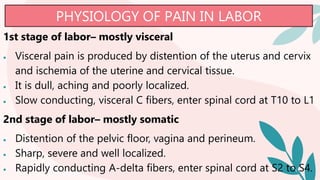
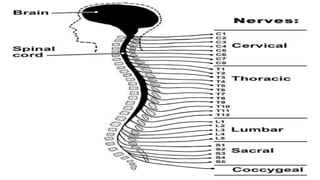
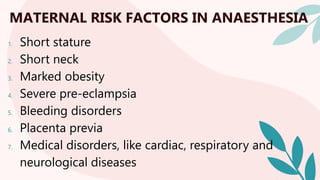
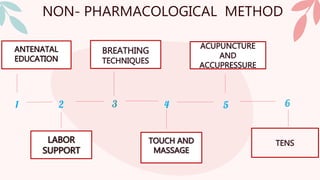
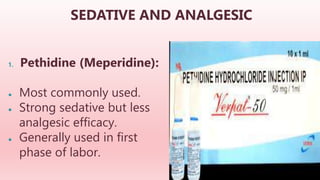
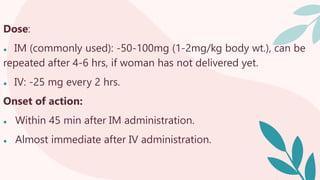
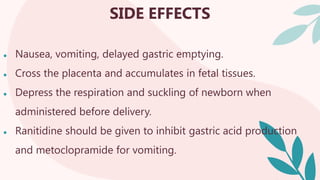
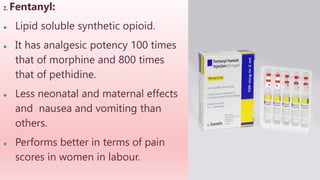
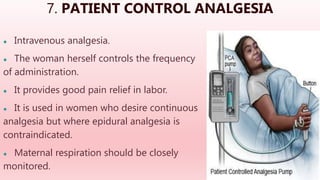
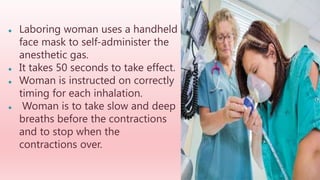
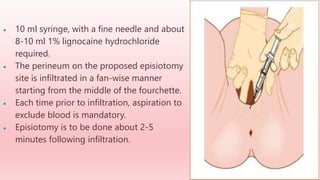
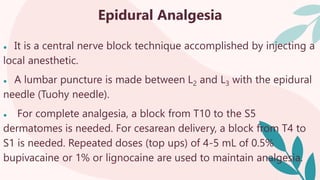
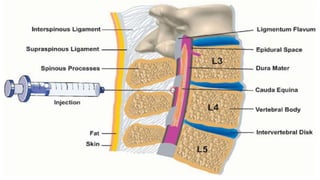
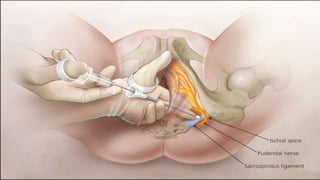
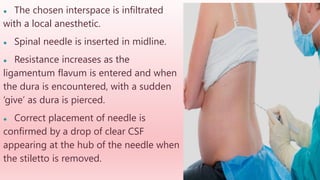
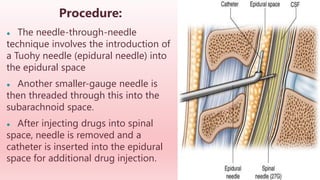
The document discusses various methods of providing anesthesia and analgesia during labor. It begins by defining anesthesia and analgesia. It then discusses the physiology of pain during the first and second stages of labor. It outlines maternal risk factors for anesthesia and debates whether labor pain requires analgesia. The majority of the document then examines both non-pharmacological and pharmacological methods for pain management, including sedatives, regional techniques like epidural and spinal anesthesia, and inhalation methods. It provides details on procedures, dosages, onset times and complications for each method.