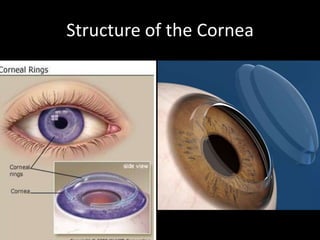
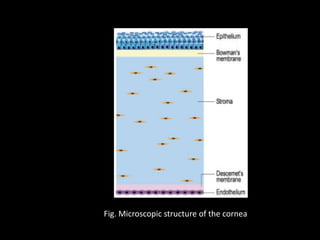
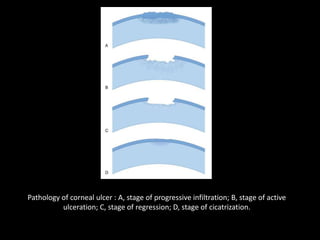
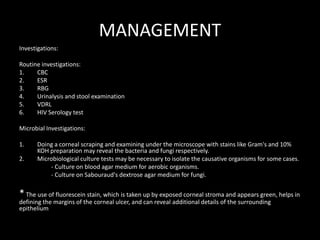
The document discusses corneal ulcer, beginning with the applied anatomy of the cornea. It defines corneal ulcer as the discontinuation of the normal epithelial surface. Causes can be infectious from bacteria, viruses, fungi, or protozoa, or noninfectious such as allergic, trophic, traumatic, idiopathic, vitamin A deficiency, or drug-induced. Clinical presentation includes pain, photophobia, tearing, redness, blurry vision, discharge, and foreign body sensation. Management involves investigations like cultures and scrapings to identify causative agents, followed by specific treatment targeting the agent and nonspecific treatments like antibiotics, cycloplegics, analgesics, and vitamins to aid healing. Complications can include