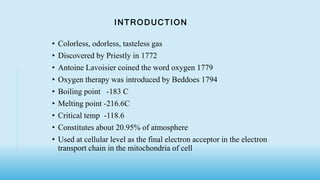
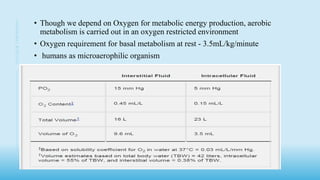
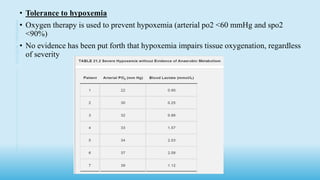
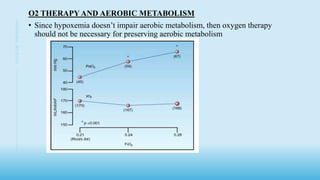
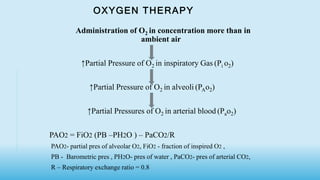
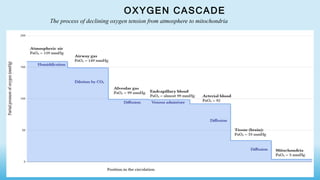
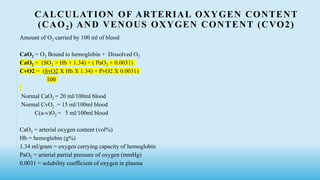
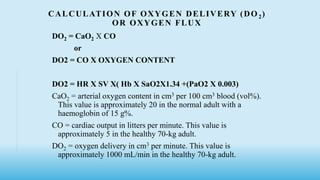
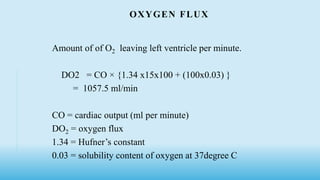
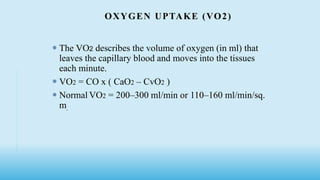
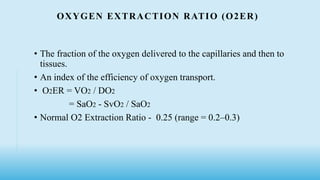
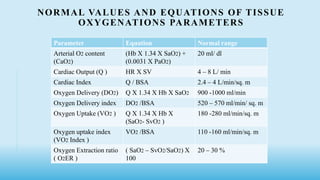
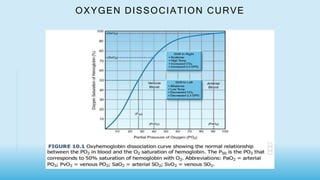
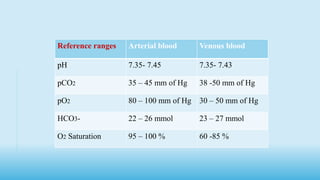
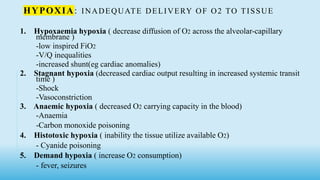
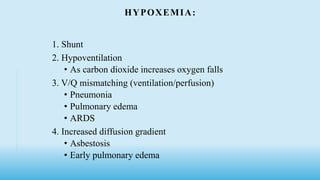
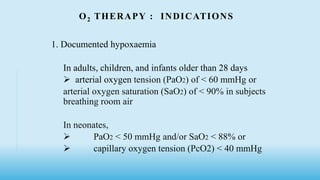
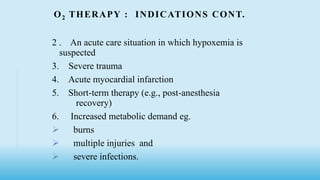
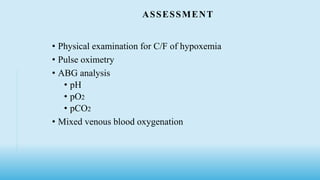
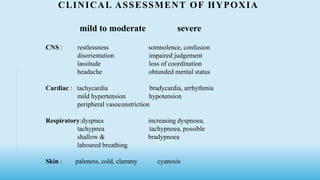
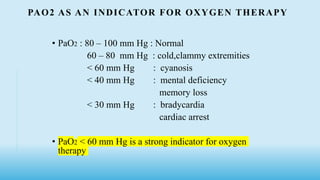
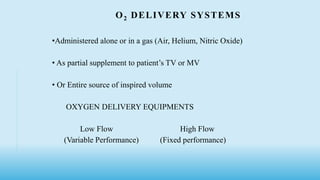
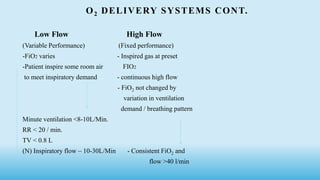
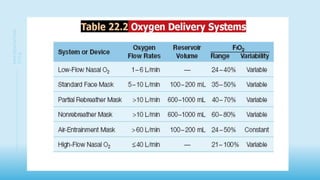
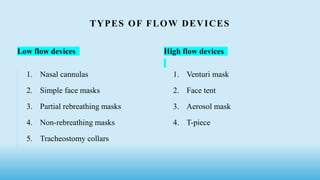
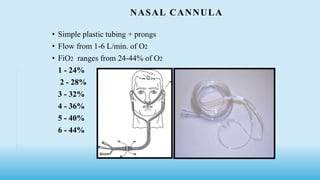
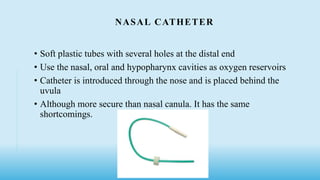
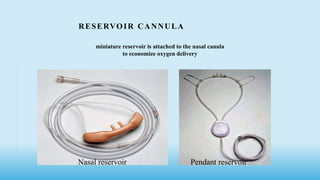
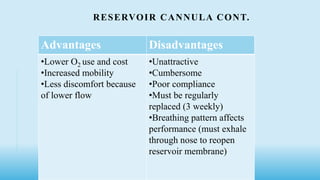
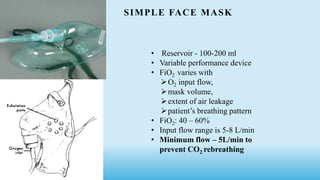
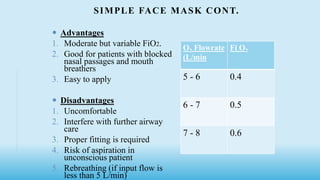
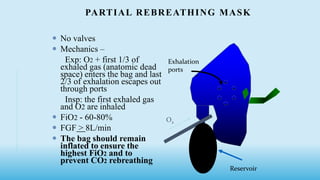
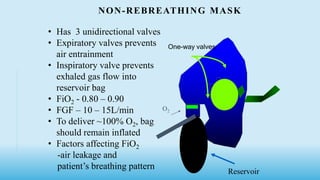
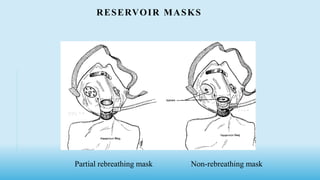
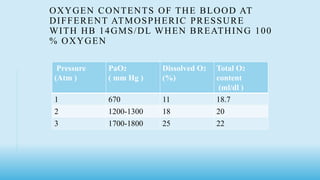
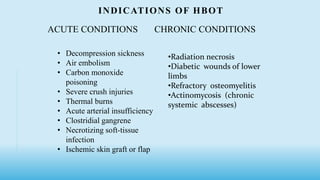
The document discusses oxygen therapy and administration, including the types of oxygen delivery systems like nasal cannulas, simple face masks, and reservoir masks. It covers indications for oxygen therapy when hypoxemia is present based on arterial blood gas values. Equations are provided for calculating oxygen content, delivery, uptake, and extraction from the blood under normal conditions.