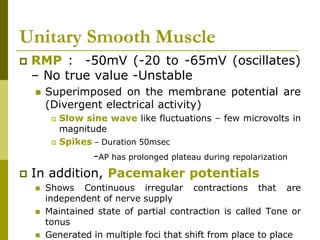
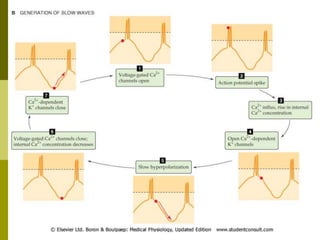
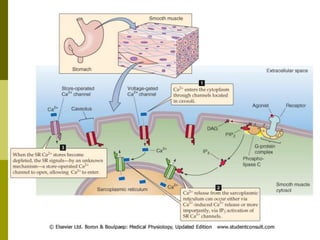
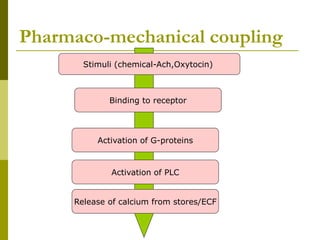
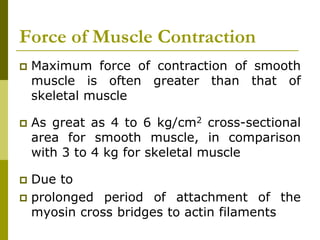
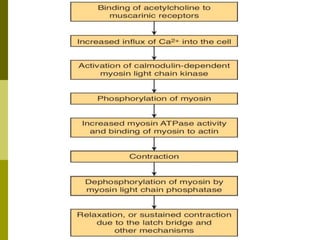
Smooth muscle lacks visible cross-striations and contains actin and myosin arranged irregularly. It contracts through calcium binding to calmodulin rather than troponin. Smooth muscle is either single or multi-unit. Single unit smooth muscle contracts as a syncytium through gap junctions and shows spontaneous rhythmic contractions. Multi-unit smooth muscle contracts through discrete localized contractions in response to nerve stimulation. Smooth muscle action potentials are driven by calcium influx and can include plateaus, producing prolonged contractions. Contraction results from calcium binding to calmodulin and phosphorylating myosin light chains, with relaxation through dephosphorylation.