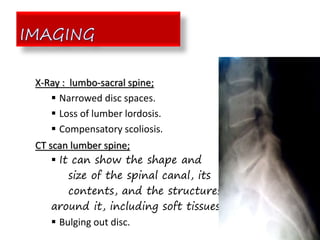
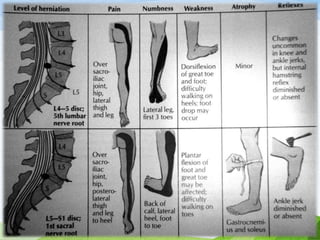
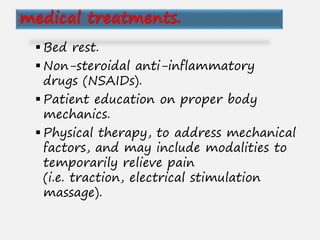
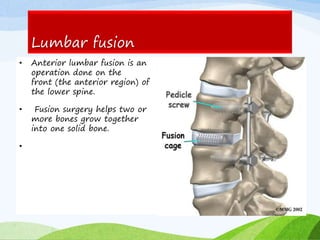
A herniated or prolapsed disc occurs when a tear in the outer ring of an intervertebral disc allows the soft inner material to bulge out. This most commonly affects the lumbar region. Symptoms include back pain and pain radiating into the legs. Diagnosis involves physical exam, x-rays, CT scans and MRI. Treatment options range from non-surgical approaches like medication, physical therapy and injections to surgical procedures like discectomy, laminectomy or spinal fusion. The goal of treatment is to relieve pressure on nerves and reduce pain.