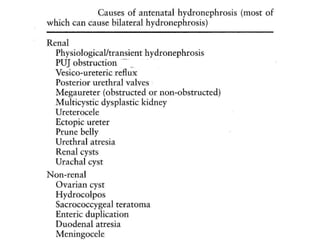
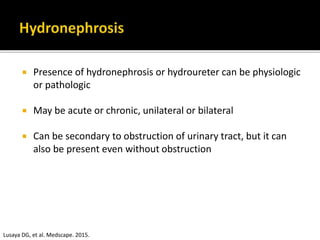
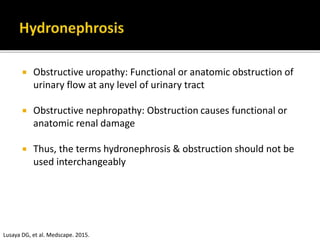
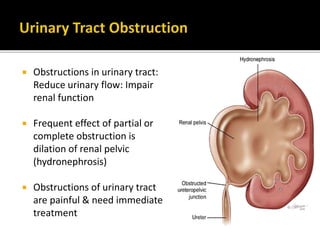
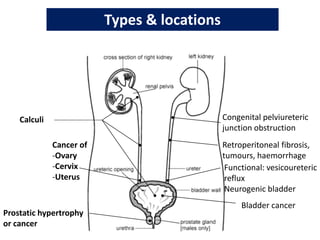
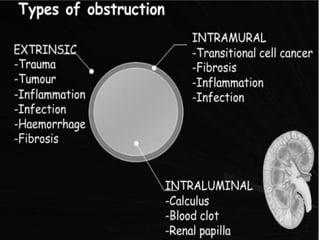
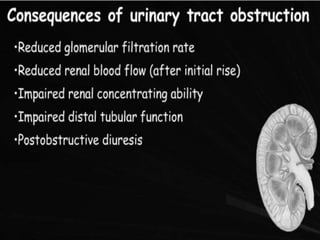
Hydronephrosis and hydroureter are common conditions, arising from obstruction in the urinary tract, which can be either physiologic or pathologic, and can be classified based on etiology and location of the obstruction. They can lead to significant renal damage and are associated with various causes, differing between adults and children. Diagnosis typically involves imaging techniques, while management may require surgical intervention, especially in cases of severe persistent hydronephrosis.

![ Symptoms vary depending on whether hydronephrosis is
acute or chronic
With acute obstruction, pain is frequently present, due to
distention of bladder, collecting system, or renal capsule
Pain is typically minimal or absent with partial or slowly
developing obstruction (as with congenital ureteropelvic
junction [UPJ] obstruction or a pelvic tumor). It is not
uncommon, for example, to see an adult who is noted to
have hydronephrosis due to previously unsuspected UPJ
obstruction
Lusaya DG, et al. Medscape. 2015.](https://image.slidesharecdn.com/hydronephrosis-240712062155-07cf70a8/85/Hydronephrosis-pptxbbbbbbbbbbbbbbbbbbbbbbtb-31-320.jpg)