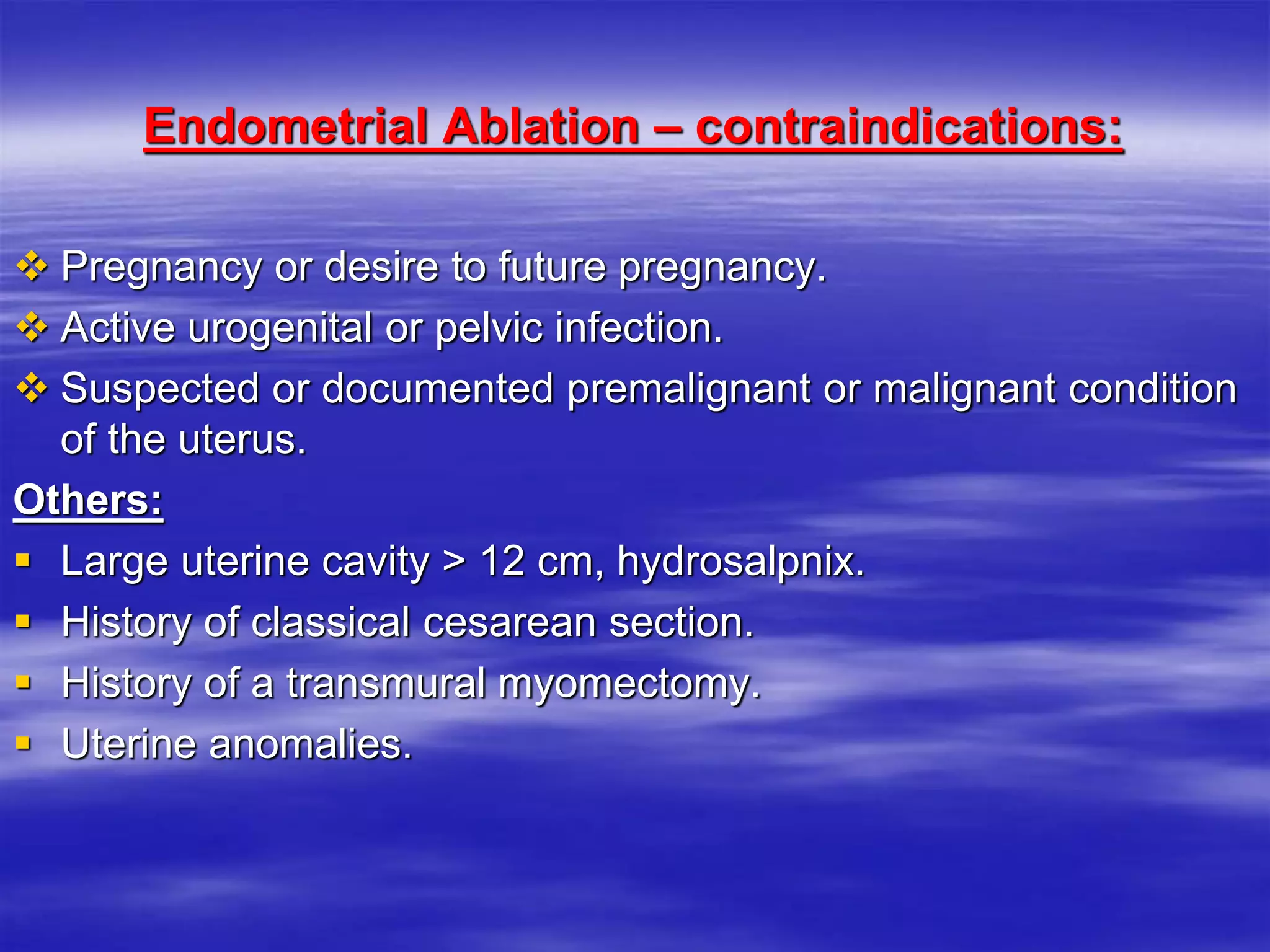
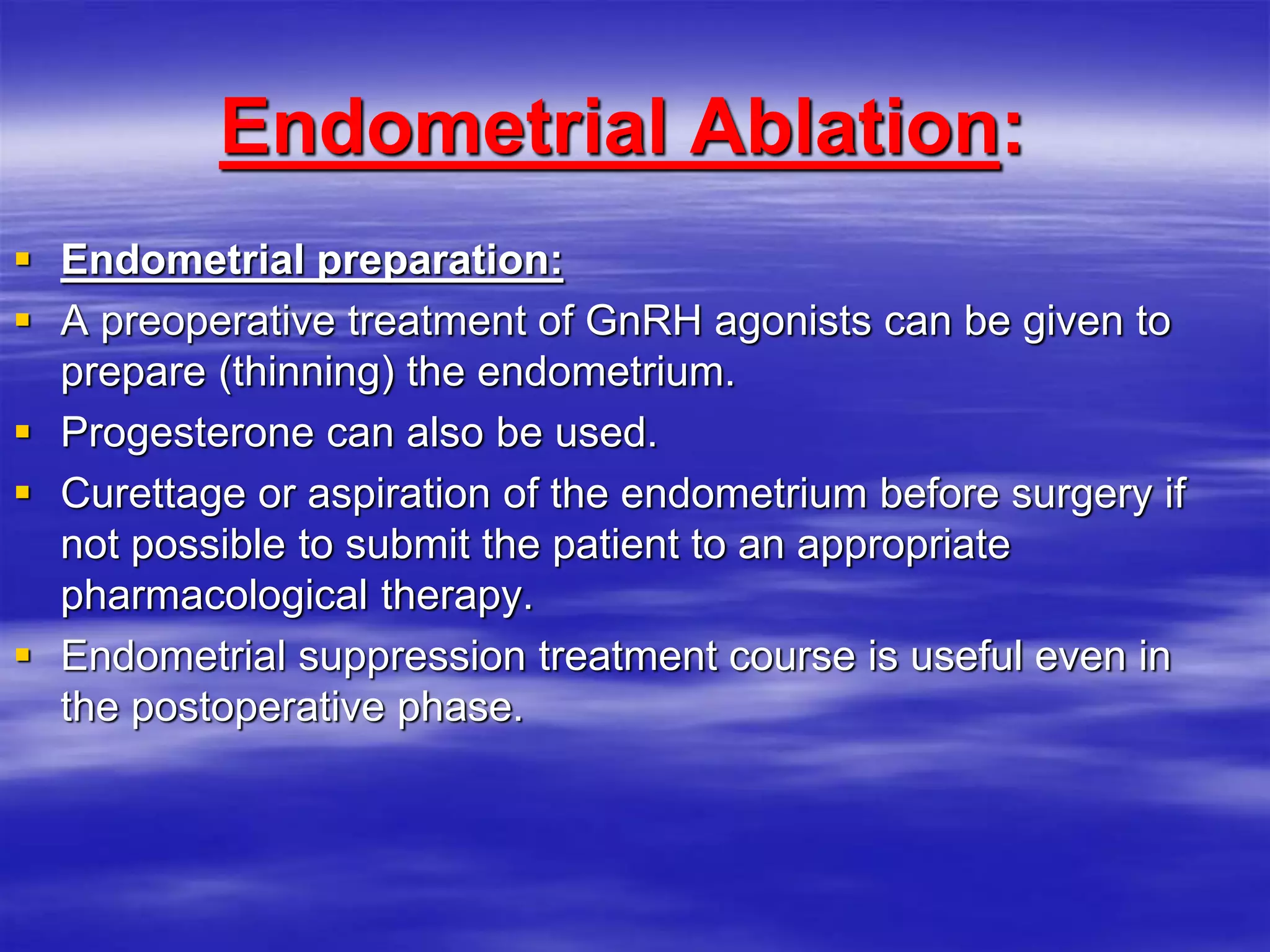
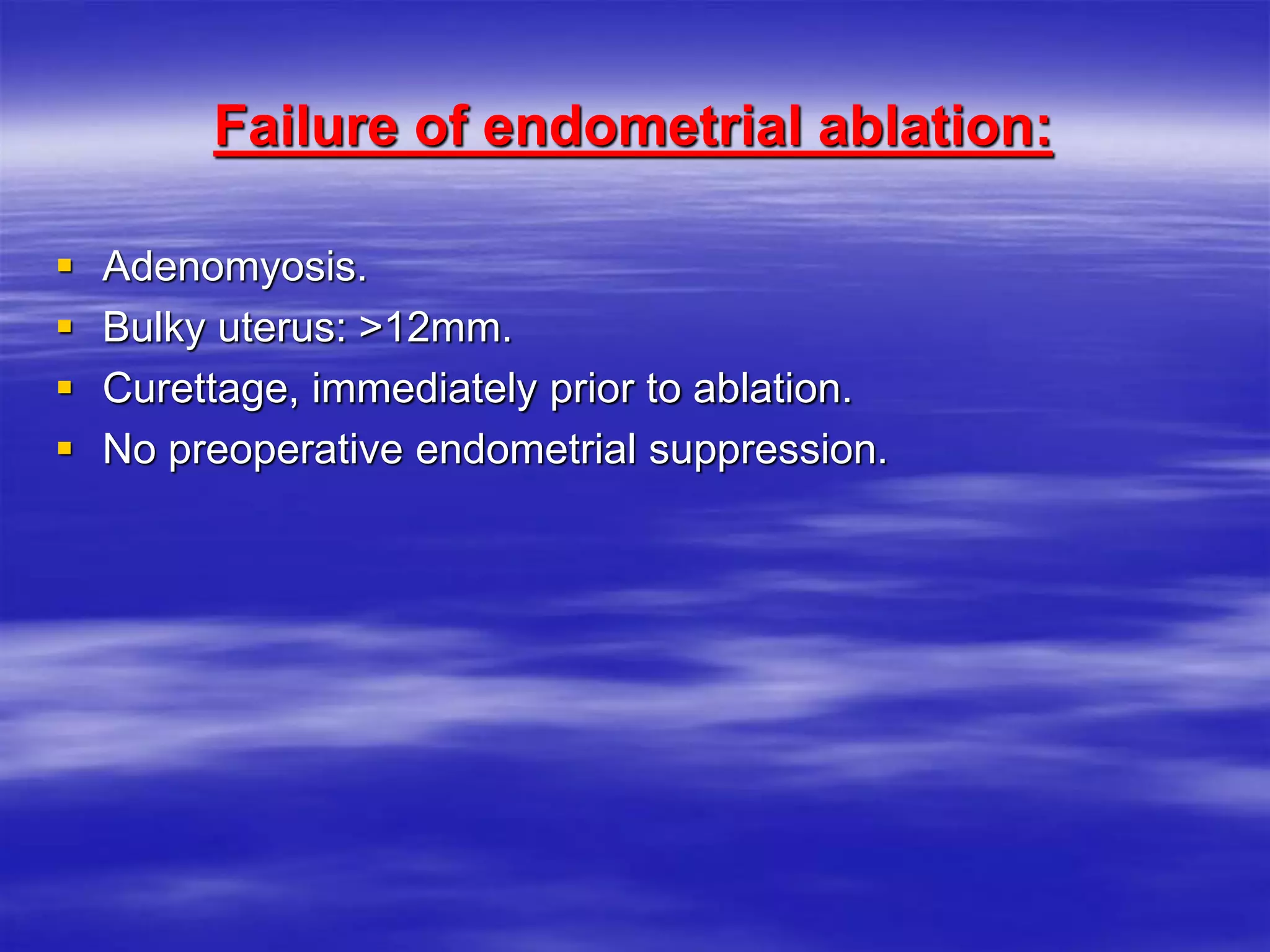
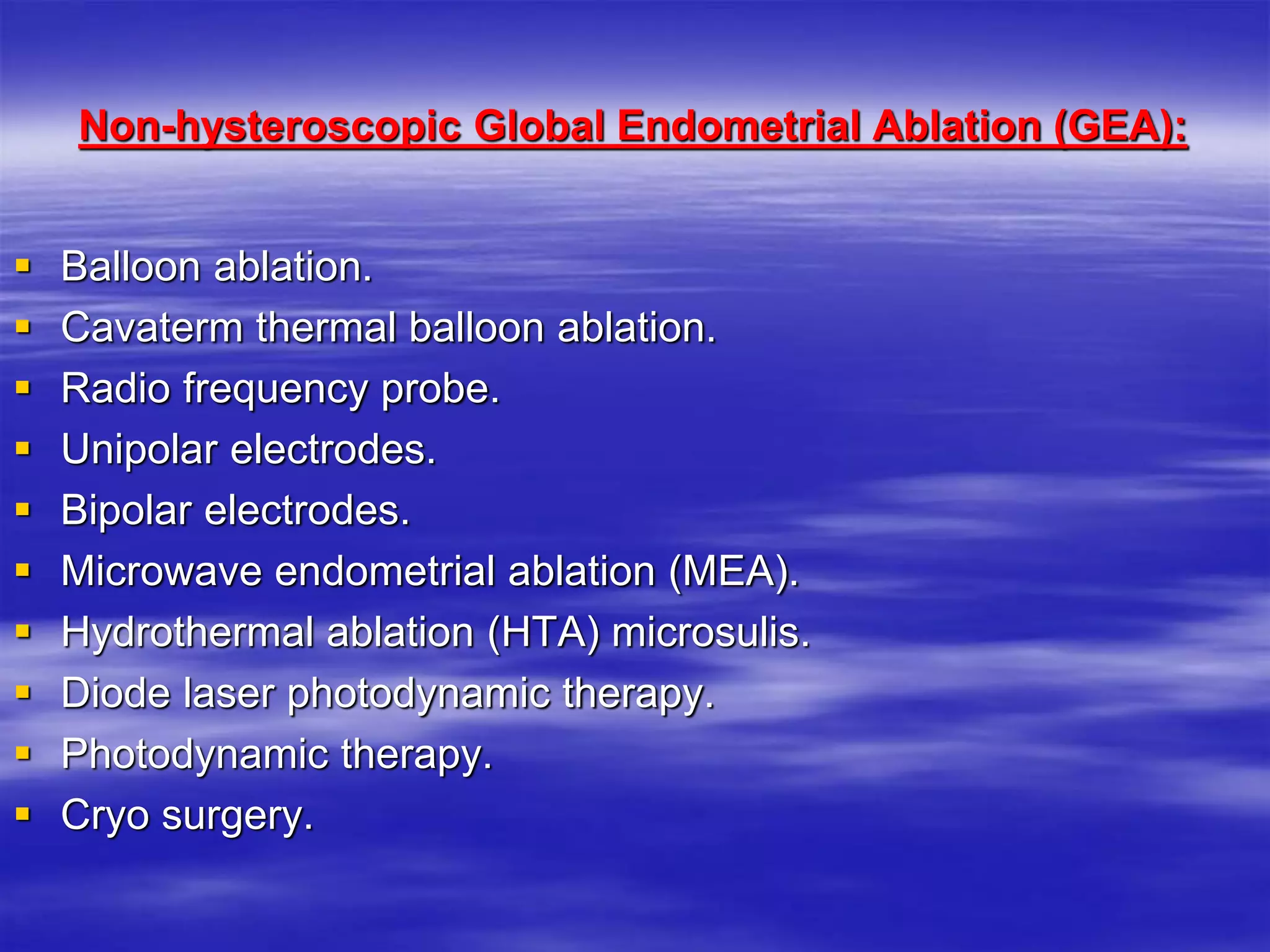
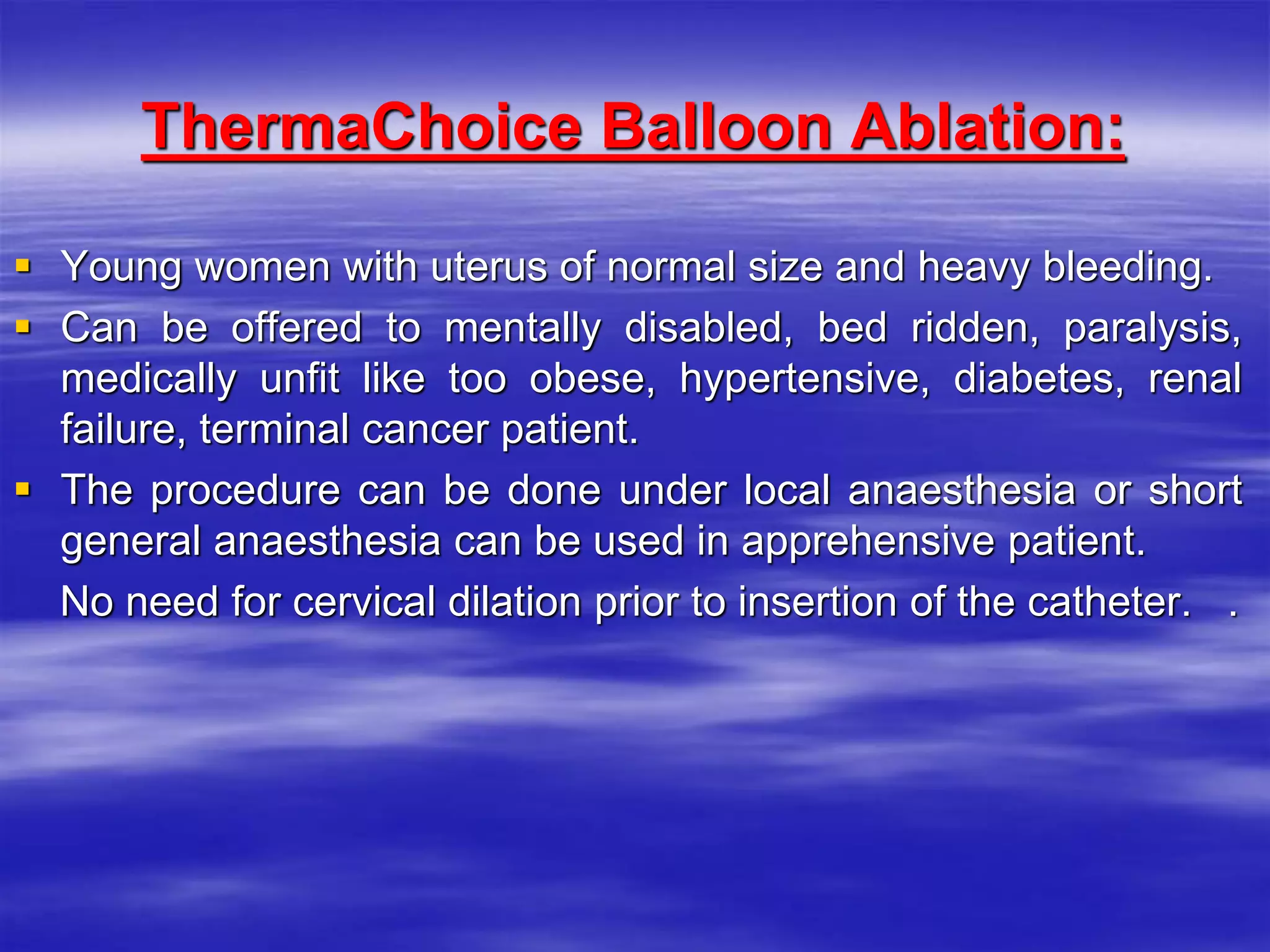
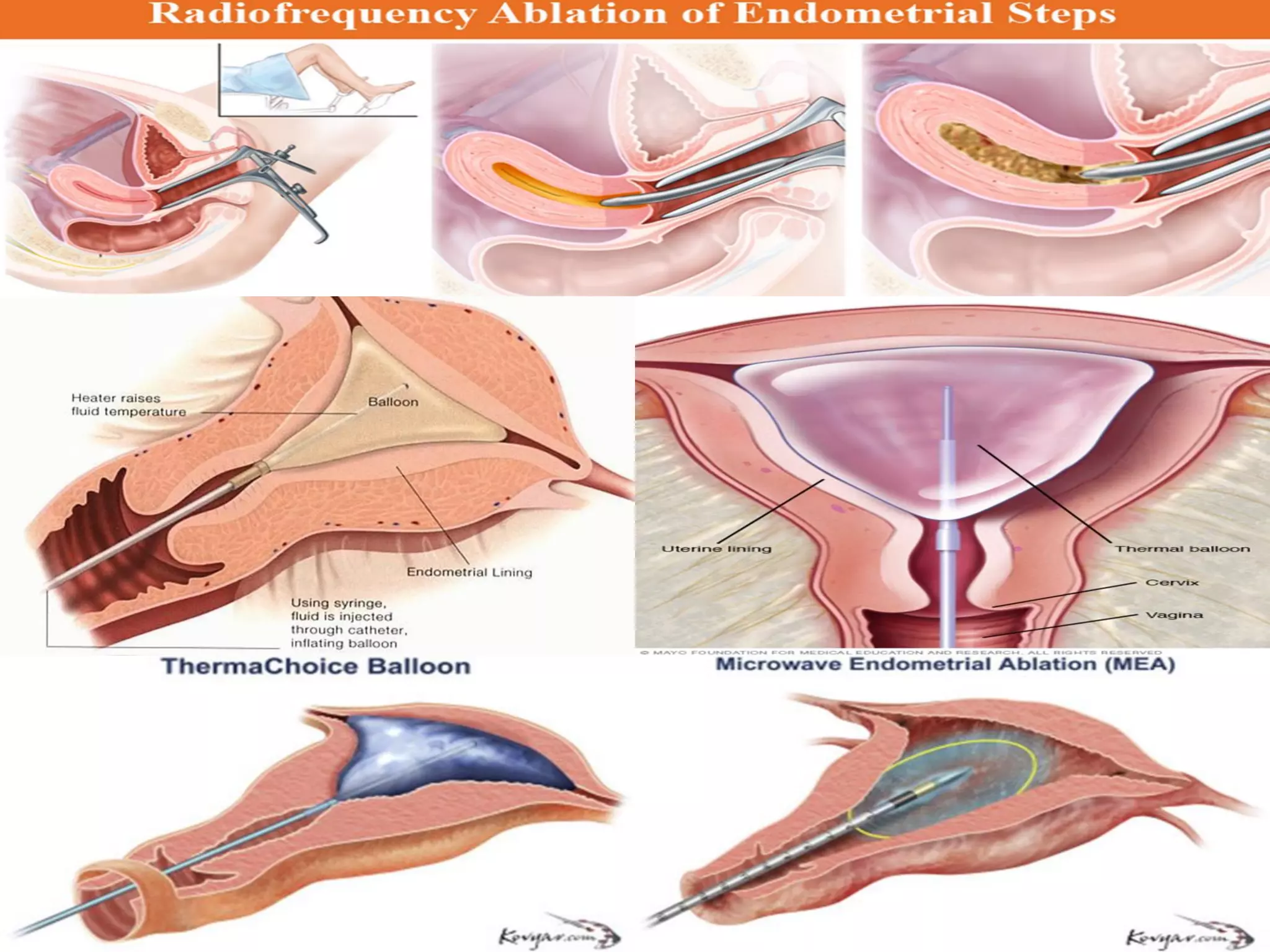
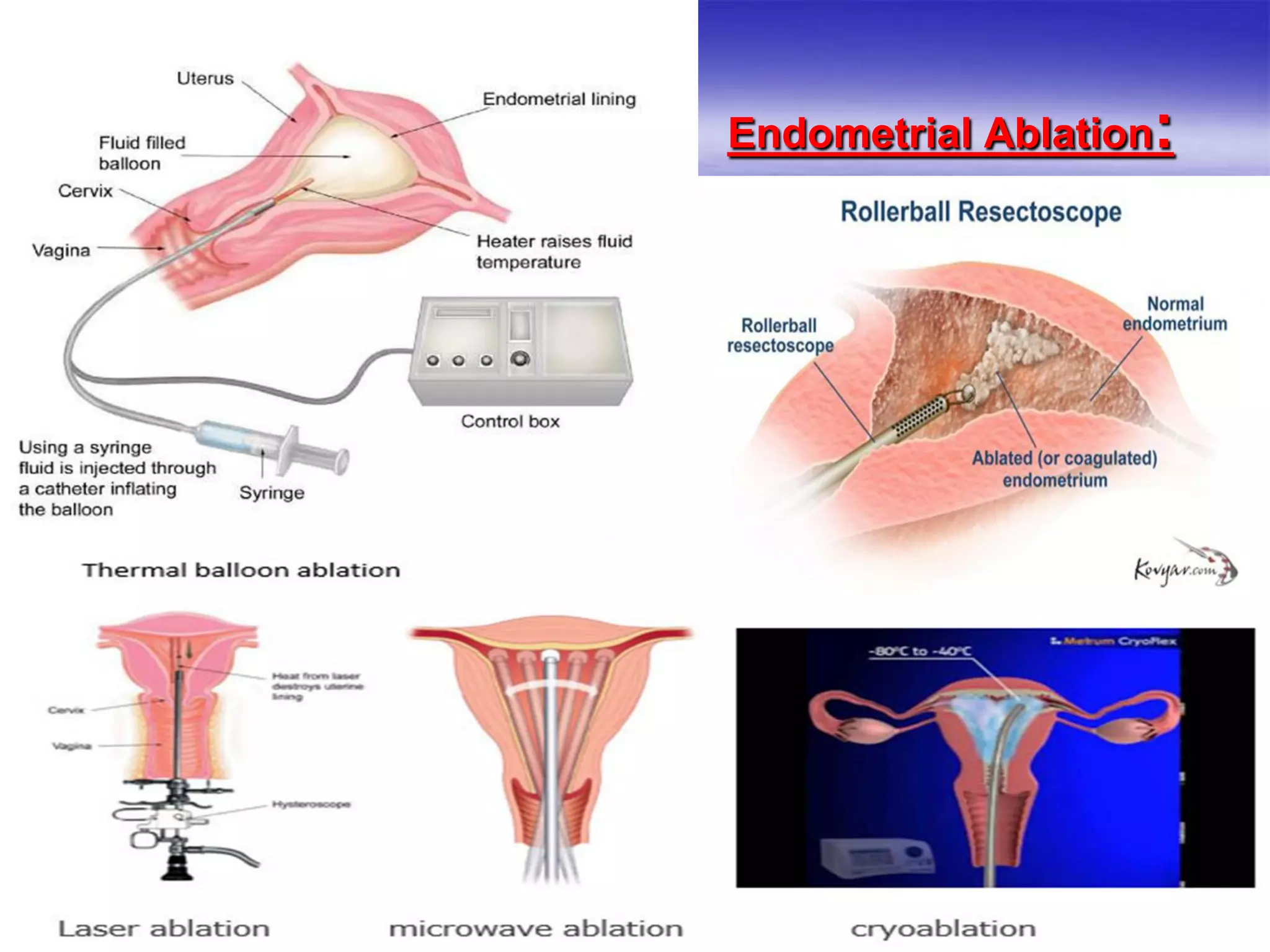
2. Endometrial ablation is presented as a minimally invasive option for abnormal uterine bleeding that does not require hysterectomy. Non-hysteroscopic methods like balloon and thermal ablation are discussed.
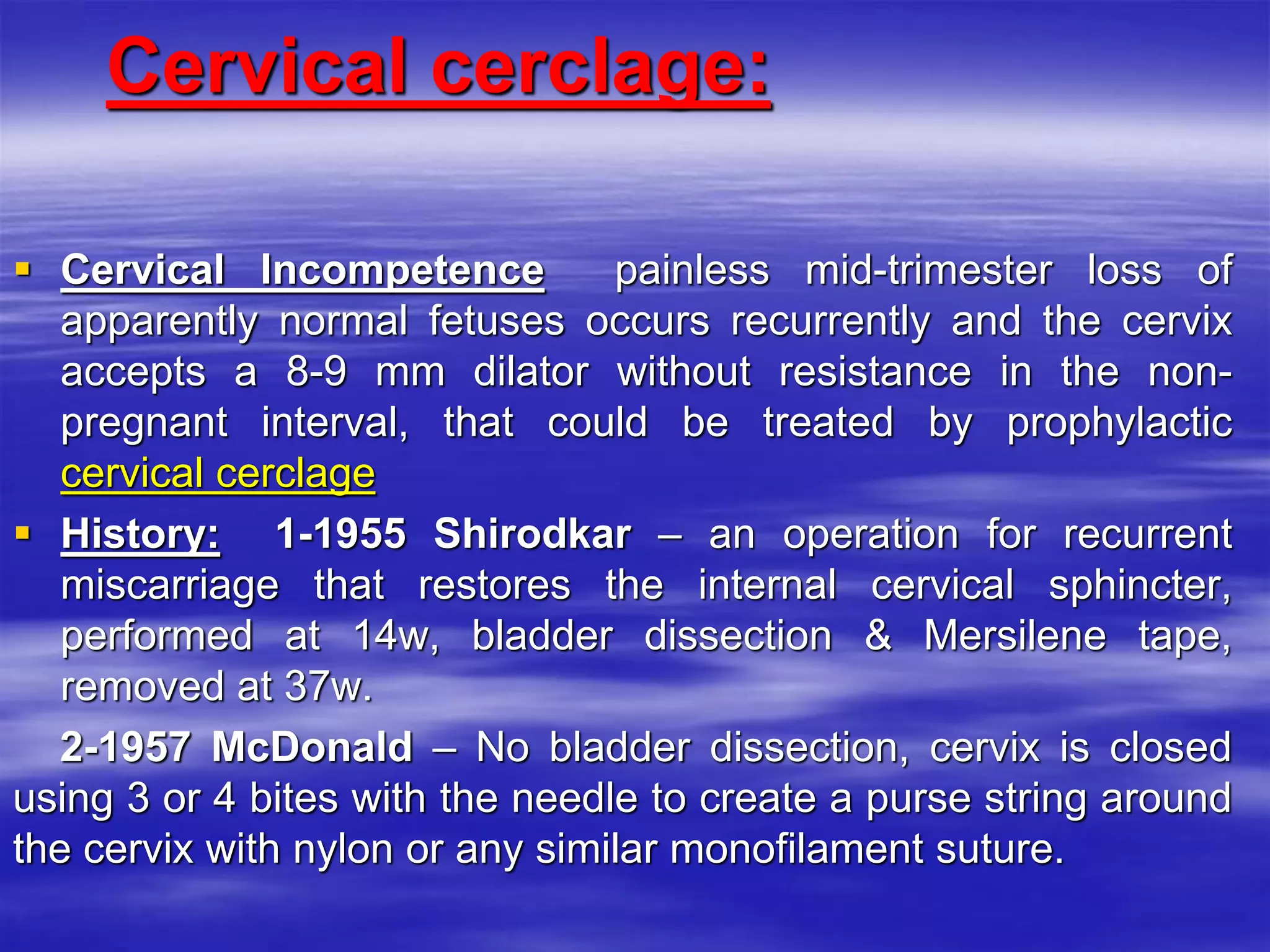
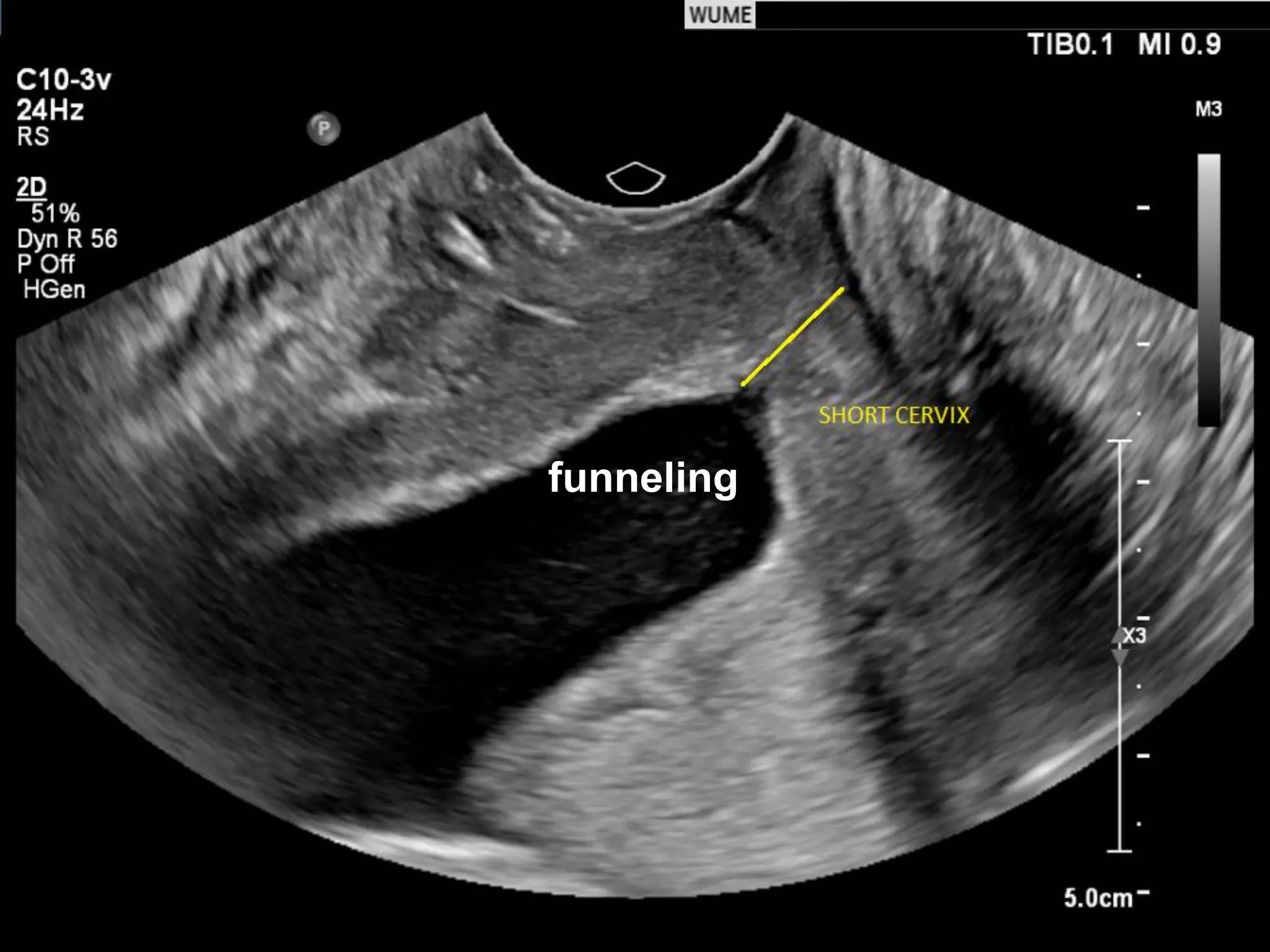
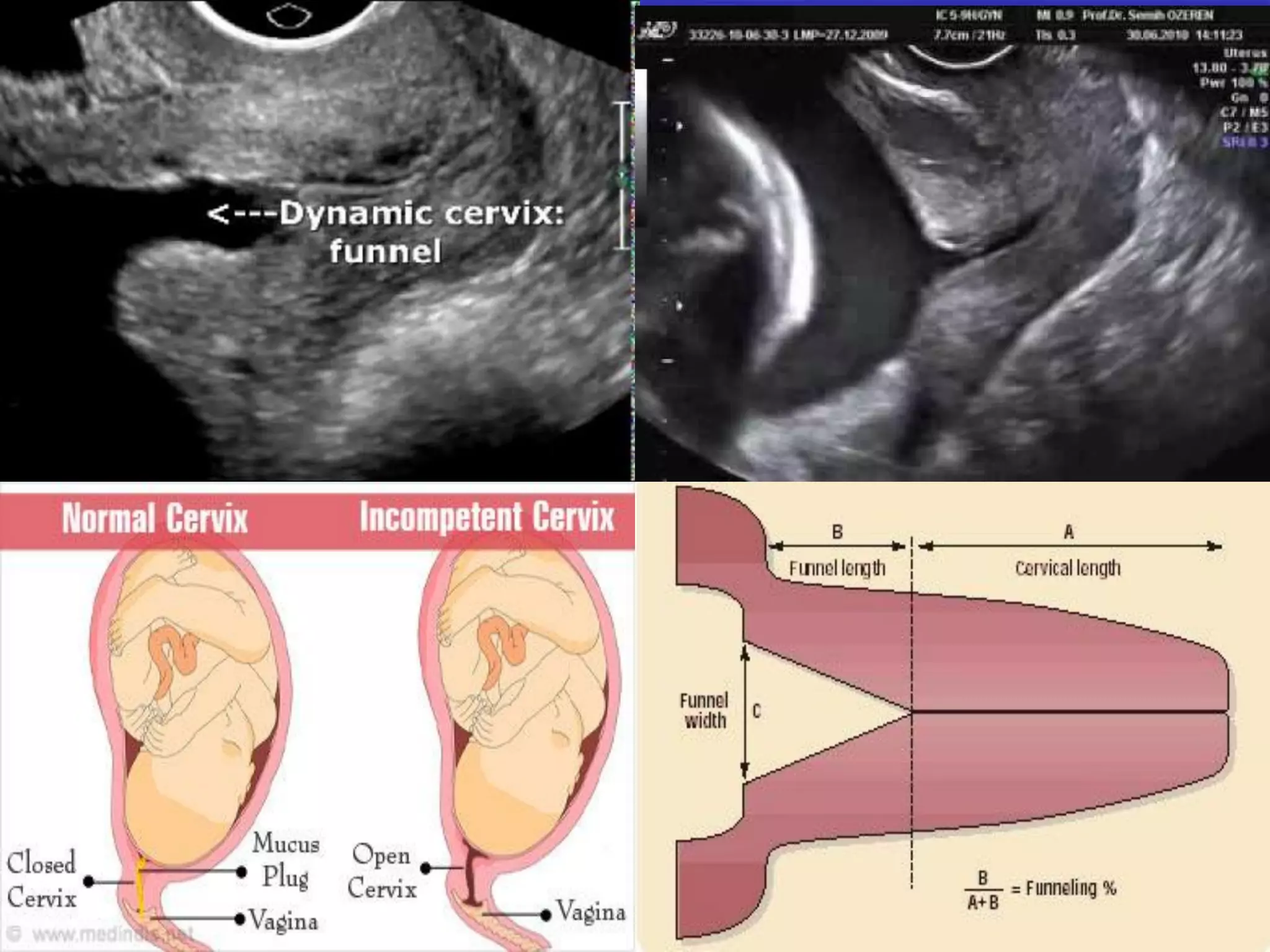
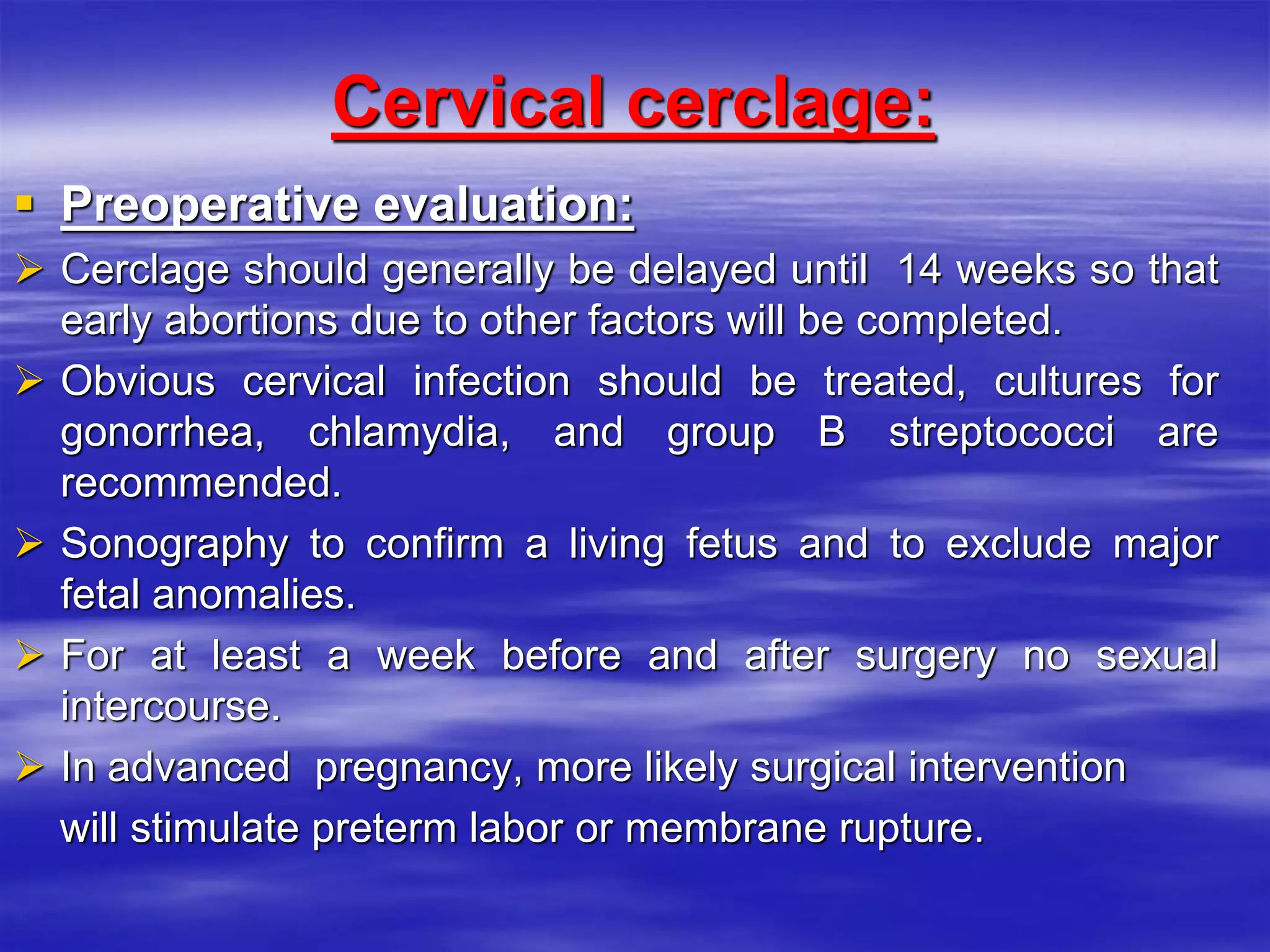
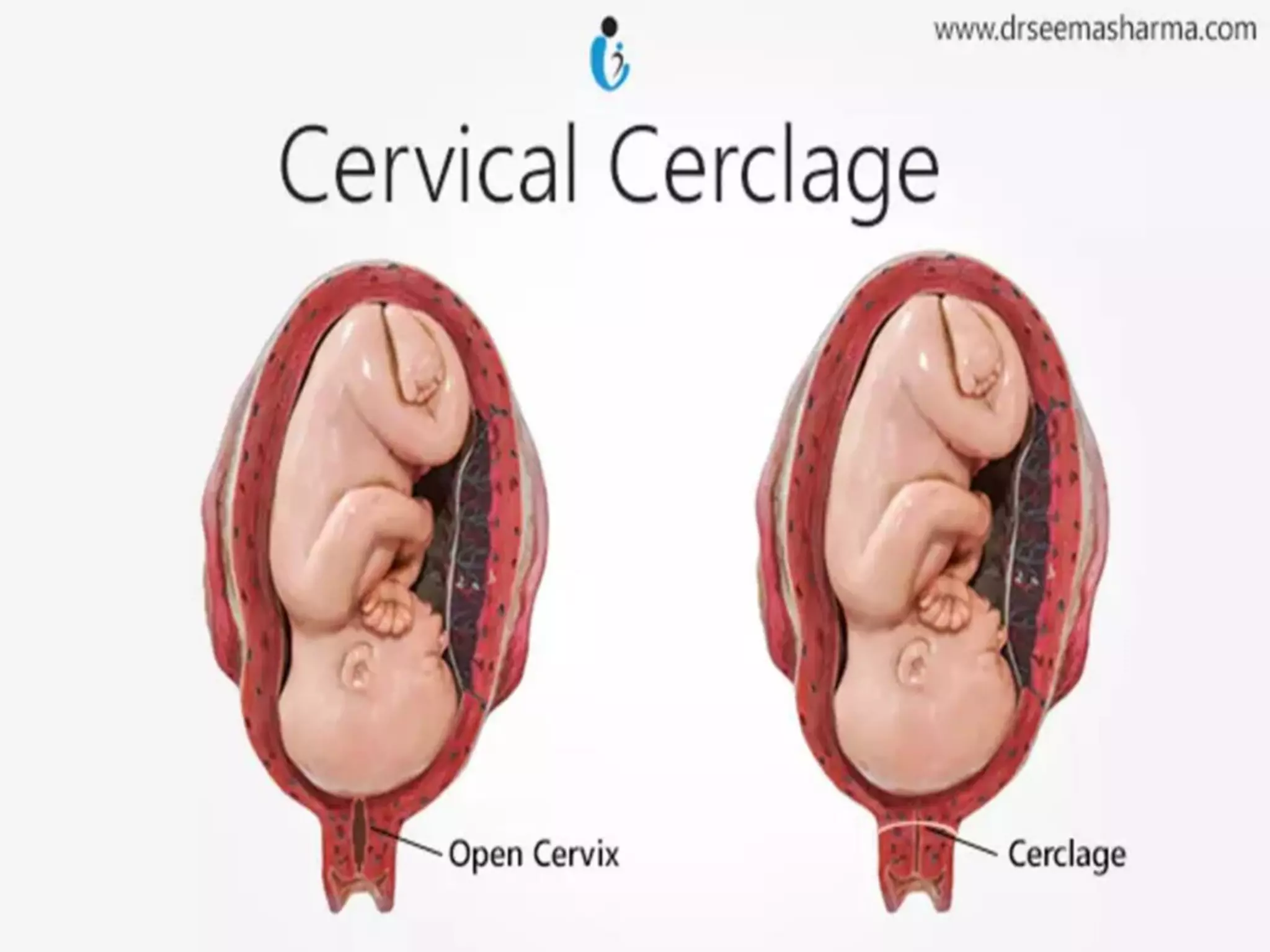
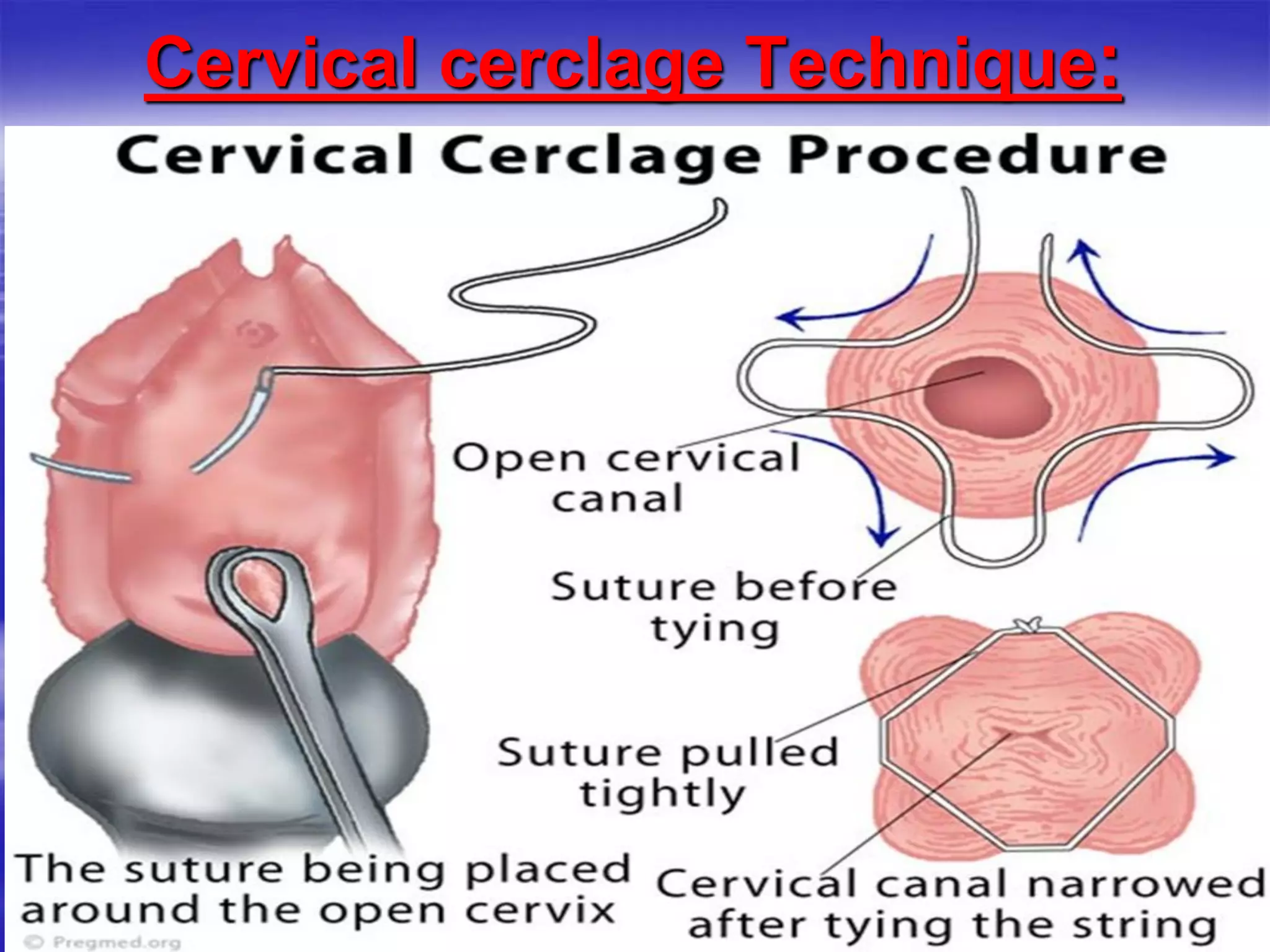
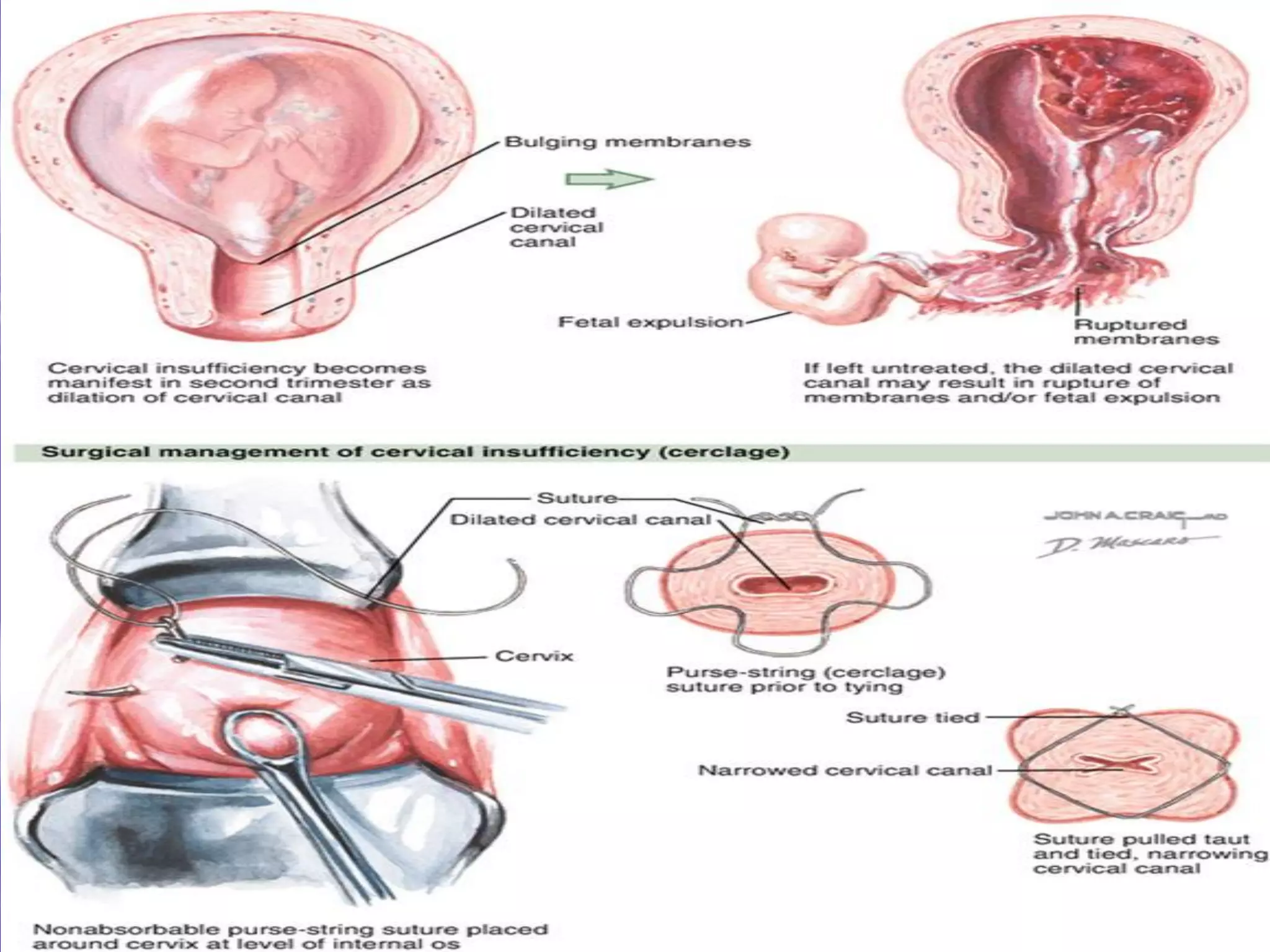
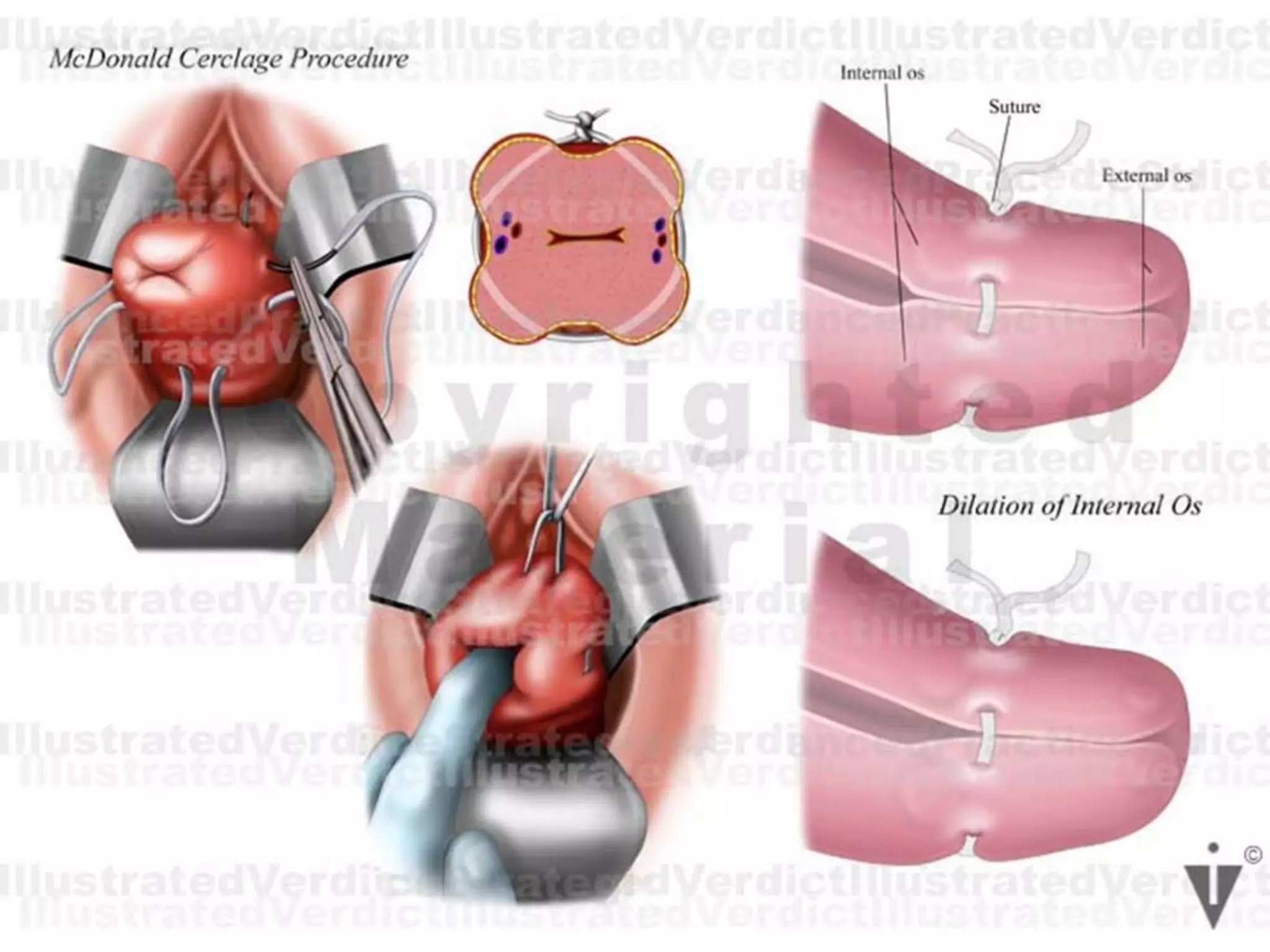
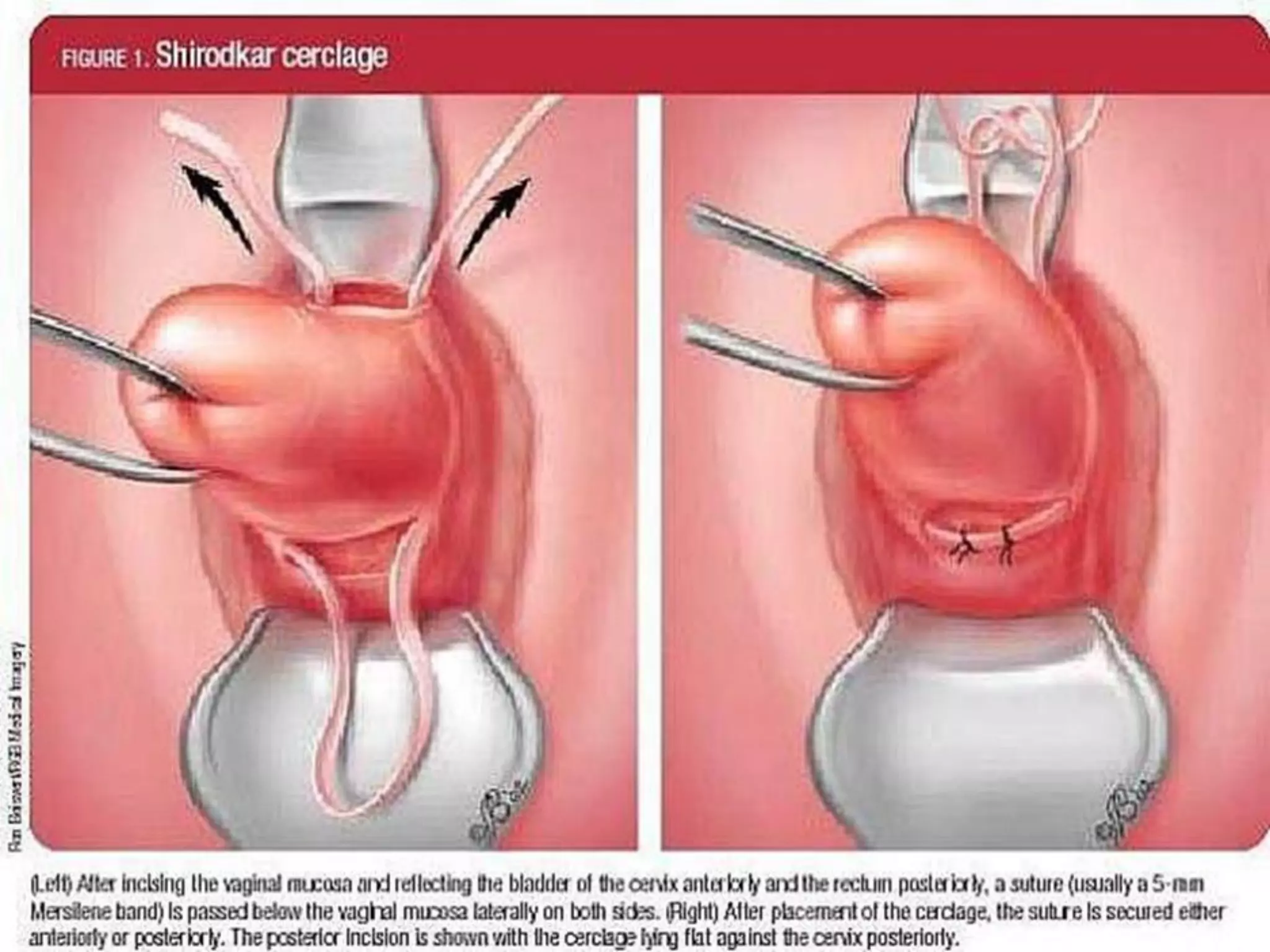
3. Cervical cerclage is explained as a surgical technique used to prevent cervical insufficiency and recurrent mid-trimester pregnancy loss, with prophylactic cerclage placed electively at 14 weeks