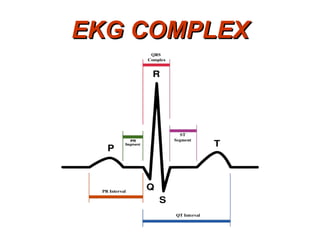
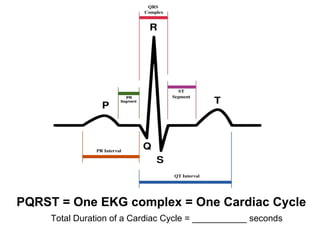
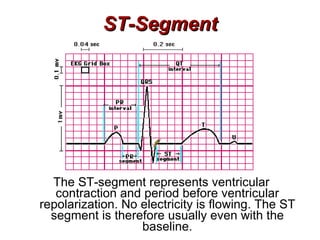
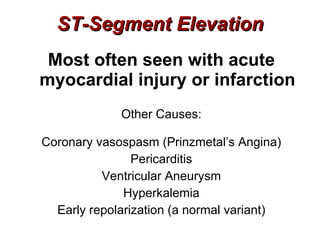
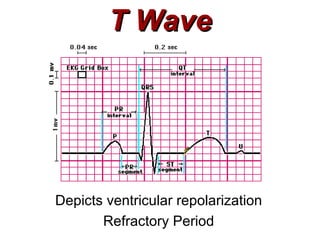
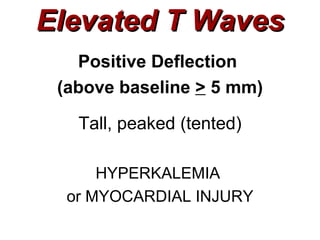
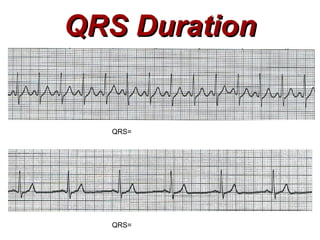
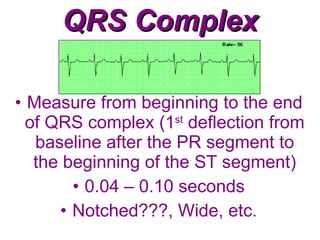
This document provides a high-level overview of cardiac electrophysiology and EKG interpretation. It discusses the different types of cardiac cells, the cardiac action potential, and the phases of the cardiac cycle. It describes how electrical signals travel through the heart via specialized conduction pathways, and explains common EKG complexes and intervals like the P wave, QRS complex, and ST segment. Key concepts covered include the roles of the sinoatrial node, atrioventricular node, and Purkinje fibers in cardiac conduction.