This document provides tips for using a PowerPoint presentation on hydronephrosis:
1. The presentation contains blank slides for active learning where the user or students can provide information before the next slide is shown.
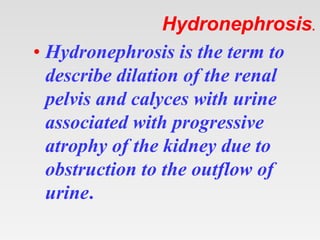
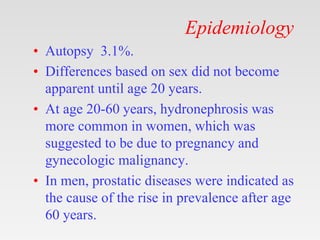
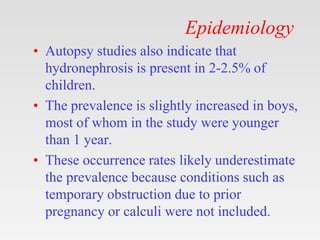
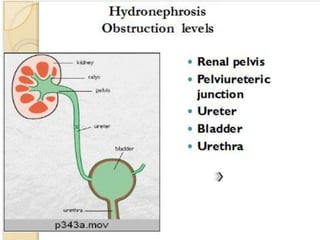
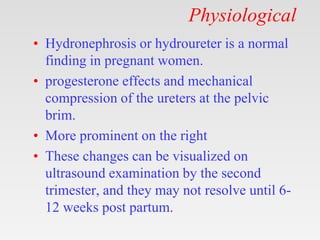
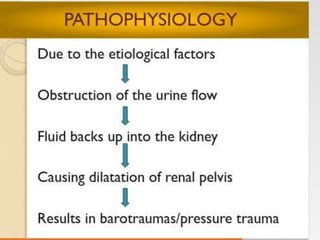
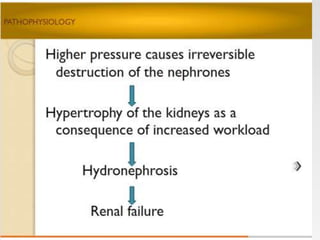
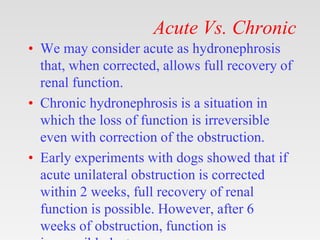
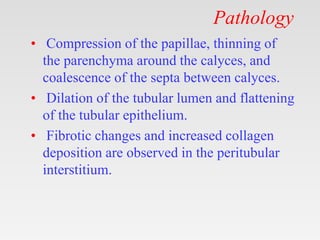
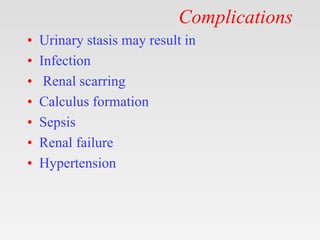
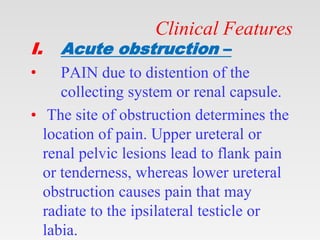
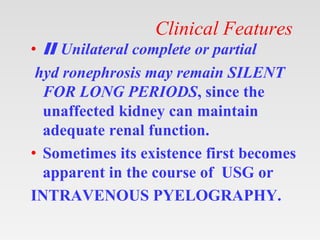
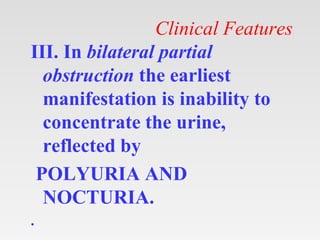
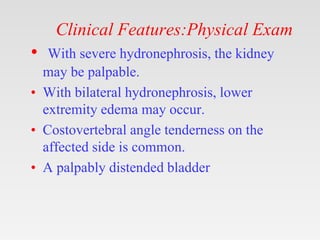
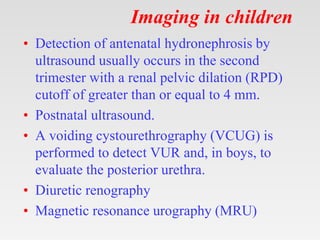
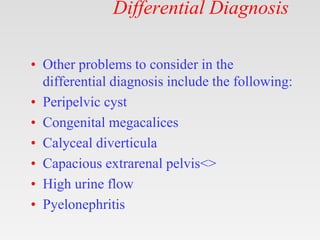
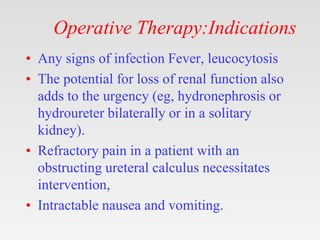
2. It covers topics like the definition, causes, epidemiology, pathology, clinical features, diagnostic studies, differential diagnosis, and treatment of hydronephrosis.
3. By displaying blank slides and having the user or students think about and discuss each topic before showing the next slide, this presentation aims to create an active learning session that can benefit both individual and group study.