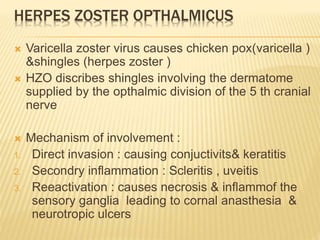
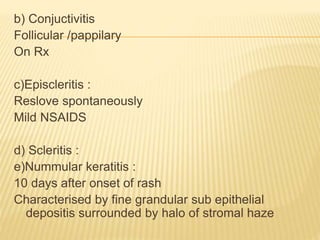
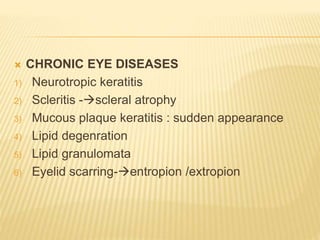
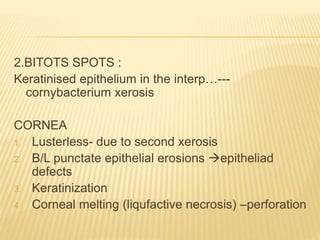
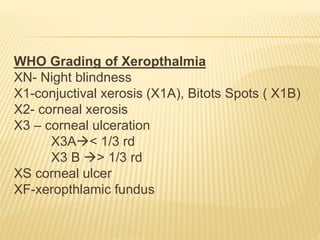
This document discusses various corneal diseases including herpes zoster ophthalmicus, syphilitic interstitial keratitis, acanthamoeba keratitis, onchocerciasis, and xerophthalmia. It describes the mechanisms, risk factors, signs, symptoms, investigations, and treatments for each condition. Key points include that herpes zoster ophthalmicus can cause acute or chronic eye involvement including epithelial keratitis, conjunctivitis, and neurotrophic keratitis. Syphilitic interstitial keratitis presents with limbitis, salmon patch vessels, and scarring. Acanthamoeba keratitis causes pseudodendrites, stromal infiltration,