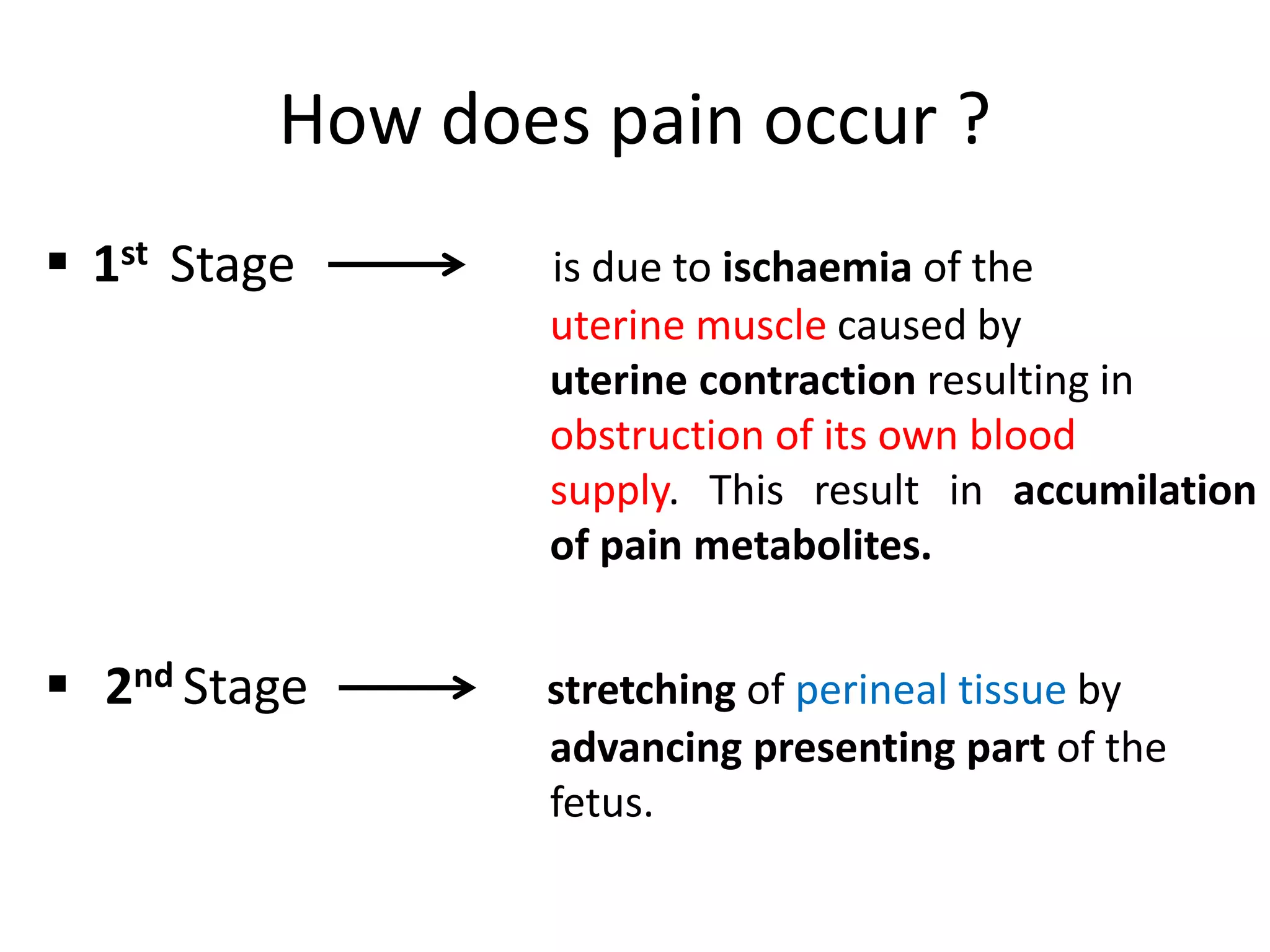
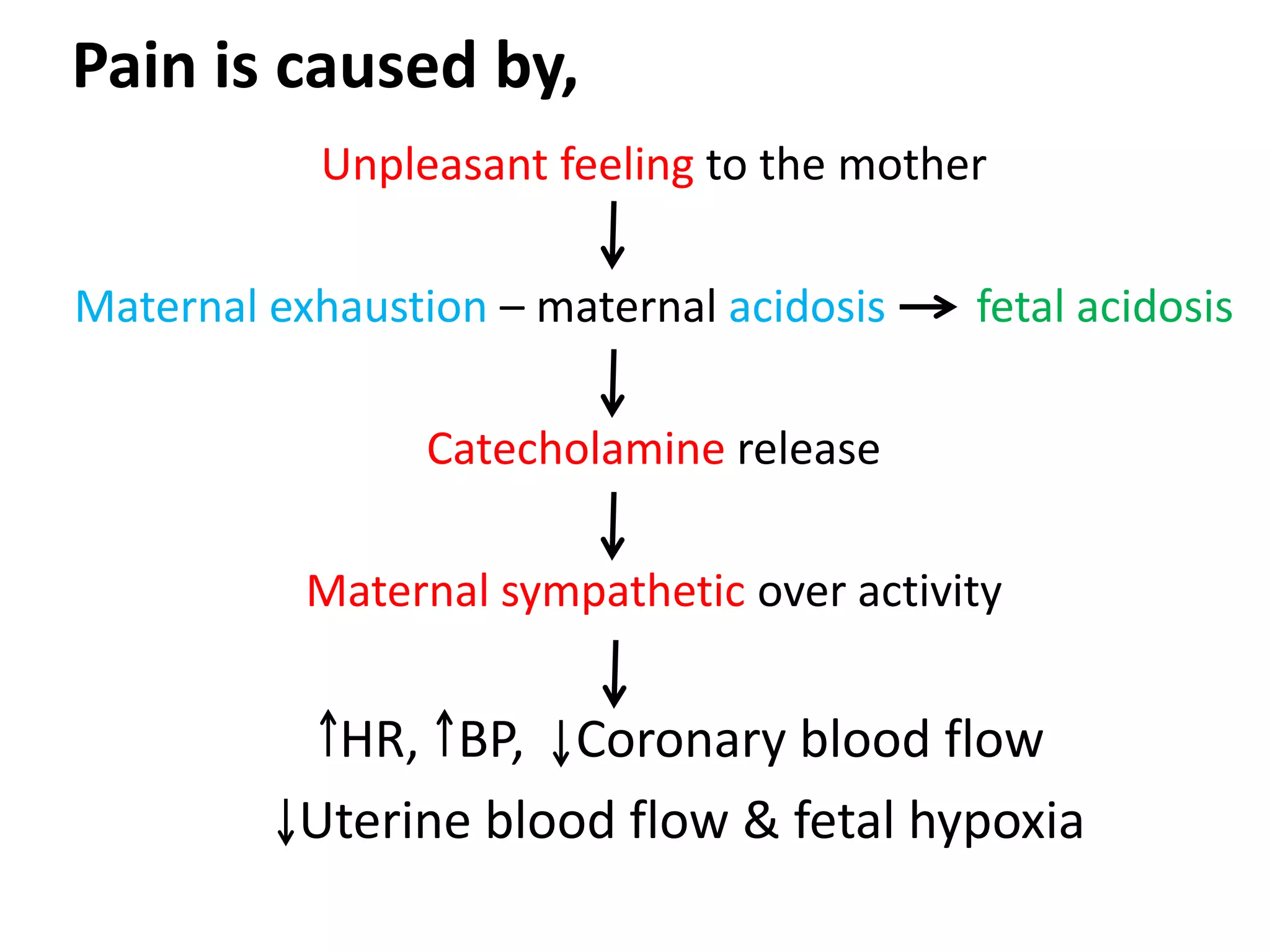
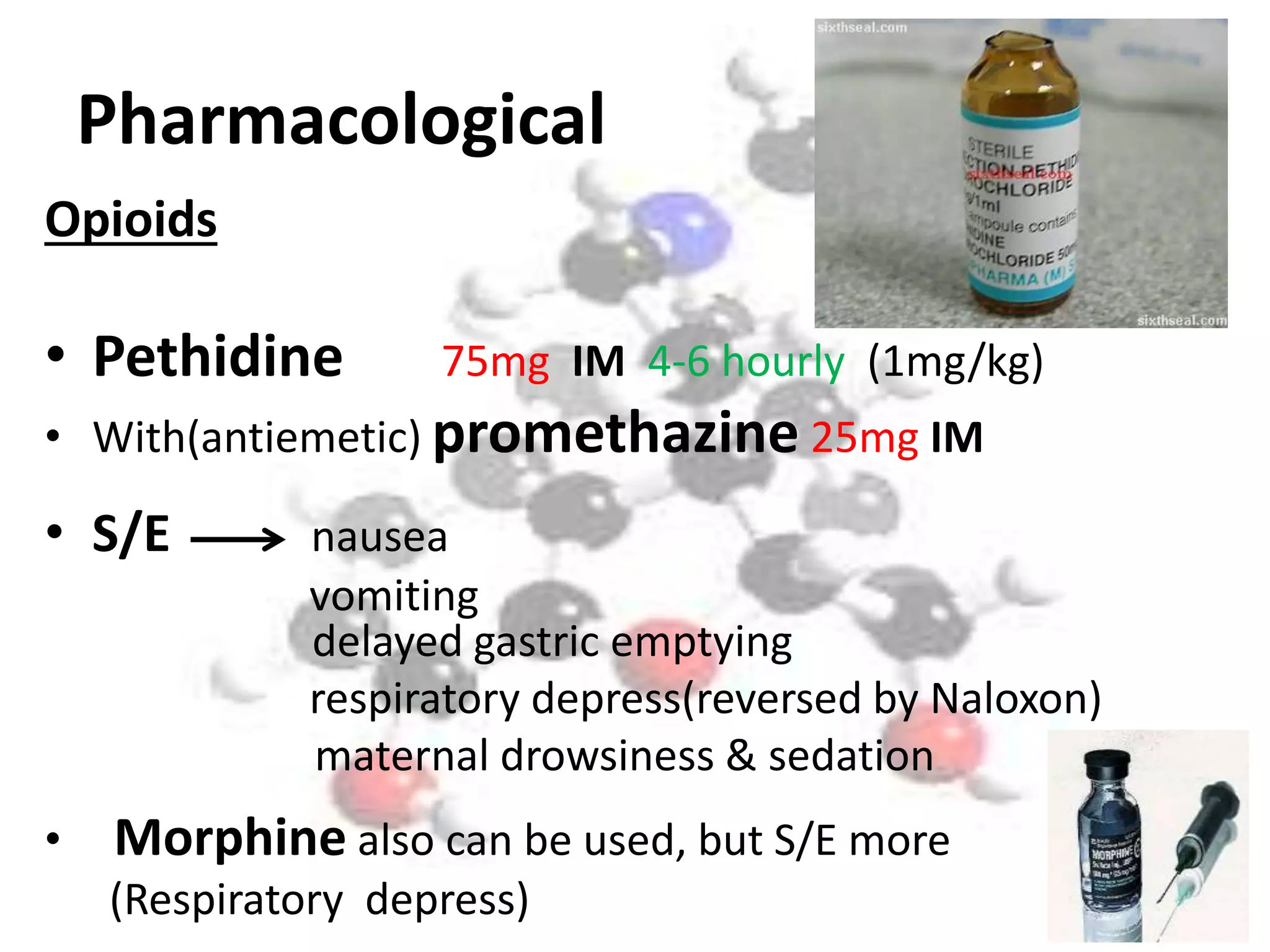
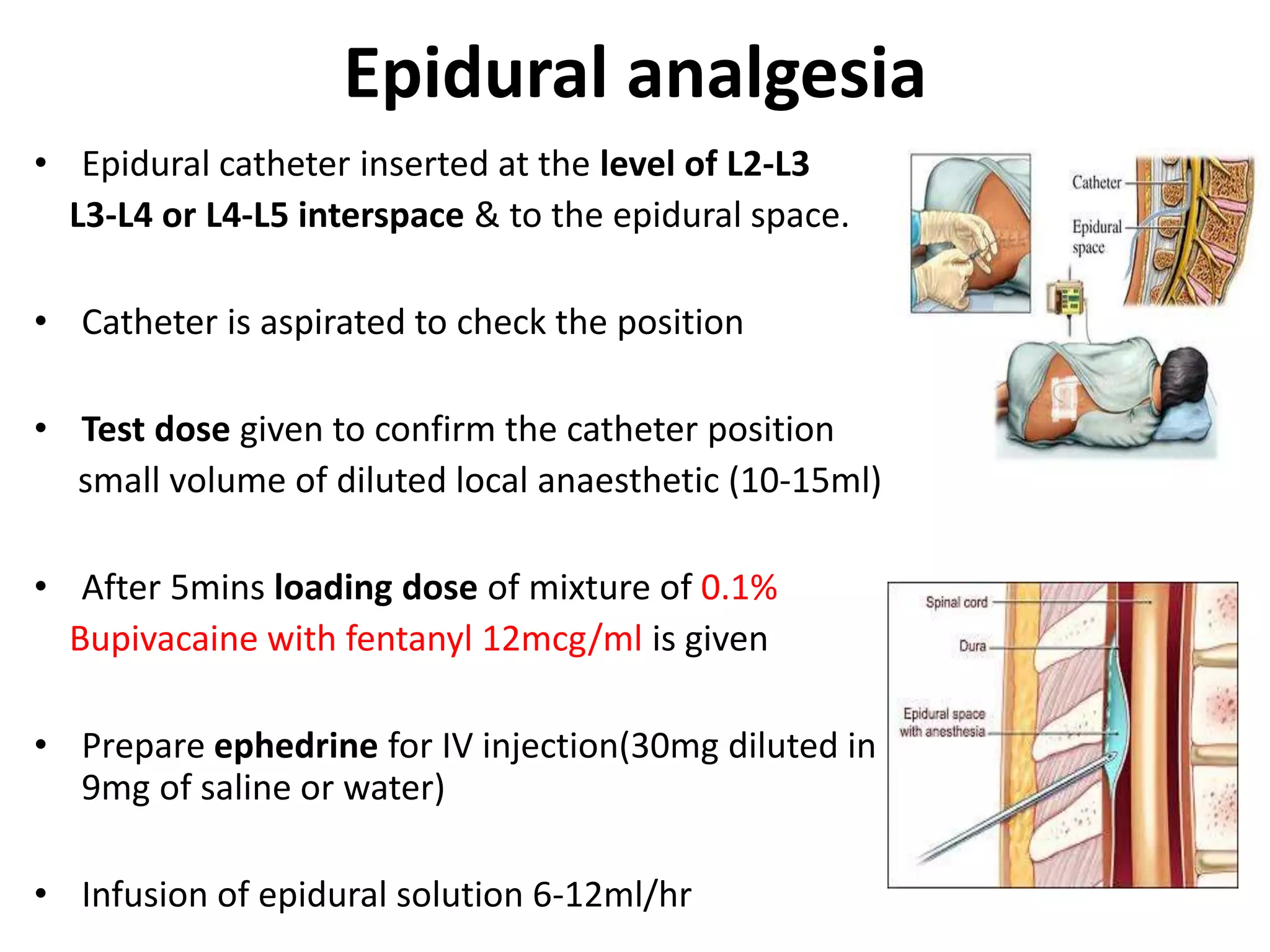
The document discusses pain relief in labor, detailing the causes of labor pain, including ischaemia of the uterine muscle and stretching of perineal tissue. It outlines various pain relief methods, both pharmacological (like opioids and epidurals) and non-pharmacological (like education and relaxation techniques). The document also highlights the administration procedures, contraindications, and potential complications associated with these analgesic options.