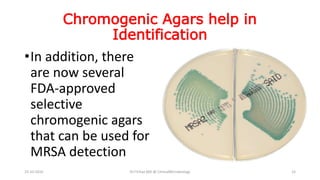
MRSA is a type of staph bacteria that is resistant to certain antibiotics such as methicillin and penicillin. It can cause infections of the skin or other parts of the body. MRSA was first identified in the 1960s and has since emerged in both healthcare and community settings. Risk factors for MRSA infection include prior MRSA infection or colonization, exposure to healthcare settings, and underlying medical conditions. Laboratories test for MRSA resistance using methods such as cefoxitin disk screening and PCR detection of the mecA gene. Proper hand hygiene and infection control practices can help reduce the spread of MRSA.



![What do you understand by
Vancomycin Resistance
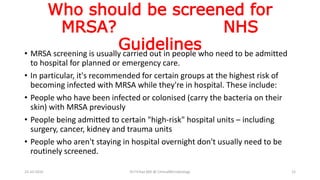
• Since 1996, MRSA strains
with decreased
susceptibility to
vancomycin (minimum
inhibitory concentration
[MIC], 4 – 8 μg/ml) and
strains fully resistant to
vancomycin (MIC ≥ 32
μg/ml) have been reported.
23-10-2016 Dr.T.V.Rao MD @ ClinicalMicrobiology 22](https://image.slidesharecdn.com/mrsa-161023101829/85/Screening-for-MRSA-22-320.jpg)