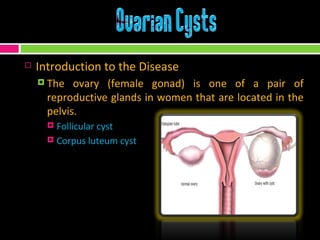
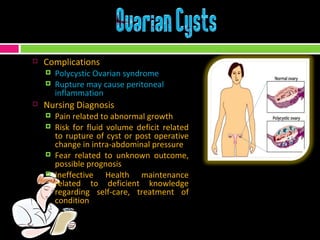
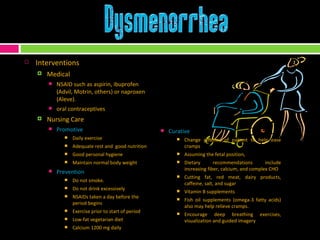
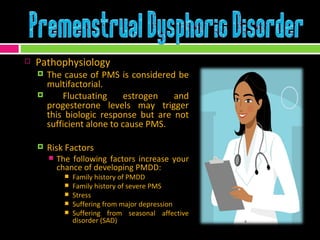
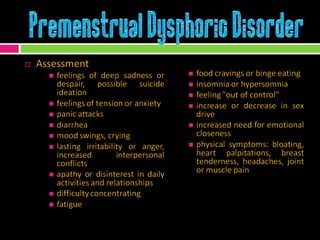
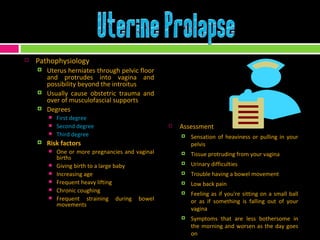
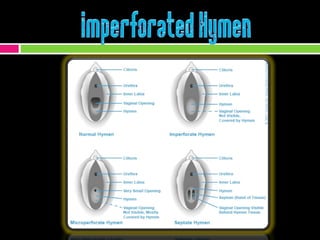
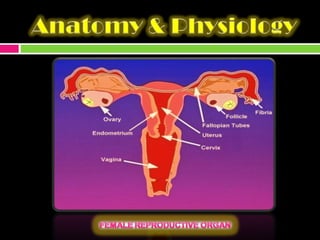
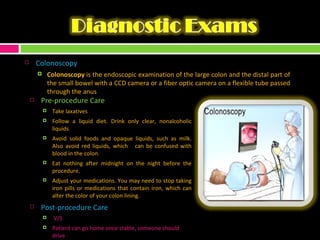
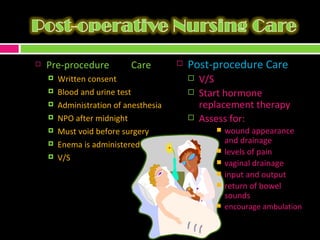
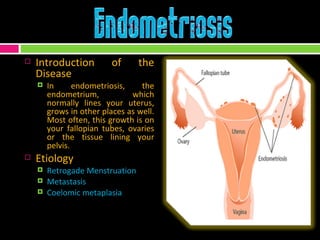
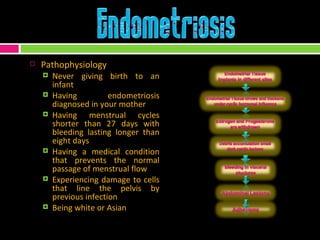
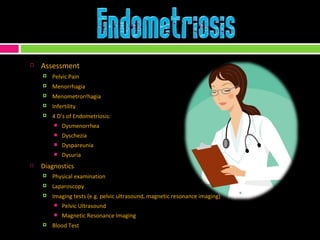
The document provides an extensive overview of the female reproductive system, detailing the anatomy, functions, and various conditions such as endometriosis, ovarian cysts, and dysmenorrhea. It discusses diagnostic procedures (e.g., laparoscopy, ultrasound), treatment options (medications and surgeries), and nursing care necessary for managing reproductive health. Additionally, it addresses complications and preventive measures to enhance women's health and well-being.
![Nursing Care Promotive daily exercise rest and nutrition good personal hygiene maintain ideal body weight Preventive have a regular physical exam; Pelvic exam use of oral contraceptives] Curative warm baths heating pad can help relax pelvic muscles, reducing cramping and pain teach patient relaxation techniques to control pain encourage patient to try position changes for sexual intercourse if experiencing dyspareunia Rehabilitative follow up check ups consider joining a support group for women with endometriosis or fertility problems.](https://image.slidesharecdn.com/group6-090314072134-phpapp02/85/REPRODUCTIVE-DISORDERS-OF-FENWICK-FILAMER-23-320.jpg)