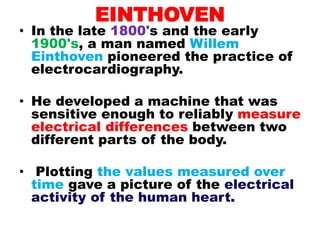
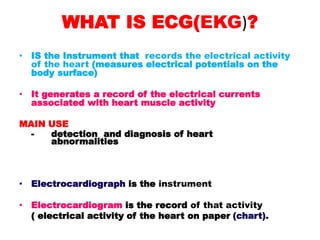
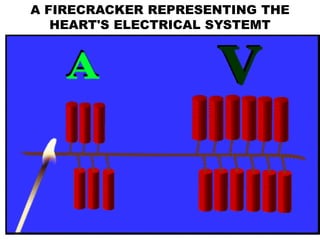
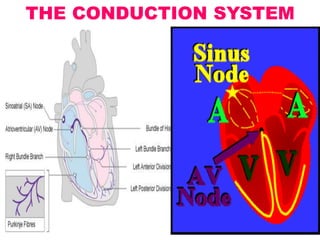
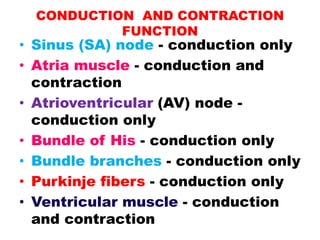
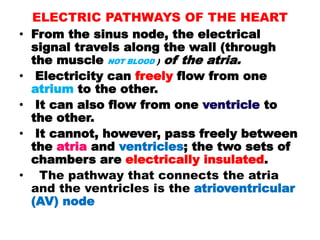
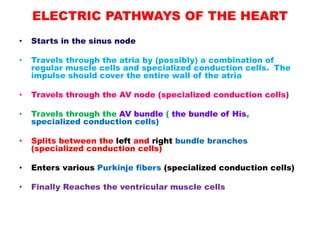
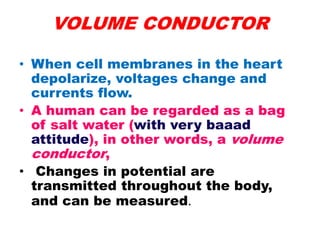
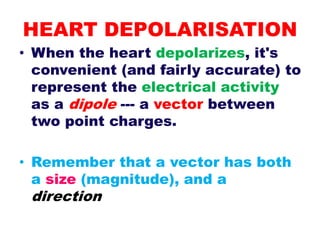
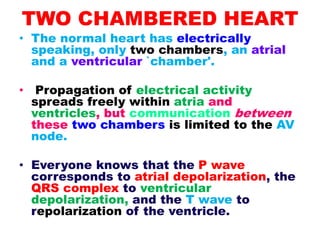
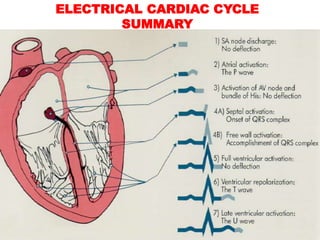
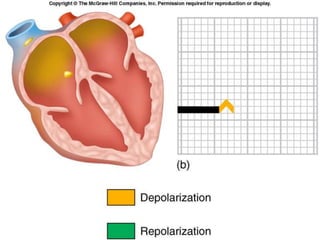
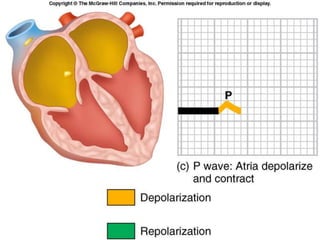
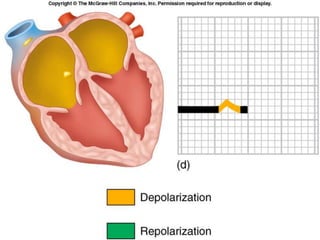
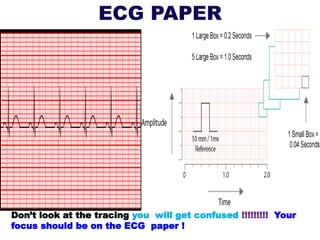
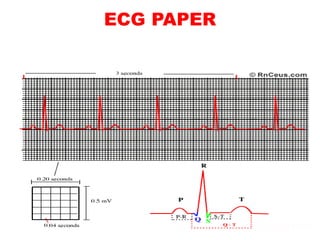
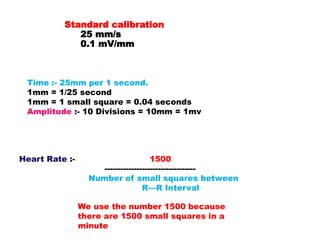
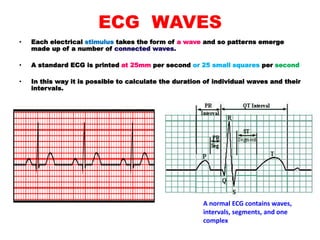
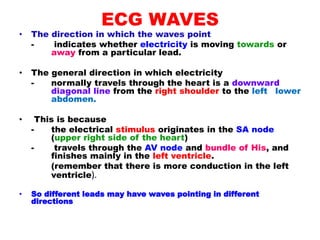
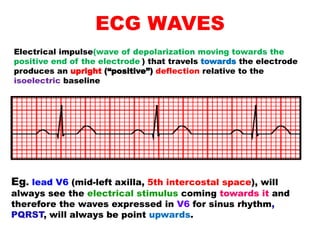
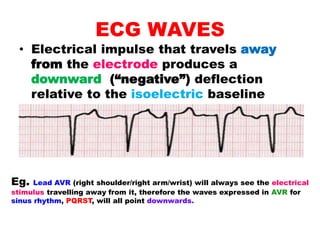
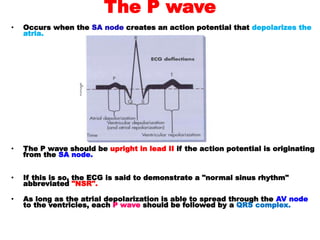
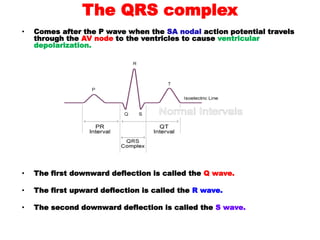
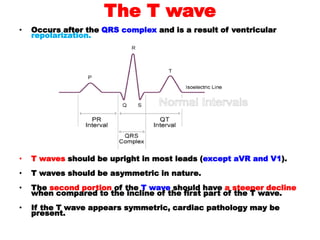
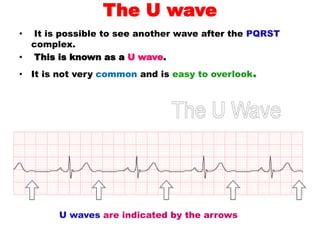
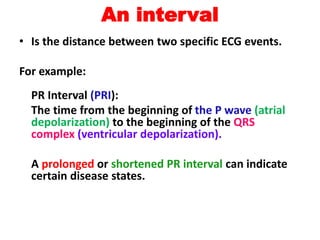
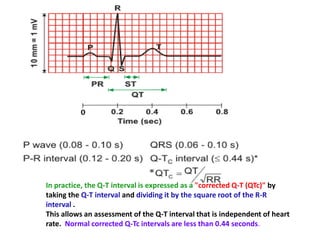
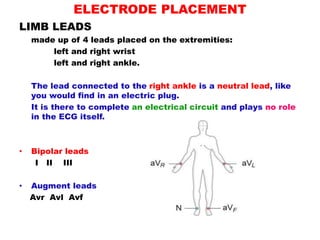
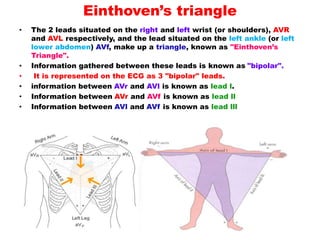
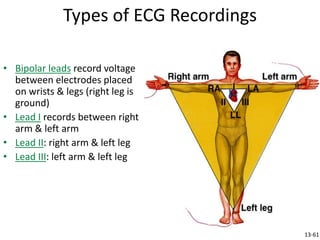
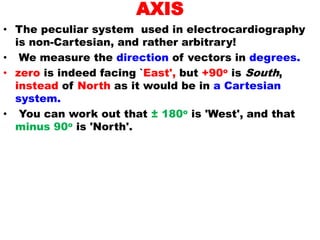
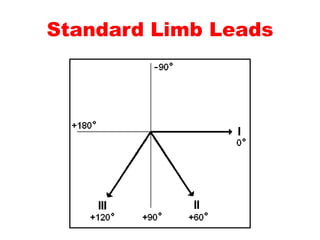
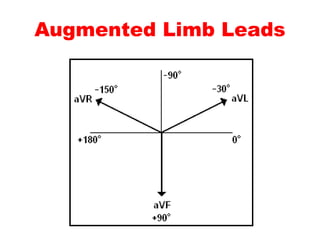
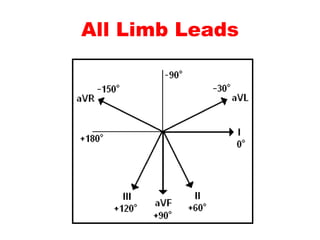
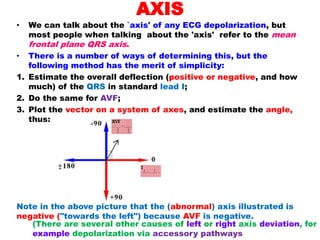
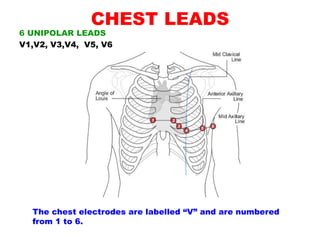
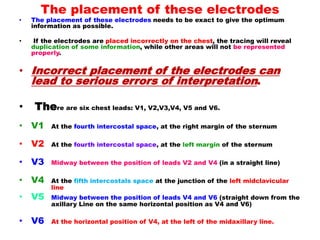
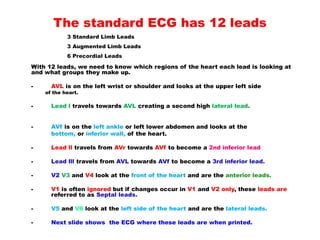
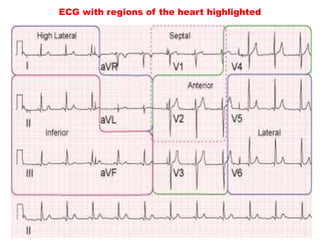
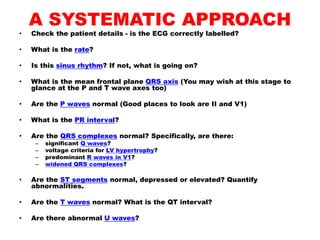
This document provides an overview of electrocardiograms (ECG), detailing the history, functioning, and interpretation of ECG readings. It explains the heart's electrical conduction system, the significance of various ECG waves (P, QRS, T, U), and the necessary arrangements of leads for accurate measurement. Additionally, it highlights the systematic approach for reading ECGs and the importance of correlating clinical findings with electrical activity patterns.