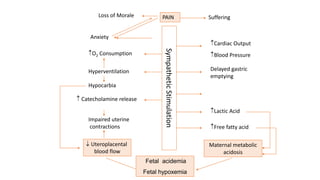
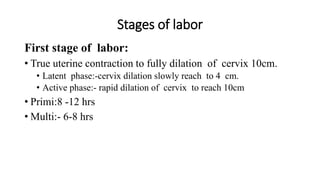
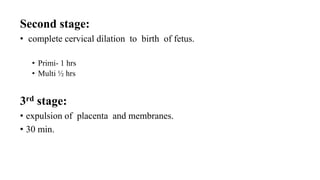
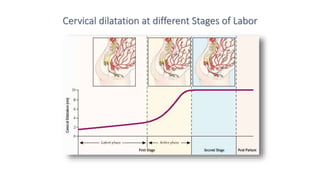
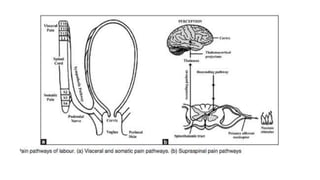
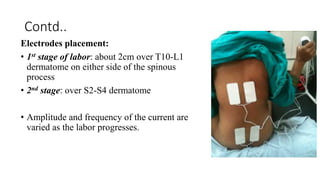
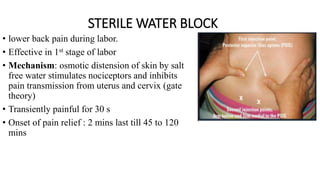
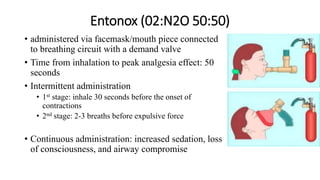
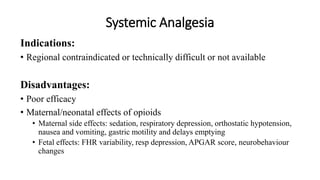
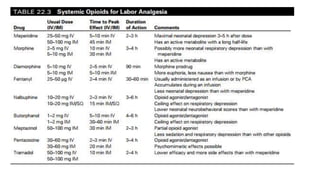
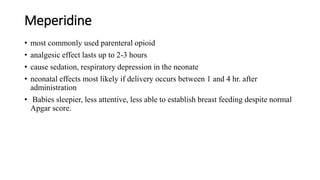
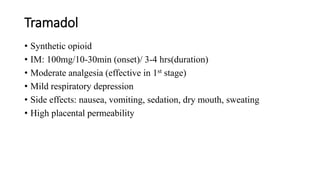
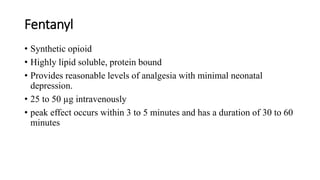
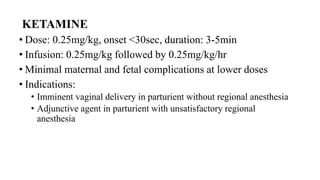
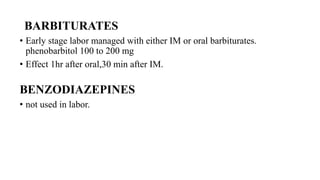
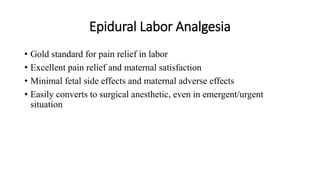
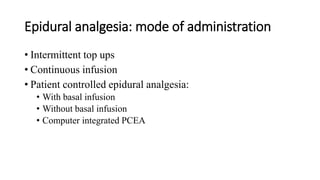
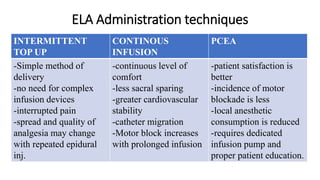
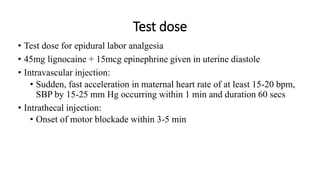
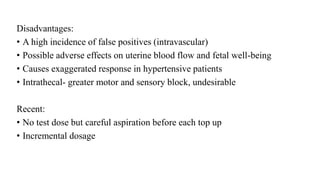
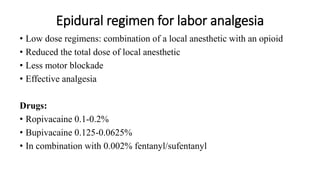
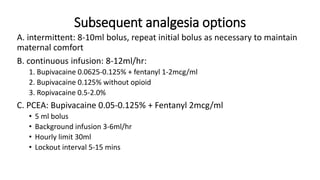
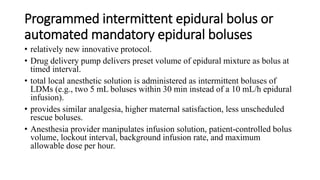
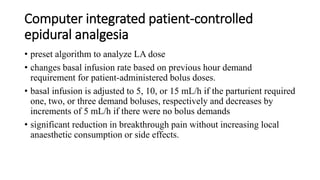
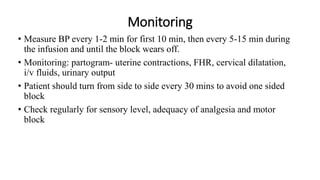
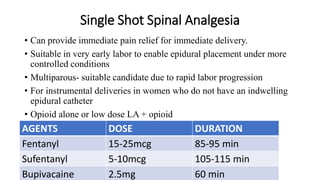
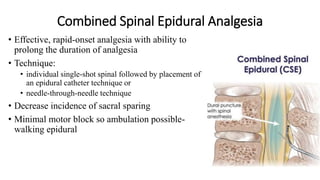
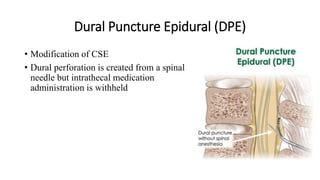
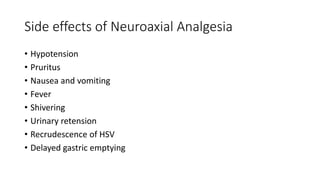
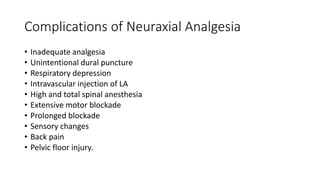
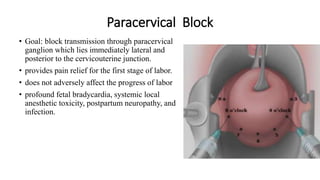
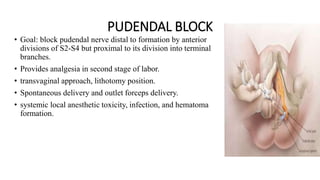
This document discusses various methods of labor analgesia. It begins by outlining the objectives and introducing the stages of labor and physiology of pain. It then summarizes non-pharmacological methods like psychoprophylaxis and TENS. Various pharmacological methods are discussed including inhalational analgesia, systemic opioids, and regional techniques like epidural analgesia, combined spinal epidural, and walking epidural. Epidural analgesia is described as the gold standard, and optimal epidural regimens, administration techniques, and monitoring are outlined.